Lichen planus (LP) is a chronic, long-term dermatosis of a multifactorial nature with diverse clinical manifestations and involvement of the skin, its appendages (hair, nails) and mucous membranes [1, 2].
Damage to the oral mucosa (OM) in LP can be combined with skin lesions, but is often isolated [3, 4]. Most often, the process develops on the mucous membrane of the cheeks, tongue, in the retromolar region, gums, lips, less often in the area of the floor of the mouth and palate. Mostly women aged 40 years and older are affected [5-7].
There are six clinical forms of LP of the red border of the lips and oral mucosa: typical, hyperkeratotic, exudative-hyperemic, erosive-ulcerative, bullous and atypical [3].
The clinical picture and course of LP on the oral mucosa has significant differences from its manifestation on the skin, in particular, greater resistance to treatment, which is due to the structural features of the mucous membrane, as well as the specificity of biological and physicochemical processes in the oral cavity.
The variety of clinical manifestations and the low effectiveness of treatment pose certain difficulties and interest not only for dentists, but also for dermatologists in terms of diagnosis and treatment of POPL.
The purpose of this work is to identify the clinical features of the manifestation of various forms of LP localized on the oral mucosa.
Lichen planus
Warts
7576 24 August
IMPORTANT!
The information in this section cannot be used for self-diagnosis and self-treatment.
In case of pain or other exacerbation of the disease, diagnostic tests should be prescribed only by the attending physician. To make a diagnosis and properly prescribe treatment, you should contact your doctor. Lichen planus: causes, symptoms, diagnosis and treatment methods.
Definition
Lichen planus is a chronic inflammatory disease of the skin and mucous membranes of unknown etiology. It is quite rare (according to WHO, 0.5% of all skin diseases) and, as a rule, occurs in people aged 45 to 60 years.
Causes of lichen planus
The causes of lichen planus still remain unclear. Experts classify it as a group of autoimmune diseases, when the body begins to produce antibodies that destroy its own tissues.
Provoking factors may include stressful situations, taking certain medications, possibly viral hepatitis C, or decreased immunity.
It has been noticed that patients with lichen planus are often characterized by increased excitability, suffer from insomnia and are prone to frequent mood swings. Some scientists believe that lichen planus is a delayed hypersensitivity reaction to various chemicals.
Proponents of the infectious nature of the disease talk about cases of the development of lichen planus after various injuries.
Classification of the disease
In patients with lichen planus, the following most common forms of skin lesions are distinguished:
- typical (the same type of rash in the form of papules),
- hypertrophic (warty rashes with indentations),
- bullous (blisters turning into plaques),
- actinic (large plaques, light at the edges and dark in the center),
- ring-shaped, or anular (rashes in the form of rings with raised edges),
- atrophic (nodules that rise above the skin and leave behind scars),
- pigmented (brown rashes merging into lesions),
- erosive-ulcerative (in addition to papules there are erosions and, less commonly, ulcers),
- follicular (pointed papules covered with dense horny scales).
Symptoms of lichen planus
In lichen planus, rashes appear on the skin, localized symmetrically on the flexor surfaces of the limbs, torso, as well as on the mucous membranes of the oral cavity, sometimes the esophagus, perineal area and anus; less often, nails, hair, palms, soles and face are affected.
Patients are bothered by itching, the severity of which depends on the form of the disease. The presence of papules on the oral mucosa causes discomfort; in the erosive-ulcerative form, bleeding of the gums is possible; there are complaints of dry mouth and pain when eating hot food. Ulcerative skin lesions in the erosive-ulcerative form are characterized by pain that intensifies during movement if they are located on the lower extremities.
In rare cases, the disease affects the nails. You can observe thinning of the nail plate, longitudinal grooves, splitting of the nail, discoloration of the nail plate and even its rejection from the nail bed.
Diagnosis of lichen planus
In most cases, the diagnosis of lichen planus is made based on the clinical picture. However, if patients have hypertrophic, atrophic, pigmentary, cystic, erosive-ulcerative and follicular forms, the typical elements inherent in this disease may be absent. To clarify the diagnosis, a biopsy of skin lesions is performed, followed by histological examination.
