About the disease
Another name for impetigo is superficial pyoderma, the frequency is about 15% of all skin diseases.
With proper treatment, no traces remain after recovery. Impetigo begins with the appearance of patchy redness (erythema) around the mouth and nose or on the extremities. Next, bubbles (vesicles) appear on the reddened skin, their contents are serous-purulent. After opening the bubbles, honey-yellow crusts form, which disappear after drying. The skin at the site of the crust remains pigmented for some time, but then this too goes away. Pain and itching are rare. Impetigo is caused by strepto- and staphylococci; the clinical manifestations of damage by these bacteria are somewhat different from each other. Streptococcal infection is typical for humid, warm areas and develops most often at the end of summer. There are no warning signs; bacteria multiply on initially healthy skin. Streptococcal bacterial carriage does not occur; the disease always develops.
Staphylococcal damage proceeds differently. Pathogenic bacteria remain on the skin for a long time in a dormant (latent) state. Therefore, the disease manifests itself either in the form of isolated cases, or reaches the frequency of an epidemiological outbreak (this is how neonatal pemphigus occurs). Epidemiological pemphigus occurs where there is crowding of people: in maternity hospitals, army barracks, boarding schools.
If Staphylococcus aureus is detected, the premises are closed and quarantine measures are carried out to stop the spread of infection. They treat both the sick person and everyone who came into contact with the patient.
In children, the dangerous age for infection is considered to be from 2 to 5 years. Contact sports and minor skin injuries increase the likelihood of the disease.
Impetigo is classified according to the type of pathogen:
- contagious (streptococcal);
- staphylococcal;
- mixed.
Within these large subgroups, several forms are distinguished. So, contagious impetigo has the following types:
- dry pyoderma, or lichen simplex - looks like pink spots on the face that immediately peel off, in their place the skin remains pigmented for a long time;
- bullous form - bullae (bubbles) up to 2 cm in diameter, filled with bloody-purulent contents, form on the limbs. The process affects the nails, after opening, rough (“greasy”) crusts form, the general condition suffers (body temperature rises, headache, other symptoms of intoxication occur);
- ring-shaped - first a bulla is formed, which opens in the center and begins to heal, and grows along the edges, and all together resembles a ring;
- jam (slit-like form) - occurs in those who often lick their lips, as well as on the wings of the nose and in the corners of the eyes. A crack forms at the site of the bubble, and the surrounding skin becomes inflamed. Heals poorly, lip and eye movements are interfered with;
- impetigo of the mucous membranes - blisters, followed by ulcers that appear in the mouth, on the tongue, inside the nasal passages, on the mucous membranes of the eyes;
- vegetative impetigo - blisters spread throughout the body;
- intertriginous streptoderma - blisters and erosions form in large natural skin folds, causing itching and pain;
- syphiloid-like form - found only in newborns, blisters form on the buttocks, subsequent erosions resemble chancre.
The most common form of staphylococcal impetigo is ostiofolliculitis, or inflammation of the mouths of the hair follicles.
It occurs when personal hygiene rules are not observed, especially in male adolescents. It occurs in the form of bullous (bubbles up to 5 cm) and non-bullous (up to 1.5 cm) varieties. A mixed form (vulgar or simple impetigo) develops when both types of bacteria are present on the skin. Itching and scratching are disturbing, rough thick crusts form, inflammation of the lymph nodes and symptoms of intoxication occur.
Thus, there are many clinical forms of impetigo. They have both common and distinctive symptoms. Therefore, if skin rashes appear, you should immediately consult a doctor. Making a diagnosis on your own is unrealistic and irrational. This only leads to delaying time and progression of the pathological process.
Etiology and pathogenesis
On human skin, streptococci and staphylococci are found as part of saprophytic microflora. In cases where, under the influence of any exo- or endogenous factors, the tension of the immune system is reduced and the barrier function of the skin is weakened, cocci turn into pathogenic forms: hemolytic and dermonecrotizing forms appear, which, under unfavorable conditions that provoke the occurrence of Impetigo (pollution and skin trauma, overheating) , cooling) cause disease. Among numerous endogenous factors, the main role belongs to the weakening of immune defense mechanisms, when a low titer of complement, antitoxin, decreased phagocytosis, weak activity of lysozyme and antihyaluronidase in the human body are combined with increased exposure to proteolytic enzymes produced by staphylococci and streptococci (hyaluronidase, plasmacoagulase, collagenase, proteinase and etc.). Metabolic disorders (hypoproteinemia, especially low levels of gamma globulins, hyperglycemia, hypocalcemia), insufficient activity of the pituitary-adrenal system, thyroid gland and gonads are important in the pathogenesis.
Adults who have had a sore throat are often carriers of cocci and a source of infection for the skin of children. Outbreaks of I. are observed in the family, as well as in children's institutions. I. often develops in children against the background of itchy dermatoses (neurodermatitis, eczema) as a result of skin infection during scratching.
Symptoms of impetigo
Inflammation caused by streptococcus manifests itself as small red blisters (up to 5 mm) with purulent contents. At first, the blisters are painful, but then the pain goes away, the blisters collapse and open, forming crusts. The whole process takes up to 2 months. Such vesicles can appear in any area of the body; the provoking factor is poor hygiene. The danger is the penetration of streptococcus into the blood and lymph, and from there into various organs with the development of myocarditis, nephritis, tonsillitis, rheumatism and even sepsis. Often, after streptococcal impetigo, panaritium develops - inflammation of the peri- and subungual bed. Staphylococcal impetigo is often localized around the hair follicles. Inflammation spreads deeper, causing the formation of ulcers, boils and even carbuncles. A lot of ulcers form at once; they cover almost all healthy skin. The lymph nodes react, become denser and hurt. Any type of impetigo is highly contagious.
