Sweating (hyperhidrosis) is a natural physiological process characteristic of all warm-blooded living organisms. It performs a number of vital functions: regulates heat exchange and maintains optimal water-salt balance. But heavy sweating is a symptom of one of the dangerous diseases.
How and why sweat occurs
The content of the article
When overheated, sweat glands begin to release fluid to the surface of the skin, thereby reducing body temperature. Water-salt balance is needed to maintain a constant level of electrolytes and ions in the intracellular fluid. Blood plasma also has a salt composition, but in a slightly different concentration.
The main regulator of sweating is the hypothalamus, a region of the brain that sends signals to various parts of the endocrine system, in particular the sweat glands.
Thus, with an increase in the concentration of salts in the blood plasma and a decrease in the volume of intercellular fluid (workout, visiting a sauna, staying in the sun), the signal is processed by the hypothalamus, which reacts by creating a feeling of thirst.
When body temperature rises, regardless of whether it is external influence (overheating) or internal processes (fever), thermoreceptors reflexively react to this and signal the hypothalamus. It activates the work of more than 2.5 million sweat glands, and they begin to secrete sweat-fat secretion.
What kind of sweating is considered normal: norms, smell
Normally, even at rest, women secrete about 500 ml. sweat, in men - 700-1000 ml. During illness, when body temperature rises, about 3000 ml of sweat is produced per day. Such losses must be compensated, otherwise unpleasant consequences will arise - dehydration.
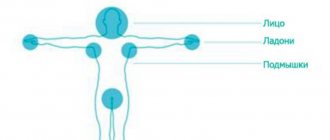
In addition to reactions to temperature, sweating is psychogenic in nature. Thus, apocrine glands located in the armpits, groin, and genital area are activated at the moment of emotional arousal, when an object of the opposite sex appears, during a quarrel or an increase in the emotional and mental background
The composition of the sweat from these glands is more concentrated, it contains enzymes that have a strong odor. However, it does not cause rejection, but carries genetic information. These are so-called pheromones, which help to choose a person who is suitable from a genetic point of view.
The unpleasant odor of sweat is due to the fact that the sweat of the subcutaneous sweat glands, eccrine glands, can destroy the keratin that covers the top layer of the skin. Microorganisms living on the epidermis begin to feed on softened keratin and multiply, releasing decay products. This is what causes the unpleasant odor.
It is especially active in the area of apocrine glands, so it is important to maintain hygiene standards. Usually, taking a shower or using wet wipes solves the problem of excessive sweating, but in some cases, hyperhidrosis becomes pathological and indicates serious problems in the body.
Hyperhidrosis - symptoms and treatment
Treatment of primary hyperhidrosis is carried out quite often and effectively, but due to the complexity of the initial diagnosis, patients often visit many different specialists in search of an adequate method of treating the disease.[22]
In general, it is more correct to talk about the need for a multidisciplinary approach to treatment with the involvement of a general practitioner, endocrinologist, dermatologist, neurologist, psychotherapist and surgeon.[12] The doctor’s experience, knowledge of the problem of hyperhidrosis and the possibilities of eliminating it are of primary importance.
How to treat hyperhidrosis
The following approaches can be distinguished in the treatment of hyperhidrosis:
- drug therapy;
- local effect on the source of increased sweating;
- surgical treatment.
Drug therapy
In the treatment of hyperhidrosis, systemic medications are used. It is possible to significantly reduce sweating with the use of oral anticholinergic drugs. In most cases, such systemic treatment is effective, but, unfortunately, due to the frequent development of side effects, long-term use of these drugs is rarely possible.
Among the drugs approved for use in the Russian Federation, oxybutynin . Its daily use in small doses (less than 10 mg per day) can reduce sweating with minimal development of side effects of the drug. You should start with 2.5 mg, gradually increasing the dosage to 10 mg.[1][4][28]
There are also numerous publications on the use of a drug such as glycopyrrolate (only the inhalation form of this drug is registered in the Russian Federation). According to the literature, this remedy is quite effective, although its use is accompanied by side effects.[11]
Among other things, some doctors recommend broad-spectrum drugs - benzodiazepines, amitriptyline, gabapentin, clonidine, verapamil, beta blockers. Their use makes sense if they are prescribed for an underlying condition. These drugs, as a rule, are not used exclusively for the treatment of sweating.
Local treatment
Local impact on an area of skin with increased sweating provides blockade of the problem area. There are several methods of such treatment.
Antiperspirants based on aluminum salts
This is the most common method of combating excessive sweating.[14]
The bulk of commercially available antiperspirants are absolutely useless for severe hyperhidrosis. In this case, only medical grade antiperspirants can help.