Before prescribing drug therapy, it is necessary to conduct laboratory tests, including a general (clinical) blood test, a general urinalysis, a biochemical blood test: AST, ALT, total bilirubin, triglycerides, cholesterol, total protein.
Material and methods
The study was carried out with the participation of 147 patients with various forms of LP of the oral mucosa, aged from 24 to 70 years, who sought advice from dental clinics at the Ural State Medical University and the Bashkir State Medical University.
The examination of patients with LP of the oral cavity included a thorough collection of anamnesis of this disease, clarification of hereditary predisposition taking into account previous diseases, identification of comorbid conditions and their relationship with the main one, the stages of manifestation of clinical symptoms of LP (periods of exacerbation and remission), allergic factor, and, if necessary, cytological and histological research.
When examining the mucous membranes, tongue and lips, attention was paid to the presence of signs of inflammation, elements of damage, and their location. An important diagnostic value is the presence of an isomorphic reaction in LP (Koebner's symptom), manifested by the appearance of fresh primary elements characteristic of this disease at the site of irritation of the skin or mucous membrane by any exogenous factor.
Routes of infection
More than 90% of the world's population are carriers of the herpes simplex virus. By the age of 30-40, almost 100% of people encounter it. Once infected with herpes, a person remains a carrier of the virus for the rest of his life. The infection is always transmitted from person to person, and the greatest probability of infection occurs during the acute phase of the disease, but it remains possible when it is asymptomatic. That is, you can get the herpes simplex virus from a carrier even if he does not have visible lesions on the skin and other symptoms of the disease. Type I herpes is found in saliva and other biological fluids of the body, so pathogens can be acquired through airborne droplets (by coughing, sneezing) or through household contact (by shaking hands, kissing, through shared utensils and hygiene items). A baby can also become infected with herpes from the mother while still in the womb, during childbirth, or while breastfeeding. With an adequately functioning immune system, some time after infection, the virus disappears from tissues and internal organs, but continues to persist in sensitive nerve fibers, making a person its lifelong carrier.
Publications in the media
Lichen planus (Wilson's lichen, true lichen) is a chronic itchy dermatosis of unknown etiology, characterized by the appearance of flat red polygonal papules with a smooth shiny surface and a slight depression in the center. Frequency. 450:100,000. The predominant age is 30–60 years.
Risk factors • Dental diseases, unsatisfactory condition of dentures contribute to the development of lichen planus on the oral mucosa • Exposure to drugs (gold preparations, aminosalicylic acid, tetracyclines) and chemicals (paraphenylenediamine compounds - reagents for color photographic and film films) • SLE • Emotional stress .
Clinical picture • Skin lesions •• Itching, often severe •• Flat, polygonal, brownish-bluish papules with a shiny surface, 1–10 mm in diameter. The rashes can merge, forming shagreen-like plaques covered with tightly packed scales. On the surface of some papules a peculiar mesh pattern is noticeable - the Wickham mesh, caused by uneven thickening of the granular layer of the epidermis (pathognomonic sign) •• Localization - the rashes are usually located on the flexor surface of the forearms, the anterior surface of the legs, the external genitalia; less often - on the dorsum of the feet, in the inguinal and sacral areas. There have been cases of generalization of dermatosis with the development of secondary erythroderma (erythematous form) •• Characterized by an isomorphic reaction at the sites of scratching (Köbner phenomenon) •• Depending on the clinical picture, the following forms are distinguished ••• Pigmented - flat papules are barely noticeable against the background of diffuse melasma ••• Erythematous - large itchy, swollen erythematous spots and papules, difficult to distinguish until the intensity of the erythema decreases; accompanied by general intoxication ••• Blistering (bullous) - blisters form against the background of papular rashes ••• Hypertrophic (warty) - large purple papules, often covered with horny layers, usually located on the anterior surface of the legs ••• Hyperkeratotic (horny) - on surfaces of papules - pronounced hyperkeratosis, localized on the legs ••• Coraloid - papules with a diameter of up to 1 cm in the form of beads of reddish-bluish color, alternating with areas of hyperpigmentation; usually located in the abdomen and neck ••• Atrophic - skin atrophy occurs in place of the papules ••• Dull (flattened) - large hemispherical, smooth, dense, low-itching papules are located on the legs, lower back and buttocks •• Depending on the location of the elements • •• Scattered single rashes ••• Linear rashes (lichen planus linear) - papules are located linearly, sometimes along the course of a nerve or along scratches ••• Ring-shaped rashes (lichen planus annulare) - papules are located in rings growing eccentrically, usually located on the trunk and mucous membranes. • Damage to the mucous membranes - in 40-60% of patients with skin lesions. In 20%, only the mucous membranes are affected. This condition is often considered as precancerous (the development of carcinoma is possible) •• The rash is painful, especially with ulceration •• Papular, often ring-shaped rashes of a whitish-pearly color in the form of a mesh, lace pattern, usually on the mucous membrane of the cheeks, less often - on the tongue, gums, the palate, on the red border of the lips - a continuous scaly stripe •• Depending on the clinical picture ••• The vesicular (bullous) form develops quite often ••• The erosive-ulcerative form with multiple erosions on the mucous membrane of the mouth and lips - the most severe form, may combined with diabetes and essential arterial hypertension (Grinshpan-Wilapol syndrome). • Damage to hair and nails •• Scalp ••• Lichen planus pilaris - rash of small papules around the mouths of follicles on the scalp ••• Skin atrophy and destruction of hair follicles, as a result of which persistent total alopecia may develop •• Nails - proximal formation - distal grooves and partial or complete destruction of the nail bed. The big toes are most often affected.
Research methods • Wickham's grid is better visible after local application of inorganic oils • Skin biopsy - inflammation with hyperkeratosis, thickening of the granular layer, uneven acanthosis, vacuolization of cells of the basal layer, hyaline bodies under the epidermis, heavy lymphocytic infiltration of the upper layers of the dermis • Serological tests to exclude syphilis.
Differential diagnosis • Secondary papular syphilides • Psoriasis • Atopic dermatitis • Leukoplakia (if localized on the mucous membrane) • Squamous cell and basal cell skin cancer • SLE • Erythema multiforme exudative • Exposure to chemicals • Rash due to drug allergies.
TREATMENT Management tactics • Clinical observation, especially of patients with the hypertrophic form of lichen planus, periodic examination of the skin • Timely detection and treatment of somatic diseases, functional changes in the nervous system, sanitation of the oral cavity, rational dental prosthetics (dental crowns must be made of the same metal) • PUVA therapy, heliocadmium laser therapy, inductothermy of the lumbar region (especially for generalized or intractable lesions). PUVA therapy is carried out periodically for 1–2 years • CBC, liver function tests, ANAT titer determination are carried out every six months • Anti-relapse therapy - repeated courses of vitamins, spa treatment • Due to the possibility of malignancy of ulcerative-erosive forms on the mucous membranes Regular monitoring by an oncologist is necessary.
General recommendations • A regimen with long sleep, rational employment with the exception of occupational factors that irritate the skin • Correction of the reaction to stress • For lichen planus of the oral mucosa, the exception of hot, hot, spicy and rough foods.
Drug therapy • For all forms of the disease •• Sedatives •• Penicillin preparations •• Vitamins (nicotinic acid, thiamine, pyridoxine, retinol) •• Histoglobulin 2 ml 2 times/week subcutaneously, per course - 8-10 injections • For skin lesions •• Locally - HA ointments (for example, triamcinolone 0.1%) •• Antihistamines (for example, diphenhydramine 25 mg every 6 hours) - to reduce itching • For lesions of the mucous membranes •• Retinol topically, tigazon 30 –75 mg/day orally (contraindicated during pregnancy) •• GC orally • For erosive-ulcerative and bullous forms - combined treatment •• GC (for example, prednisolone 20-25 mg every other day for 2-4 weeks) •• Chloroquine 0.25 g 1–2 times a day for 4–6 weeks •• Xanthinol nicotinate 150 mg 3 times a day •• Erosion of the oral mucosa is lubricated with a paste containing solcoseryl.