Diagnosis
The diagnosis is based on a wedge, a picture, and is confirmed by laboratory research: the pathogen is detected when the discharge from the pustules is inoculated on nutrient media. Differential diagnosis of individual forms of I. is carried out with other types of pyoderma, syphilis, fungal diseases (Candidiasis, trichophytosis). It is often necessary to conduct a general examination of the patient to identify endogenous pathogenic factors that provoke and maintain the disease, as well as to identify possible complications.
Causes of impetigo
Pathogenic bacteria are everywhere; you can completely get rid of pathogens only through special treatment (sterilization), and then only for a short time.
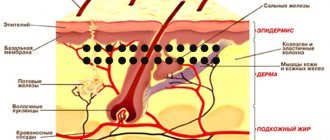
Even with daily hygiene procedures, transient flora and permanently resident bacteria are always present on the skin and do not cause infection. Under the slightest unfavorable conditions - prolonged wetness, untimely bathing, disruption of the sebaceous glands, scratches - bacteria instantly penetrate the dermis. The dermis immediately reacts to the invasion and inflammation develops. Various substances are released into the skin to destroy bacteria and restore integrity. The process ultimately ends with the cessation of inflammation and the formation of a scar, which gradually resolves.
Pathohistology
Both with streptococcal and staphylococcal varieties of I. the main element is the pustule, the edges develop directly under the stratum corneum. Pustule (see) contains fibrin, neutrophilic leukocytes and a certain amount of lymphocytes. In the pustule you can find groups of cocci located extracellularly or inside neutrophils. In the spinous layer under the pustule there is spongiosis (see), many migrating neutrophils. In the upper part of the dermis there is a slight inflammatory infiltrate consisting of neutrophils and lymphocytes.
Prevention of impetigo
The main prevention is good personal hygiene, frequent change of bed and underwear, individual sets in common areas (swimming pools, baths, trains). Children need to be taught hygiene skills as early as possible. Washing your hands after returning from a walk can prevent many skin diseases. Doctors at the SM-Doctor clinic are ready to help every child when the first signs of skin damage appear. At the first appointment, an individual treatment and prevention plan is developed so that the baby’s skin remains under the best protection for life. Contact qualified dermatologists at SM-Doctor!
Classification
There are several wedges, types of I. (according to etiology):
1. I. streptococcal, or streptogenic (syn.: Fox's impetigo, Jadassohn's impetigo, superficial streptoderma), including seven wedges, varieties: ring-shaped I., bullous I., slit-like I., I. vegetative, I. mucous membranes, syphiloid post-erosive papular I. and simple lichen of the face (syn. pityriasis alba).
2. I. staphylococcal, or staphylogenic (syn.: Bockhart’s impetigo, follicular I., superficial staphylococcal folliculitis).
3. I. streptostaphylococcal, or streptostaphylogenic (syn. vulgar I.).
The previously isolated pemphigoid form of streptococcal I. is the so-called. Pemphigus of newborns is classified as a disease of staphylococcal nature (see Pyoderma).
General information
Impetigo is a contagious skin disease, that is, it can be transmitted from sick individuals to susceptible objects (people, animals) through various transmission routes, for example, through direct contact. Refers to superficial pustular pyoderma and most often streptococci , followed by the possible addition of staphylococci .
The main manifestation of the clinical picture is non-follicular conflicts - superficial pustules in the substratum of the skin, and sometimes on the mucous membranes. Outwardly, they look like flat blisters, have a flabby, easily torn tire and an inflammatory halo of hyperemia .
Impetiginization can occur against the background of various types of dermatoses , eczema or scabies . The disease is very contagious and easily spreads in families and children's institutions - kindergartens, schools, cases of mass destruction are known.
Treatment
Patients with widespread rashes and general symptoms of intoxication are prescribed broad-spectrum antibiotics (oletethrin, albomycin, rondomycin, etc. are especially effective). The conflicts (bubbles) are opened, the erosions are treated with 1-2% solution of aniline dyes (brilliant green, gentian violet or 5-10% anthocyanin solution). To remove purulent crusts and have an anti-inflammatory effect, use 5% colymicin, dibiomycin, 0.5-1.5% erythromycin or 5% polymyxin ointments, 2-3% white mercury ointment, as well as creams and ointments containing corticosteroid hormones along with antibiotics: oxycort, geocortone, locacorten, dermosolone.
The duration of antibiotic use depends on the form of I. and its course. Sulfonamides are used less frequently. Etazol, norsulfazole and long-acting agents - sulfapyridazine and sulfadimethoxine (Madribon) - are prescribed. For long-term cases, specific and nonspecific immunotherapy is widely used: staphylococcal toxoid, staphylococcal antiphagin, staphylofiltrate, staphylococcal bacteriophage, strepto- and staphylovaccine, streptofibroantigen, gamma globulin, native plasma, autohemotherapy and blood transfusions. Among the general strengthening agents used are iron, phytin, rutin, ascorbic acid, vitamins A, B. The food of patients should contain an increased amount of proteins and vitamins; carbohydrates are limited, salty foods are excluded; The diet should include mainly dairy and plant products.
Forecast
in uncomplicated cases, it is usually favorable; with proper treatment and careful care of the child, complications are rarely observed. Timely treatment of complications also leads to recovery.