The effectiveness of an antiperspirant is determined by the concentration of aluminum salts (usually aluminum chlorides). At the initial stage, you can use a spray with a 10-12% concentration, but antiperspirants with a 15% concentration, as well as with 20%, 25% and 30% are most often used. Higher concentrations are very rarely used due to significant irritant effects on the skin.
The mechanism of action of antiperspirants: penetration of the active substance into the pores with the subsequent formation of metalloprotein plugs that prevent the release of sweat. The penetration process of the drug takes at least one hour after application, therefore the antiperspirant should be applied only at night before bed and only on dry skin. In the morning, the drug must be washed off.
IMPORTANT : The widespread advertising about applying antiperspirants in the morning after a shower is extremely incorrect. In this case, the sweat glands, active in the morning, will be further stimulated, and the sweat released will wash away the applied antiperspirant. Moreover, applying antiperspirant to a damp surface causes skin irritation similar to a chemical burn.
The effectiveness of treatment with antiperspirants is especially high for axillary hyperhidrosis. At the same time, you need to know that in the case of long-term treatment (3-4 years), atrophy of the sweat glands may develop, and, accordingly, a cure for hyperhidrosis. For mild forms of palmar and foot hyperhidrosis, this treatment can also be effective.
The popular literature often discusses the connection between the use of antiperspirants and the development of breast cancer, but there is no scientific basis for such a statement.
Iontophoresis (iontophoresis)
This physiotherapeutic method of treating primary hyperhidrosis is especially effective in cases of mild to moderate palmar and foot forms of the disease.[5][10]
Treatment is carried out in baths with plain water and aluminum electrodes placed at the bottom, through which a direct or pulsed electric current is passed.[14][16]
As a rule, procedures are carried out separately for arms and legs. They last 20-30 minutes. In total, 10-12 procedures are necessary to obtain the effect (preferably daily).
Once anhidrosis is achieved, the effect may last 2-3 weeks or longer, after which treatment is repeated. Another option to maintain the effect is preventive treatment every 4-5 days.
IMPORTANT : the method cannot be used if you have metal implants or cancer.
Botulinum toxin injections
This local method of getting rid of hyperhidrosis is effective for any localization of increased sweating (most often axillary).[10][14] Treatment consists of intradermal injections of the drug into areas of hyperhidrosis.
The action of the method is based on the absorption of the injected drug by the nerve endings, a fragment of which leads to blocking the release of acetylcholine.
Due to the speed, safety and high efficiency of the procedure, this method is now considered as the gold standard for the treatment of axillary hyperhidrosis. The duration of the effect is 6-8 months, after which repeated treatment is required.
Botulinum toxin injections are also effective for palmar hyperhidrosis, although they are used much less frequently due to the need to use higher doses. When treating this form, short-term weakening of the muscles of the thumb is possible (for 2-3 weeks), and therefore initial treatment is best carried out on one hand.
The method is less likely to be effective on feet with severe sweating, despite the use of high doses of the drug.
New methods of local treatment
New local treatments include microwave thermolysis of sweat glands,[25] radiofrequency microneedle therapy,[18] microfocus ultrasound and local hyperthermia.[15][22] All of them are applicable only for axillary forms of hyperhidrosis.
Local surgery
Local surgical treatment for hyperhidrosis in the armpits includes complete excision of the hyperhidrosis area, subcutaneous shaving, laser and suction curettage of areas of increased sweating.[2]
Excision is the most radical method. It is usually used when there is excess skin fold in the armpit area. It is highly effective, but is accompanied by a rather rough scarring process.
A lighter version is shaving - partial excision followed by visually controlled removal of the dermis layer.
Subcutaneous aspiration curettage can be considered a minimally invasive method. The operation is performed under local anesthesia. Instruments are inserted through a mini-incision to separate the axillary flap, followed by aspiration and curettage of the dermis until the skin flap is thinned. The method rarely leads to complete anhidrosis, but it significantly reduces the intensity of sweating.[29]
Treatment of hyperhidrosis with laser
Laser treatment for hyperhidrosis is used to eliminate axillary hyperhidrosis and is performed under local anesthesia. Exposure leads to damage to the sweat glands and a decrease in the severity or elimination of hyperhidrosis.
Contraindications for laser treatment of hyperhidrosis. The method has no side effects. Contraindications for laser treatment are intolerance to anesthesia and local inflammatory or scar processes. An acute inflammatory process is an absolute contraindication, scar changes are a relative contraindication, i.e. the procedure can be performed, but with certain technical difficulties or not always fully.
Surgical treatment
This approach to the treatment of hyperhidrosis involves surgical intervention on the sympathetic nerves - sympathectomy. There are two methods of endoscopic sympathectomy - thoracic (thoracic) and lumbar.