Complications • Malignant degeneration of long-existing hypertrophic, ulcerative-erosive lesions on the mucous membranes (1% of cases) • Alopecia • Nail destruction.
Prognosis • The disease has a benign, but long-term course, especially erosive-ulcerative forms • An individual therapeutic approach to the patient, taking into account pathogenetic factors, contributes to positive treatment results • Spontaneous resolution is possible within several weeks • A tendency to relapse is noted, especially against the background of emotional stress. A recurrent course is observed in 20% of cases, mainly in generalized forms. Prevention. Elimination of chemical factors and drugs that provoke lichenoid reactions, thorough sanitation of the oral cavity, reduction of stress.
ICD-10 • L43 Lichen planus
Treatment
For different forms of the disease, a different course of medications is prescribed. If the disease is asymptomatic, drug treatment may not be necessary. If erosions and ulcers have already formed, it is necessary to begin treatment as quickly as possible to avoid worsening the condition.
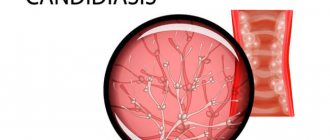
Inflammatory processes are controlled by the use of corticosteroids. Local treatment is carried out to relieve pain and accelerate tissue regeneration. To avoid the development of candidiasis, antifungal drugs are prescribed.
Electrophoresis and phonophoresis are also effective. In rare cases, when erosions do not heal for a long time, surgical intervention is indicated.
In all cases, without exception, the oral cavity is sanitized and the source of inflammation is removed (for example, periodontitis, caries or pulpitis).
Introduction
Lichen planus (LP) is a T-cell-mediated chronic inflammatory disease of skin and mucous membranes of unknown etiology. Dermatosis is characterized by a papular rash on the skin and most cases occur between the ages of 30 and 60 years. However, LP is increasingly observed in children. It may affect the mucous membranes, especially of the mouth and genitals, and very rarely, the mucous membranes of the anus, nose, larynx, conjunctiva and urethra. Lesions of the oral mucosa occur in 50-70% of patients with LP and may be the only manifestation in 20-30% of cases. However, skin lesions in oral LP were observed in 15% of patients. The estimated prevalence of oral LP (OCLP) ranges from 0.5 to 4% of the general population and is more common in women. The purpose of this study is to analyze the etiopathogenesis, clinical manifestations, diagnosis and treatment of OCPL.
Etiopathogenesis
Although OCPL is thought to be a T-cell-mediated autoimmune disease, its cause remains unknown. Current evidence suggests that the disease is associated with alterations in cellular immunity caused by endogenous or exogenous factors that result from altered responses to autoantigens. The majority of activated T cells in the inflammatory infiltrate of ACPL are CD8+. Activated T cells of the inflammatory infiltrate are associated with increased production of Th1 cytokines (IL-1, IL-8, IL-10, IL-12, TNF-α), increase the expression of intercellular adhesion molecules (ICAM-1) on Langerhans cells and macrophages. Other mechanisms that may also be involved in the etiopathogenesis of the disease are due to mast cell degranulation and activation of matrix metalloproteinases. Moreover, some researchers believe that the chronic course of OCPL can be partly explained by the insufficiency of immunosuppressive mechanisms mediated by transforming growth factor beta. However, the reasons that lead to the occurrence of the process have not yet been fully elucidated.
The relationship between OCPL and hepatitis C virus is not stable, as the prevalence of this virus in patients varies across studies, ranging from 0% to over 60%, depending on the country where the studies were conducted. The incidence of HCV infection in patients with LP is high in Japan, Italy and Brazil and low in the USA, France, Scandinavian countries, UK and Germany. The reasons for the difference in the prevalence of HCV infection in different geographical areas have not been clearly explained, but it is thought to be related to differences in socioeconomic status and subject selection (mean age and sex) in the respective countries. Despite this geographic heterogeneity, support for the hypothesis that certain genetic alterations may contribute to the development of OCPL in a subgroup of patients with hepatitis C is provided by the increased incidence of HCV in patients with OCPL. A recent meta-analysis of the literature concluded that HCV is associated with a statistically significant risk for the development of OCPL, suggesting that the presence of either HCV or certain types of OCPL may be used as predictive markers for each other in certain geographic regions. Thus, it is suggested that investigation of liver disorders or hepatitis C in patients with ACLP should only be performed in individuals with a suspicious clinical and epidemiological history.
