Questions:
- What is pyoderma?
- Causes of pyoderma
- Symptoms
- Types of pyoderma
- How is pyoderma transmitted?
- Chronic pyoderma
- Pyoderma in children
- Pyoderma in newborns
- Treatment of pyoderma
- Is it possible to treat pyoderma at home?
- At what age can Timogen cream be used in children?
- Treatment with folk remedies
- Prevention
Medical specialists answer frequently asked questions from users
Causes
The etiological factor is bacteria - staphylococci and streptococci. There are pyoderma caused by other pathogens: Proteus vulgaris, pneumococcus, Pseudomonas aeruginosa, etc.
5 facts about the disease
- Pyoderma is the most common skin disease at any age, accounting for up to 40% of all skin diseases.
- Concomitant diseases often play a primary role in the occurrence of pyoderma.
- Almost all forms of infection are accompanied by purulent rashes.
- Pyoderma in newborns carries a high risk of serious complications.
- Opening ulcers (especially boils) on your own can aggravate the infection.
Features of pathogens
An important place in the pathology of humans in general and the skin in particular is occupied by Staphylococcus aureus and β-hemolytic streptococcus. The former widely colonizes the skin, especially at the mouths of hair follicles, sweat and sebaceous glands. The second, in smaller quantities, inhabits smooth skin, the area of natural openings and large folds. The disease develops according to the places of colonization. In this case, suppuration of the skin occurs due to the release of bacterial waste products (enzymes, exotoxins). Healthy, intact skin is a virtually impenetrable barrier to these microorganisms. Both external factors and diseases of internal organs can open the way for infection.
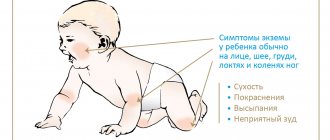
Figure 1. Pyoderma in children. Image: Artemida-psy / Depositphotos
External factors
There are many exogenous factors that help bacteria overcome the protective layer of the skin. Among them:
- Mechanical damage to the skin: abrasions, abrasions, cracks, diaper rash.
- Failure to maintain skin hygiene means contamination, improper care.
- Violation of the chemical composition of sweat, sebum, change in the acid-base state of the water-lipid film.
- Thermal effects on the skin: overheating, hypothermia.
- Exposure to chemicals, radiation.
- Maceration of the skin - soaking of the skin with liquid and swelling.
- Long-term use of antibacterial, cytostatic and, in particular, corticosteroid drugs.
Internal factors
Chronic diseases of internal organs and other endogenous causes are also often the cause of pyoderma. These include:
- Decrease in both general immunity and local immune status of the skin.
- Vascular diseases in which blood microcirculation is disrupted.
- Pathologies of the endocrine system: diabetes mellitus, hyperandrogenism, Itsenko-Cushing syndrome, etc.
- Diseases of the digestive tract and liver.
- Foci of chronic purulent infections.
- Conditions of hypo- and avitaminosis.
- Long-term, sluggish, severe illnesses, including HIV infection.
Pyoderma also complicates many dermatological diseases from the category of itchy dermatoses (eczema, scabies, atopic dermatitis and a number of others). This is due to damage to the skin as a result of scratching during itching.
How to relieve itching and prevent pyoderma?
- Cool the air in the room.
- During the hot season, you can sleep in slightly damp clothes.
- Itching will decrease if you are distracted by drawing, embroidery, knitting - using fine motor skills of your hands.
- You can apply ice or frozen foods wrapped in cloth to the itchy areas.
- It is recommended to use emollients that moisturize the skin.
Despite the large number of causes, pyoderma can be primary and occur on completely healthy areas of the skin.
What is pyoderma?