Endoscopic thoracic sympathectomy (ETS)[19][22]
ETS is the only permanent treatment for palmar and facial hyperhidrosis. The operation is one-step, performed in one of the following ways:
- removal of ganglia (sympathectomy);[17]
- intersection of the sympathetic trunk between the ganglia (sympathicotomy);[19]
- intersection of sympathetic communicating branches (ramycotomy);
- clipping of the sympathetic trunk is the only reversible method of influencing the sympathetic trunk.
The operation is performed with the patient in the supine position with arms apart under endotracheal anesthesia (it is also possible to perform the operation with a laryngeal mask):
- A telescope and instruments are inserted into the pleural cavity through incisions in the armpits;
- at the required level, the sympathetic trunk is isolated and processed;
- after the lung is expanded, the ports are removed and the operation continues on the other side (no drains are left).
The intervention may be hampered by previous chest surgery or severe pneumonia with pleurisy.
The duration of the operation in experienced hands does not exceed 15-20 minutes. Typically, the patient can be discharged from the hospital within a few hours. The effect of the operation is immediate: the palms become dry (as a rule, forever) and warm (lasts three months). After the operation, there may be a short-term resumption of sweating within a week, which quickly passes. When using 5 mm instruments, minor pain may occur, which also lasts no longer than a week.
Relapses of hyperhidrosis are possible in approximately 10% of cases. They are associated with activation of the overlying sympathetic ganglia, which were not affected.
Complications are unlikely (mostly occur when treated by inexperienced doctors):
- erroneous impact on similar structures (accessory nerves);
- damage to the stellate ganglion with the development of Horner's syndrome;
- injury to the intercostal nerve or branches of the brachial plexus.
IMPORTANT : Sympathectomy is not recognized by all doctors due to the potential risk of developing compensatory hyperhidrosis. In most cases, such hyperhidrosis still occurs both immediately after surgery and several months later. It manifests itself in the form of inadequate sweating of the torso below the zone of influence on the sympathetic trunk: the back, chest, abdomen are usually affected, and less often the buttocks, thighs and popliteal areas. However, compensatory hyperhidrosis is easily tolerated and, as a rule, occurs only in the hot season, during physical activity and less often during excitement.[7]
Because of this possible condition, the patient should be thoroughly informed about the risk of side effects from the operation.
Approximately 4-5% of patients consider compensatory hyperhidrosis as a more serious problem than the original sweaty palms, and therefore strive to return everything to the way it was. The latter is only possible with clipping, when during a repeat operation the clips are removed, and within 6-12 months it is possible to restore the original state. The likelihood of reversion is higher with early treatment after the first operation.
A more complex option for returning to the original state is the formation of a nerve insertion from the sural or intercostal nerve. The most promising is considered to be reconstruction of the trunk using a surgical robot.
Endoscopic lumbar sympathectomy (ELS)[21][22]
EPS is the only permanent treatment for foot hyperhidrosis. It is less common due to its technical complexity, and also due to the fact that treatment is resorted to only in extreme cases, when the level of hyperhidrosis can be described as catastrophic - constantly wet feet to the point of visible streams of sweat.
The operation is performed under general anesthesia sequentially on both sides:
- a retroperitoneal cavity is created using an expander balloon;
- a video camera and two manipulators are introduced sequentially;
- the sympathetic trunk stands out and overlaps at the level of 3-5 lumbar vertebrae;
- the operation is repeated on the other side.
The effect of the operation is immediate.
Potential complications:
- risk of damage to the genitofemoral nerve, which leads to a feeling of numbness in the inner thigh;
- development of lymphocele - accumulation of lymph in tissues (rare).
Specific complications include postsympathectomy neuropathy. This condition develops 7-10 days after surgery and occurs in the form of pain of varying intensity in the lower abdomen, thighs and legs. This complication is observed in approximately 30% of those operated on, and most often it goes away on its own. Isolated cases of long-term persistent course of neuropathy have been described, which should be reported to patients in advance.
Information about the undesirable effects of surgery on the male genital area has not been confirmed.
As with thoracic sympathectomy, lumbar resection of the sympathetic nerve may be accompanied by increased general body sweating, but to a significantly lesser extent than after thoracic sympathectomy.
Choice of treatment method
The choice of treatment method depends on the location of the hyperhidrosis zone, its severity and the likelihood of developing side effects.
Axillary hyperhidrosis:
- antiperspirants - start with 15%, if ineffective, increase the concentration;
- botulinum toxin injections;
- local methods of physiotherapy and any of the new treatment methods;
- local surgical methods;
- sympathectomy - exclusively for a combination of palmar and axillary hyperhidrosis.