Genetic polymorphisms of some cytokines also seem to be associated with clinical manifestations of the disease. Interferon polymorphisms have been associated with LP with isolated OCLP without skin eruptions, and TNF-α polymorphism has been associated with forms that affect the oral mucosa and skin. OCPL is a genetically determined disease. However, these findings need to be confirmed by studies conducted in different geographical areas.
A severe form of the disease, the so-called “vulvovaginitis-gingival syndrome” in LP, is thought to be associated with the HLA class II allele (HLA-DBQ1).
An interesting fact is the presence of rashes identical to LP in graft-versus-host disease (GVHD). The clinical and histological findings of oral lichenoid lesions in GVHD are indistinguishable from idiopathic OCPL lesions. In GVHD, T cells from the tissue donor attack the minor histocompatibility complex antigens of the host cells. Thus, GVHD represents an interesting model in studying the pathophysiology of ACPL.
Some authors have also shown that oral lichenoid reactions can result from contact with dental restorative materials, especially those containing amalgams, metallic mercury, or ammoniacal mercury. This can be proven in cases in which replacing these materials leads to an improvement in OCPL.
The association with psychological factors varies among authors. Two points are being discussed: 1) mental disorders (anxiety, depression) are involved in the genesis of the disease; 2) mental disorders (anxiety, depression) are a consequence of chronic pain lesions. In a study of 16 patients with OCPD without mental complaints and without a subjective need for psychiatric care, a psychiatric examination showed that 5 of them had moderate mental disorders and one had signs of “neurosis.” An association with depression has been reported by some authors and refuted by others.
Clinical manifestations
OCPL manifests itself in the following forms: reticular, atrophic, papular, erosive, bullous and erythematous. These different clinical manifestations represent variations in the intensity and duration of the disease. These different forms may coexist, and the predominant clinical morphology may change over time in the same patient. OCPL is often bilateral and symmetrical, which distinguishes it from contact lichenoid reaction of the oral mucosa. Unilateral lesions of OCPL are rare and atypical. The mucous membrane of the cheeks and gums, the back of the tongue, and the mucous membrane of the lips are most often affected. The gingival mucosa often appears in the form of "chronic desquamative gingivitis." OCPL can appear at sites of mucosal injury (koebnerization).
Mostly lesions in OCPL are represented by small whitish opalescent and keratinizing (scales sit tightly and cannot be removed with a spatula) papules. The lesions may have different patterns. Lesions in the posterior portion of the tongue tend to be more keratinized, isolated, or plaque-forming due to the specific features of the epithelium in that portion. As a result of prolonged existence, such rashes are prone to atrophy. Depapilation of the tongue caused by atrophy can lead to taste changes with a burning sensation when contacting certain foods.
In the erosive form, bright red, well-demarcated erosions are observed, surrounded by typical papules. Rarely, with a rapidly progressing course, blisters may occur. The pain is usually intense and can affect the patient's quality of life.
Lesions identical to those described above may also appear on the vermilion border of the lips and usually affect this area diffusely. However, they almost always do not extend beyond the border between the red border and the skin of the lips, unlike some other cheilitis.
Manifestations of the form of “desquamative gingivitis” are common and can occur in isolation or with lesions in other areas. There are painful erosions on the gums that make it difficult to brush your teeth.
In dark-skinned individuals, residual pigmentation of the mucous membrane (pigmented LP) is possible.
Damage resulting from a reaction caused by contact of mucous membranes with dentures containing metal is indistinguishable from idiopathic LP, except that they are distributed asymmetrically on the mucosa, in areas of the mucosa in contact with dentures. There is no correlation between the extent and severity of oral and cutaneous lesions in LP. Associated extraoral rashes in the scalp, nails, conjunctiva, esophagus, larynx, urethra, vagina, vulva and perianal area can lead to severe dermatosis. The combination of severe forms of oral and genital LP has recently been identified as “vulvovaginal-gingival syndrome”.