Pyoderma is a disease of purulent skin lesions, most often caused by pyogenic (pyogenic) cocci - streptococci and staphylococci, which are constantly found on the skin and mucous membranes. In addition to these pathogens, there are other microorganisms on human skin, such as pseudodiphtheria bacillus, yeast-like fungi, etc., which can also cause disease under certain conditions. The name of the disease comes from the Greek py'on - pus and de'rma - skin). This is one of the most common skin diseases.
to the begining
Risk factors
Risk factors include all of the predisposing conditions listed above, but special attention should be paid to the following:
- The presence of immunodeficiency. With a suppressed immune response, the slightest damage to the skin can cause a pustular infection. Under these conditions, they are also less treatable and are fraught with complications.
- Endocrinopathies. Hormonal imbalances can affect the composition of sebum, which can lead to excessive proliferation of staphylococci in the hair follicles and provoke pyoderma.
- Poor blood supply, especially in the extremities. This factor significantly increases the likelihood of severe acute and chronic streptostaphyloderma, coupled with chronic alcohol intoxication and/or hypothermia.
- Violation of sanitary and hygienic regime. An important factor, the prevention of which is available to everyone, nevertheless still remains relevant.
Is pyoderma contagious?
Some forms of pyoderma are highly contagious diseases. This especially applies to all types of streptococcal lesions. In this regard, it is advisable to avoid contact with patients, which is especially important for young children. Often, patients with pyoderma in the hospital are isolated from other patients.
External factors
The likelihood of the occurrence of the disease increases when the integrity of the skin is violated - ordinary and microtraumas, maceration of the skin.
External risk factors also include overheating or hypothermia of the body, increased sweating, contamination or alkalization of the skin, excessive or, on the contrary, insufficient hygiene. For example, overuse of antibacterial products destroys the natural protective barrier and beneficial bacteria living on the skin. Without protection, the cover becomes dry, cracks appear, and dysbiosis develops - this makes it easier for harmful bacteria to penetrate inside and cause inflammation.
Classification
The pyoderma group includes a large number of diseases that are classified according to several criteria.
For convenience, the classification is presented in the form of a table below. Table 1. Classification of pyoderma
| By origin |
|
| According to the depth of the lesion (form of infection) |
|
| By pathogen |
|
| With the flow |
|
Prevention of pyoderma
The first and most important rule for the prevention of pyoderma is timely antiseptic and antibacterial treatment of any wounds, cracks and microtraumas of the skin. Even habitual shaving causes microtraumas - pay special attention to the treatment of the skin and its daily care.
If you have diseases that increase the risk of developing pyoderma, treat them promptly in accordance with your doctor's recommendations.
If you already have a history of inflammatory skin diseases, do not forget about selective phototherapy and sanitation of focal infections. A detailed list of recommended procedures will be provided by a dermatologist.
Other articles by the author
- Pyoderma
- Herpes zoster
- Pityriasis rosea
- Shingles
Staphyloderma
With staphyloderma, the hair follicle and sweat glands are affected. The process is limited in nature and does not tend to spread and merge foci.
Folliculitis
Folliculitis is a purulent acute inflammation of the hair follicle. It is localized on the face, limbs, and torso; in men it often occurs after shaving. It usually begins with damage to the mouth of the follicle (ostiofolliculitis) and then spreads to the rest of it. Initially, redness and slight soreness occur around the hair, then a small abscess (pustule) matures. The surface of the pustule quickly dries into a yellowish crust.
The process can be isolated or multiple. Depending on the depth of the lesion, subjective sensations can vary: from mild to severe pain, from mild redness to severe perifollicular edema. Also, with multiple lesions, temperature and signs of inflammation may appear in a blood test.
Folliculitis completely regresses within 3-6 days (depending on the depth of the lesion). Typically, after infection, mild depigmentation (change in skin color) is observed, which quickly disappears. However, in cases of deep folliculitis, small scars may remain.
Patient with folliculitis. Photo: Indian Dermatology Online Journal / ResearchGate (Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported license)
Sycosis vulgar
Vulgar sycosis refers to chronic staphyloderma. It appears first in the form of multiple folliculitis in the area of beard and mustache growth, less often in the area of the eyebrows, pubis and armpits. Then the formations merge into a single lumpy surface with yellowish-red crusts on the surface. The hair in the outbreak is pulled out without effort, but does not fall out. Itching, tingling, some soreness or lack of subjective sensations are possible.