Several publications, especially articles in dental journals, have focused on the “precancerous” potential of OCPL lesions. Indeed, some studies have been conducted on this topic, but with inconclusive results regarding possible “risks of malignancy.” In our opinion, the development of squamous cell carcinoma in LP occurs only in very old atrophic-scarring lesions, but this is rare.
Unlike cutaneous LP, which in most cases occurs with short-term exacerbations and almost always responds well to treatment or regresses after several months, OCPL is characterized by a chronic, long-term persistent course and resistance to therapy.
Diagnosis
The diagnosis is established on the basis of clinical and histological examination. Histopathological manifestations include acanthosis (in keratinizing lesions), atrophy (in old lesions), and absence (erosive lesions) of the epithelium. There is a superficial lymphocytic inflammatory infiltrate at the junction of the epithelium with the lamina propria. Biopsy material should preferably be taken from keratinized areas to avoid erosion, since they lack epithelium, making microscopic examination difficult.
Direct immunofluorescence allows one to distinguish OCPL from other mucosal diseases with an inflammatory component, especially lupus erythematosus, erythema multiforme, and drug rash. Most often, with OCPL, the presence of deposits of IgM and, less often, IgA and C3 in the subepithelial layers is detected.
Differential diagnosis
Depends on the morphology of the lesions. Reticular papular lesions should be differentiated from discoid lupus erythematosus, candidiasis, morsicatio buccarum (mucosal defects due to the habit of gnawing the mucous membrane of the cheeks) and other traumatic injuries, spots of secondary syphilis, with leukoplakia and incipient squamous cell carcinoma. Erosive LP should be differentiated from aphthae, mucosal pemphigoid, pemphigus vulgaris, drug reaction, erythema multiforme and acute lesions of lupus erythematosus. Differential diagnosis of the pigmented form is made with several causes of mucous pigmentation.
It is sometimes difficult to diagnose LP gingivitis in the absence of rashes in other areas of the skin and mucous membranes. Lesions of the mucous membrane of the gums with pemphigoid, pemphigus vulgaris and OCPL can manifest as desquamative gingivitis. Therefore, it is very important to perform histopathological examination and direct immunofluorescence for a correct diagnosis.
Treatment
Treatment of OCPL should be aimed at relieving symptoms and minimizing the manifestations of dermatosis. There are no known effective treatments for all cases of OCPL, because its cause is unknown. Therefore, professional experience is important here. The extent of damage and severity of symptoms should be taken into account. Thus, treatment is individual for each patient. Isolated reticular papular lesions are asymptomatic and do not require treatment. Consequences are observed in atrophic lesions. Erosion damage requires drug therapy, because accompanied by severe pain.
It is important to adhere to the rules of oral hygiene, especially with periodontal disease, when gum lesions are present. Tartar and plaque can stimulate local inflammation and aggravate disease activity. Replacement of metal teeth is recommended if a reaction to these substances is suspected. Improvement occurs in areas close to metal teeth.
More often, strong topical corticosteroids are prescribed - mouthwashes, ointments or Orabase pastes, used 2-3 times a day. It is important to note that creams are never recommended for use on the mucous membranes of the mouth, and Orabase pastes are only used on intraoral lesions (moist surfaces). For lesions on the red border of the lips, ointments should be used. Systemic oral and intralesional corticosteroids are almost never used for exclusively intraoral manifestations of LP, with the exception of severe erosive forms.
The potency of topical corticosteroids and their frequency of use should be reduced when clinical improvement is achieved. Intraoral use of topical steroids is safe and well tolerated. The most common side effect is oral thrush, which can be prevented by prophylactic use of topical nystatin and preventing the patient from sleeping with dentures.
Erosive gingival lesions are especially resistant. A rational selection of dentures is necessary. Excessive application of potent corticosteroids to the gum mucosa can lead to tooth retraction.