Furuncle
Furuncle is a deep purulent-necrotic inflammation of the hair follicle with damage to adjacent tissues. It can be single, occurring on intact skin, or multiple (furunculosis), complicating diabetes mellitus, vitamin deficiency and other conditions.
Furuncle. Photo: Mahdouch at French Wikipedia (Creative Commons Attribution 1.0 Generic license)
Appears on the face, buttocks, neck, hips, shoulders, first in the form of a painful, dense red swelling. The pain increases over 4-5 days, the color changes to bluish-red, and a pustule appears on the surface. The boil opens with the expulsion of a large amount of pus, after which a crater remains. Over time, it fills with connective tissue and a scar forms. The disease resolves within two weeks.
With a single boil, there are usually no general symptoms, however, with furunculosis, fever and changes in the blood test are possible.
Important!
Some localizations of boils, namely in the area of the nasolabial triangle and neck, are dangerous for the development of serious complications. Meningitis and thrombophlebitis of the venous sinuses are much more serious conditions than the boil itself. To avoid these consequences, it is important to seek help from a doctor and under no circumstances try to open the abscess on your own - this will increase the likelihood of complications.
Carbuncle
Carbuncle is a purulent-necrotic inflammation of several closely spaced hair follicles. At its core, these are several boils with a tendency to merge necrotic rods, therefore, before the formation of an ulcer, the course of the disease resembles furunculosis. As it matures, several pustules form on the surface of the skin against a background of general inflammation and swelling. Then they are also opened with the release of a large amount of pus.
Unlike a boil, the disease is always accompanied by fever, weakness and general inflammatory changes in the blood test. A deep ulcer with a red-black bottom appears in the affected area, in place of which a rough star-shaped scar is formed. Carbuncle usually does not appear on its own, but becomes a complication of immunodeficiency, diabetes and other conditions.
Hidradenitis
Hidradenitis is a purulent inflammation of the sweat glands with an apocrine type of secretion. These glands are located in the armpits, perineum, peripapillary, and perianal areas.
Hidradenitis often develops in the axillary region. Photo: Postgraduate medical journal / Open-i (CC BY-NC 3.0)
The disease begins with the formation of painful dense nodes in the thickness of the skin, which then soften, become cone-shaped and merge with each other. As the formation grows, the pain increases, fever, weakness and signs of inflammation appear in a blood test. The accumulated pus pours out through the fistula opening that forms in the lesion. The process ends with the formation of a retracted scar.
Hidradenitis occurs mainly in adolescence, since apocrine sweat glands function most actively at a young age. Statistically, girls are more likely to get it. Another name - “bitch udder” - the disease received due to the characteristic nipple-like protrusions of the resulting nodes. The use of antiperspirant deodorants increases the risk of hidradenitis.
Streptoderma
Streptoderma is less common, and the nature of the lesions in them is usually more widespread. The lesions often merge, and the resulting rash grows peripherally.
Streptococcal impetigo
Impetigo is a multiform disease characterized by the formation of many red spots, on the surface of which flat blisters (less than 1 cm) with cloudy contents then appear. This type of formation (phlycten) occurs in open areas of the body and is a typical primary eruptive element in streptoderma.
Soon the blisters break open, revealing an erosive, moist surface. The erosion discharge quickly dries out and turns into a yellowish crust, in place of which short-term depigmentation remains. The duration of the disease is usually no more than a week.
In addition to the classic one, there are other forms of impetigo, including:
- Streptococcal diaper rash - damage to large folds of the body (inguinal, axillary, etc.).
- Streptococcal infection - lesions appear in the corners of the mouth, causing severe pain.
- Bullous impetigo - develops in places with thick skin (hands, soles of feet), characterized by large dense blisters.
- Ring-shaped impetigo - characterized by a peculiar pattern of lesions in the form of rings due to the centrifugal growth of lesions.
- Syphilitic impetigo is localized in the genitals and buttocks, resembling a syphilitic rash in morphology.