Topical calcineurin inhibitors (TCIs)—tacrolimus and pimecrolimus—were introduced in the treatment of ACPL early in the last decade. They have a local immunosuppressive effect, are an alternative to TGCS for OCPL, and have shown interesting therapeutic results. 0.1% cyclosporine ointment and 1% pimecrolimus ointment are indicated. The ointment should be applied 2 times a day. Adverse reactions include burning and tingling where the ointment is applied. Systemic levels of pimecrolimus and tacrolimus were detected after application to the oral mucosa. The theory is that these drugs may increase the incidence of cancer in OCPL because in addition to acting on the immune system, they also act directly on cells. For example, according to Becker et al, tacrolimus appears to block several important intracellular signaling pathways, especially those associated with the p53 protein, whose mutation is present in some types of cancer. Therefore, the systemic absorption potential and malignancy of such agents support the need for further long-term evaluation of these drugs.
Some authors have reported the effectiveness of topical retinoids in the treatment of ACPL, especially when used in combination with topical corticosteroids for reticular or hyperkeratotic lesions. Recently, imiquimod has been used in a small number of cases. We did not use these drugs.
Some anti-inflammatory drugs commonly used in dermatology, such as levamisole, sulfones, griseofulvin and chloroquine, have been used by several authors with questionable results and without scientific basis.
Immunosuppressive therapies such as PUVA, methotrexate, azathioprine and mycophenolate mofetil may be attempted in very severe and refractory cases.
Some specialists have attempted CO 2 laser treatment, but in our opinion, the method lacks a scientific basis for such indications (laser is not used in the treatment of cutaneous LP).
Patients should be monitored periodically due to the need to gradually reduce the frequency and dose of medications and, especially, monitor atrophic-scarring lesions.
Individuals with comorbid psychopathology, especially symptoms of depression or anxiety, may require specialized care.
Causes of the disease
Lichen planus occurs under the influence of a number of factors, among which the most common is immuno-allergic. When the body's immunity decreases under the influence of external and internal factors, T-lymphocytes cannot cope with their protective function.
Factors that provoke the development of oral lichen planus include:
- Chronic stress;
- Strong shocks;
- Diseases of the gastrointestinal tract;
- Diabetes;
- Hypertension;
- Grynszpan syndrome;
- Injuries to the oral mucosa;
- Incorrectly installed dentures;
- Fillings that injure the oral mucosa;
- Prostheses made of dissimilar materials;
- Long-term use of tetracycline;
The risk group also includes patients whose work involves developing camera film or who come into contact with paraphenyldiamine.
Symptoms of the disease
There are six types of oral lichen planus. This is a typical, exudative-hyperemic, hyperkeratotic, erosive-ulcerative, bullous and atypical form. They are united by the formation of foci of inflammation on the oral mucosa, the appearance of defects and erosions. In some particularly severe forms of the disease, the patient may complain of itching and burning sensation in the mouth and difficulty eating. In milder forms, the disease may not manifest itself at all.
Typical lichen planus is the most common form, occurring in half of patients. White nodules appear on the mucous membrane of the oral cavity. Merging, they resemble lace.
The esscudative-hyperemic form is characterized by the appearance of gray papillomas on the edematous mucous membrane.
The hyperkeratotic form is one of the least common forms, which is characterized by the formation of gray spots that rise above the affected surface. Over time, these plaque spots become rougher and flake off.
Erosive-ulcerative is the most severe form of the disease, occurring in 23% of cases. Multiple erosions and ulcers covered with fibrinous plaque appear on the lining of the oral cavity. There is a strong burning sensation in the mouth, and when trying to remove plaque, bleeding and pain occur.
The bullous form is a relatively rare variety, occurring in 3% of cases. Accompanied by the appearance of dense blisters, inside of which there is hemorrhagic exudate. After the bubbles open, erosions form.
Atypical form - occurs slightly more often than bullous - in 4% of cases. This form is characterized by dilation of the mouth of the salivary gland, as well as inflammation of the lips and gums.
Quite often, one patient can develop several forms of lichen planus in parallel. Often one form can flow into another. Ringworm is a chronic disease prone to relapse.