- Periungual impetigo is a purulent inflammation of the nail fold.
- Dry streptoderma is an atypical variant of impetigo without conflicts, found in children.
Ecthyma
Ecthyma is a deep streptoderma, the lesion of which is represented by a large ulcer, reaching several centimeters. It is most often localized on the legs, less often on the thighs and torso.
The lesion initially appears as a single large phlyctena with purulent or purulent-hemorrhagic contents, around which the infiltrate grows and a red inflammatory border appears. The exudate turns into a thick crust, under which there is an ulcer with necrotic masses at the bottom. The latter heals with the formation of a rough scar. In total, the disease lasts 15-30 days.
Cellulite and erysipelas
Cellulite is a deep streptoderma affecting the skin and subcutaneous fat. The lower extremities are most often affected by infection. A characteristic symptom is increasing redness of the skin (erythema), and the affected area becomes painful and hot to the touch, its boundaries are blurred. Accompanied by fever, weakness, changes in the blood.
Erysipelas is characterized by a more superficial nature of the infection, but rapid progression and severe intoxication with a rise in temperature to 40°C, chills, headache and general malaise. The erythema is clearly demarcated from healthy tissue. Unlike cellulite, erysipelas often appears on the torso, face, neck, and chest.
Both infections are preceded by skin damage, surgery on the lymphatic vessels, and contact with carriers of streptococci. Flicktens and blisters may appear on the erythema, and complications are common.
Streptostaphylococcal pyoderma
Vulgar impetigo
Impetigo vulgarity in its clinical picture is very similar to the classic streptococcal impetigo described earlier, namely, it is characterized by conflicts on open areas of the body (especially on the face). The crusts formed after the opening of the blisters merge into single large yellow-brown plaques. The infection lasts about a week and goes away, leaving short-term depigmentation.
Chronic ulcerative-vegetative pyoderma
Ulcerative-vegetative pyoderma is characterized by the formation of a large ulcer, which occurs during the development of deep folliculitis, furunculosis or ecthyma. In the vegetative form, pathological tissue growths (vegetations) appear in the ulcer. A rim of redness forms along the periphery of the ulcer, on which new pustules and phlyctenas mature. The disease is accompanied by pain, insomnia, weakness and often becomes recurrent.
Chancriform pyoderma
Symptoms of chancriform pyoderma are similar to those of primary syphilis. Localized on the genitals, face and tongue. The lesions are pink ulcerative defects with clear boundaries, a dense base and purulent discharge. Lasts 2-3 months and ends with the formation of scars.
Symptoms depending on the type of disease
It is very difficult to highlight a small list of pyoderma symptoms. Manifestations of the disease will depend on the specific form.
- Impetigo. Water blisters appear on the patient's face and head (rarely on the body), and then they become yellow crusts, causing itching. Sometimes the color is greenish.
- Hidradenitis. This is inflammation of the sweat glands. Usually localized in the armpits, labia, perianal area, and groin. We are talking about the formation of a nodule with pus inside. There is no rod in the tumor, so it is different from a boil, but the formation is painful.
- Sycosis. This is pyoderma of the facial skin, which involves inflammation of the hair follicles. Affects the mustache and beard, lasts a long time, and often returns.
- Furuncle. And in this case, the follicle is affected, destroying adjacent tissues, a node is formed that hurts, and in its center there is a rod.
- Carbuncle. The formation resembles a boil, but spreads more strongly and can even reach the muscles. Because of this, there will be severe swelling, there is a risk of fever, severe intoxication. The carbuncle eventually becomes an ulcer, healing is accompanied by the formation of a scar.
- Ostiofolliculitis. Characterized by inflammation of the mouth of the hair follicle. It is a blister with reddened skin around it. After drying, a crust forms and then falls off.
- Folliculitis. Also inflammation of the follicle, but deeper. The abscess in the center is riddled with hair. The formation may simply resolve or form an ulcer, which after healing leaves a small scar.
These are just some of the options for skin pyoderma. There are also varieties that are found only in children.
Are you experiencing symptoms of pyoderma?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Pyoderma in children
In newborns and young children, the skin has different anatomical and physiological characteristics than in adults. This is explained by the underdevelopment of many systems, in particular the excretory and immune systems. In this regard, pyoderma in children has other clinical forms that are not found in adults.
The result of the vital activity of staphylococcus on the skin of a newborn baby. Photo: ResearchGate
Vesiculopustulosis
Vesiculopustulosis is a staphylococcal superficial pyoderma, a common occurrence in newborns. The disease is preceded by prickly heat, which arose as a result of overheating of the child. On the skin in the area of large folds, the torso, and on the head, following prickly heat (manifested by red spots and transparent blisters), blisters with white contents and redness around appear.
The infection lasts from 3 to 7 days, after which it disappears without a trace. However, when the infection spreads deeper, the pathogen may enter the bloodstream and damage internal organs, which poses a threat to the life of the newborn.
Multiple abscesses
Multiple abscesses (pseudofurunculosis) are a deep form of staphyloderma, in which infiltrative nodes the size of a pea appear on the skin. At the same time, the child’s temperature rises, appetite worsens, weakness appears, and the skin turns pale.
The disease is difficult to treat and can last up to several months. Severe purulent complications and sepsis are possible. The risk of complications is higher than that of vesiculopustulosis.
Epidemic pemphigus of newborns
Epidemic pemphigus of newborns is a contagious superficial staphyloderma. The infection is often acquired by medical personnel or the woman in labor herself through a poorly treated umbilical wound.
The disease is characterized by the formation of flaccid blisters up to 1 cm in size with a cloudy liquid, which after a certain time increase in size and open. After opening, erosions remain or crusts form, along the periphery of which new blisters appear. With a wide spread of rashes, an increase in temperature, refusal to eat, and tearfulness are observed.
In the best case, the infection lasts 2-4 weeks and goes away without a trace. But complications are also possible, including sepsis, which sharply worsen the prognosis.
Ritter's exfoliative dermatitis
Exfoliative dermatitis is considered a malignant form of epidemic pemphigus of newborns. The disease is characterized by the appearance of erythema, blisters, cracks and desquamation of the epidermis, resembling a 2nd degree burn in its clinical picture. The infection quickly spreads to the entire body, causing severe intoxication and damage to internal organs. It is the most dangerous pyoderma in newborns with a mortality rate of up to 50%.
Papulo-erosive and dry streptoderma
Both diseases are varieties of streptococcal impetigo. Papulo-erosive streptoderma occurs when the child is not properly cared for due to exposure of the skin to urine and feces. This is facilitated by the use of waterproof diapers, untimely change of linen and poor quality washing of clothes. The disease manifests itself in the area of the buttocks, perineum, thighs and scrotum in the form of bluish-red nodules. Subsequently, conflicts appear on the surface of the nodules, then erosions and crusts.
Dry streptoderma (lichen simplex) occurs with the formation of pinkish scaly spots on the skin of the back, buttocks, limbs and face (the most common location).
Both variants of infection proceed without a trace and are characterized by a good prognosis.
Are there any complications?
If the immune system is weak and the body is not provided with professional support, the disease will develop and there are risks of complications. In this case, these are inflammation of the lymph nodes, abscesses, scars, sepsis, meningitis, inflammation of internal organs and even thrombosis of cerebral vessels. That is, theoretically, things could lead to complications that would be dangerous not only to health, but also to human life. So the symptoms of pyoderma should never be ignored. This is not just an aesthetic problem. Moreover, against the background of the aesthetic factor, severe psychological conditions can develop, even depression - so this point also cannot be ignored.
Complications of pyoderma
Superficial forms of pyoderma can be complicated by transition to deep ones or become a gateway for the addition of another infection. In adults, their course is usually more favorable and there are fewer complications than with deep forms. The exception is erysipelas. Erysipelas can quickly develop into cellulite, subcutaneous abscesses with suppuration of fatty tissue and gangrene.
In children, with regard to superficial forms, the situation is somewhat worse. Due to an underdeveloped immune system, diseases such as exfoliative dermatitis or vesiculopustulosis can lead to pathogens entering the bloodstream (sepsis). With the blood flow, bacteria spread to literally every “corner” of the body, affecting vital organs: the brain, lungs, heart, kidneys. Caused secondary severe pneumonia and meningitis in children are associated with a very high risk of death.
Deep forms are often complicated in adults. The most severe complications are associated with the entry of pathogens and their waste products into the blood. For example, deep folliculitis or a boil in the area of the nasolabial triangle can provoke purulent meningitis and thrombophlebitis due to the entry of staphylococcus into the system of venous sinuses of the skull from the facial veins.
Causes of pyoderma
Frequent causes of pyoderma are hypothermia and overheating of the body under production conditions.
When the body cools, blood circulation is disrupted, swelling of the skin occurs, sebum secretion and sweating decrease, as a result, the skin becomes dry and flaky, making it easily susceptible to injury and infection.
Overheating of the body leads to loss of water and chlorides (mineral salts), the latter affecting the vascular system and the functions of the kidneys and skin.
The possibility of pyogenic infection can be increased by additional irritants like oils and other contaminants.
The skin is able to destroy microorganisms that fall on its surface due to the acidity of the skin (pH), the so-called “acid protective coat of the skin.” Bacterial infection occurs faster in those areas of the skin where the pH is higher - these are the armpits, interdigital folds of the feet, and inguinal folds. Therefore, pathological changes occur more often in these places.
to the begining
Diagnosis of pyoderma
Diagnosis of pyoderma is carried out on the basis of the clinical picture of the disease; there is generally no need for detailed specific tests.
When difficulties arise in diagnosis, for example, in the case of chancriform pyoderma, similar to syphilis, they resort to specific studies of the discharge for the presence of pale treponema (the causative agent of syphilis). They also resort to examining the discharge in severe deep and chronic pyoderma that requires antibiotic therapy. The material being studied is sown on special media, determining the specific strain of the pathogen and its sensitivity to antibiotics.
A blood test is always done, since there may be signs indicating a widespread inflammatory process. The level of these changes allows us to draw conclusions about the intensity of inflammation and concomitant diseases.
In case of pyoderma, the doctor must refer the patient for a blood test. Photo: megafilm / freepik.com
Diagnostics
To diagnose pyoderma, the doctor first examines the rash and determines its nature. Then the discharge from the purulent areas is examined under a microscope. If the tissue damage is very severe, a biopsy is often prescribed.
Additionally, the doctor may recommend a blood test to exclude diabetes, control leukocytes and ESR.
When making a diagnosis, cutaneous forms of tuberculosis and syphilis, as well as various fungal, parasitic and other skin lesions that are not related to pyoderma, are excluded.
Treatment of pyoderma
General points and treatment of superficial forms
First of all, when carrying out treatment, great attention is paid to skin care in and around the lesions. In case of localized forms, avoid washing the skin in the lesions and along the periphery, and in case of widespread rashes, washing is completely excluded. The hair in the affected areas is cut off, without resorting to shaving.
Unaffected areas of the skin are subjected to local treatment with disinfectants: an alcohol solution of salicylic acid, an aqueous solution of potassium permanganate, chlorhexidine, etc.
For superficial forms, priority in therapy is given to local treatment. An alcohol solution of salicylic acid, aniline dyes, local antiseptic and antimicrobial drugs are used. If necessary, open conflicts and pustules, washing them with a solution of hydrogen peroxide and lubricating them with the agents listed above. In case of common forms of infection, antibiotic ointments are applied.
Treatment of a boil. Photo: El Pantera / Wikipedia (CC BY-SA 3.0)
Therapy of deep and chronic forms of infection
In the treatment of deep forms, absorbable agents, enzyme preparations and healing ointments are used. Ulcerative lesions are treated with special dressings and ointments that accelerate the growth of the epithelium and ensure faster scarring of the lesion.
Antibacterial therapy with systemic drugs makes sense in the treatment of chronic forms of infection, the appearance of symptoms of intoxication (fever, weakness, signs of inflammation in the blood), localization of lesions in the area of the nasolabial triangle and with extensive purulent processes.
Immunotherapy plays an important role in the treatment of chronic forms of infection. They use neutralized bacterial toxins (anatoxins), hyperimmune plasma with ready-made antibodies, and medications that enhance nonspecific immunity.
In the case of sluggish, chronic infections, the treatment must also include B vitamins, vitamin C, and drugs that improve capillary blood flow.
Physiotherapy
Physiotherapeutic procedures improve reparative processes and local blood supply in the affected areas. The most promising methods include:
- UV irradiation.
- Dry heat.
- UHF therapy.
- Laser radiation.
- Water-filtered short-wave infrared radiation (wiRA therapy).
Physiotherapy is an auxiliary method of treatment and is used only as an addition to the main etiotropic and pathogenetic therapy.
Treatment
- Treatment in children
Treatment of omphalitis is carried out only by a doctor. In the initial stage, local use of medications is possible: washing the wound with a solution of hydrogen peroxide, treatment with brilliant green, iodine solution, methylene blue solution and various local antimicrobial drugs. Treatment of pyoderma in children involves the use of broad-spectrum antibiotics, infusion therapy, and immunomodulators. In the initial stages of pyoderma, it is possible to treat pyoderma with local means - solutions of boric and salicylic acids, sanguiritin, eucalymin, tomicide, cyminal and others in the form of solutions, lotions, under a bandage. See also our specialist’s answer to the user’s question: Pyoderma in children, how to cure it? - Treatment in adults
In adults, pyoderma is also treated by a doctor. For mild pyoderma, local medications are used (see above); for moderate severity, broad-spectrum antibiotics and sulfonamides are added to local treatment.To increase the body's resistance in the treatment of pyoderma, the immunomodulatory drug Thymogen is used. These are Thymogen cream, which is applied to the affected areas, and Thymogen solution for injection.
to the begining
Nutrition during an exacerbation
Nutrition plays an important role in the treatment of various forms of pyoderma. The basic principles of diet during an exacerbation of the disease can be described as follows:
- Meals should be regular.
- Complete in composition of proteins, fats, carbohydrates and vitamins.
- The amount of salt in food is sharply limited (up to 5 g).
- The amount of carbohydrates is reduced.
- Alcohol is completely excluded.
- Any products that can provoke allergies are excluded (for this, an allergy history is carefully collected).
- The drinking regime is controlled; it is necessary to consume at least 1.5 liters of liquid.
The diet includes low-fat fermented milk products; fresh vegetables, herbs; lean boiled meat and fish; durum wheat pasta; boiled eggs; olive and linseed oils; buckwheat grain; bran.
conclusions
Thus, Minocinclin
has a wide spectrum of antimicrobial action, high bacteriostatic activity against infections sensitive to it, a minimum of side effects and a convenient dosage regimen.
Consequently, the drug meets modern requirements for rational antibiotic therapy and can be recommended in clinical practice for the effective treatment of various clinical forms of pyoderma. Recommended course: the initial dose of Minolexin
was 200 mg (2 capsules of 100 mg or 4 capsules of 50 mg), then 100 mg (1 capsule of 100 mg or 2 capsules of 50 mg) every 12 hours (2 times per day).
Taking the drug does not depend on food intake. The duration of antibiotic therapy is 7 days, for erysipelas - 10 days. The drug has a good safety profile, which is confirmed by the absence of significant negative dynamics in clinical blood and urine tests and biochemical blood tests. Minocycline
is characterized by high lipophilicity and dermatotropism, allowing it to achieve optimal therapeutic concentrations inside the inflammatory elements of the skin and the absence of increased photosensitivity .
The authors declare no conflict of interest.
1e-mail 2e-mail
Prognosis and prevention
The prognosis depends on the form of pyoderma, existing concomitant diseases and the timeliness of assistance provided. With localized superficial forms, the prognosis is most often favorable. Deep and widespread superficial forms also respond well to treatment with adequate therapy and correction of concomitant conditions (diabetes mellitus, immunodeficiency, endocrinopathy).
The most unfavorable prognosis are erysipelas, furunculosis and severe pyoderma of newborns (for example, exfoliative dermatitis, multiple abscesses). These diseases are characterized by a high rate of progression and a high chance of generalization of infection. In addition to the above, the listed infections often occur against the background of diabetes mellitus, immunodeficiencies, malignant blood diseases and other conditions that are themselves difficult to treat.
Chronic infections, such as sycosis vulgaris, although not dangerous, greatly reduce the patient’s quality of life.
Prevention of pyoderma
Primary preventive measures against pyoderma come down to the following principles:
- Compliance with safety precautions at work with a high risk of skin injury.
- Timely treatment of skin injuries with disinfectants.
- Treatment of common diseases that are risk factors for the development of pyoderma (diabetes mellitus, diseases of the ENT organs, digestive tract, etc.).
- Therapy of other dermatological pathologies (atopic dermatitis, scabies, eczema, etc.), against which secondary pyoderma occurs.
- Compliance with hygiene standards and rules, especially when caring for infants.
How to properly treat injured skin?
When treating abrasions, scratches and cuts, you can follow the following algorithm:
- The affected area is washed with clean boiled or bottled water. You can first add a little liquid soap to a container of water.
- If the wound bleeds heavily, the affected area must be pressed with a cloth. It is better if it is a sterile bandage. Apply pressure to the wound for at least 5 minutes, without periodically removing the tissue to see if blood flows.
- After washing and stopping the bleeding, the wound must be treated with a disinfectant.
- If you only have alcohol solutions on hand (solutions of iodine, brilliant green), then you only need to treat them with the edges of the affected area. By no means the wound itself!
- Disinfectants such as chlorhexidine, miramistin, povidone-iodine can be used to treat both the edges and the wound itself.
- Next, depending on the size, you can stick a bactericidal adhesive plaster on the affected area or apply a gauze bandage, securing it with strips of rolled plaster.
Secondary prevention involves regular medical examinations, medical examinations, and anti-relapse therapy (special skin care, sanitation of foci of chronic infections, UV irradiation, prophylactic intake of vitamins).
Internal factors
The general condition of the body and immunity also affect the likelihood of pyoderma. Thus, the risk of developing the disease increases in the presence of endocrine diseases (for example, diabetes), obesity, diseases of the digestive or circulatory system, and severe somatic diseases.
Vitamin deficiency, reduced immunity, chronic intoxication, and hormonal disorders also serve as a favorable background for the development of pyoderma. In childhood, the risk of developing the disease is higher due to the structural features of children's skin and the functioning of the immune system.
If there are similar infections (for example, staphylococcal) in other organs, the likelihood of pyoderma caused by the same bacterium also increases.
Sources
- Skin and venereal diseases: textbook / ed. O.Yu. Olisova. - M.: Practical Medicine, 2015. - 288 p.: ill.
- Golub T.N. Pyoderma: informational and methodological letter for dermatovenerologists and general practitioners.
- Kukharik O. S. Modern features of the course of pyoderma // DVKS. 2011.
- Plieva Lina Rostislavovna On the treatment of superficial pyoderma // Russian Journal of Skin and Venereal Diseases. 2015. No. 1.
- Zverkova F.A. Pyoderma in young children // Regular issues of “RMZh” No. 11, 1997.
Symptoms of pyoderma
The manifestations of pyoderma depend on the causative agent of the disease and the affected area, which makes it difficult to identify a clear list of symptoms. However, if the following symptoms appear, pyoderma may be suspected and it is recommended to consult a doctor:
- inflammation of the hair follicles;
- inflammation of the sebaceous glands;
- the appearance of bubbles with liquid.
We recommend that you consult a dermatologist if any unpleasant, incomprehensible symptoms or manifestations appear on the skin.