Palmar hyperhidrosis:
- antiperspirants - immediately start with 25-30%, the effect can be expected only with mild forms of hyperhidrosis;
- iontophoresis - for mild and moderate hyperhidrosis;
- botulinum toxin injections - help with any severity of hyperhidrosis, however, with a severe degree, increased doses are required, and the duration of the effect may be insignificant;
- endoscopic thoracic sympathectomy - helps with any degree of hyperhidrosis, but is most justified in severe cases.
Foot hyperhidrosis:[26]
- absorbent insoles and frequent changes of shoes - for mild forms of hyperhidrosis;
- antiperspirants - immediately start with 25-30%, the effect can be expected only with mild forms of hyperhidrosis;
- iontophoresis - mainly for mild and moderate hyperhidrosis;
- botulinum toxin injections - help with any severity of hyperhidrosis, however, with a severe degree, increased doses are required, and the duration of the effect may be insignificant;
- endoscopic lumbar sympathectomy - helps with any degree of hyperhidrosis, but is most justified in severe cases.[21]
Hyperhidrosis of the face and scalp:[23]
- therapy with systemic drugs - especially when sweating of the scalp predominates and hyperhidrosis occurs in adulthood;
- antiperspirants - no more than 10-12% due to the risk of skin irritation;
- botulinum toxin injections - only in the forehead and carefully in the perioral area due to the risk of blocking facial muscles;
- endoscopic thoracic sympathectomy - helps with any degree of hyperhidrosis, but is most justified with severe degrees (the risk of severe compensatory hyperhidrosis is higher than with surgery for palmar hyperhidrosis).
Perineal hyperhidrosis:
- therapy with systemic drugs;
- antiperspirants - start with 15%, if ineffective, increase the concentration;
- injections of botulinum toxins - after a detailed determination of the boundaries of hyperhidrosis and subject to careful administration in the perianal area.
Treatment of hyperhidrosis with folk remedies
Traditional medicine is a method whose effectiveness and safety have not been scientifically proven, so their use may be useless or cause harm to health.
Care at home
To reduce hyperhidrosis at home, you can use aluminum chloride antiperspirants.
What does increased sweating indicate?
Hyperhidrosis is not always a pathology. Sweating affects obese and overweight people, women in the premenopausal period, and teenagers. There is nothing abnormal about this. Men sweat 2 times more intensely than women, people with African roots have a genetic predisposition to hyperhidrosis, and in summer the intensity of sweating increases regardless of gender and age.
Professional athletes who train 5-6 hours a day, even after taking a shower and completely changing clothes, continue to sweat intensely for some time after physical activity, and this is not a deviation from the norm.
Some people don’t see anything wrong with sweating; it doesn’t irritate them, although those around them suffer from it.
We should talk about pathology when the problem not only interferes with the person who has it, but also affects social connections. Sweat has a rather complex composition, which includes lactic and uric acids, ammonia, and various salts. As a result of exposure to the epidermis, bacteria are activated, which feed on softened keratin particles. This is precisely the reason for the specific vinegar smell of sweat.
In principle, it is enough for a healthy person to regularly change his underwear and take a shower daily so that the unpleasant smell of sweat is not heard. Apocrine glands secrete a substance with an individual odor depending on health, age and fertility.
In unhealthy people, it becomes intense and repulsive to others. Moreover, standard preventive measures (changing underwear, using antiperspirants, showering twice a day) do not bring any results.
Sweating for no apparent reason indicates pathological processes in the body, among which there are life-threatening pathologies. In particular, hyperhidrosis is characteristic of impaired hemostasis - the optimal level of hormones. This happens when there is a malfunction of the hypothalamus, a small area of the brain that controls the endocrine system.
The most famous example of disturbances in the functioning of the hypothalamus is menopause - the attenuation of a woman’s reproductive functions. During this period, the hypothalamus sends incorrect signals, the endocrine systems experience disruption and react with involuntary activation of the sweat glands - the so-called hot flashes.
In addition to menopause, hyperhidrosis occurs in case of other disorders.
Increased sweating in thyroid diseases
Sweating is characteristic of hyperthyroidism, characterized by an increase in the production of thyroid hormones and the development of intoxication.
In addition to increased, causeless sweating, symptoms of hyperthyroidism include:
- sudden weight loss
- drowsiness
- swelling in the neck area
- tachycardia
- irritability and nervousness
- diabetes. Under the influence of sugar in the blood, blood vessels and nerve connections are destroyed, but not throughout the body, but only in certain areas. The scalp, arms, neck and chest sweat especially heavily in diabetes.
Sweating is also characteristic of hypoglycemia - a lack of glucose in the blood. This is caused by an increase in adrenaline levels, which is activated when there is a lack of sugar.
Botox for the treatment of hyperhidrosis of the head and face
The Botox injection procedure in our clinic is performed by experienced cosmetologists. This procedure does not require special preparation; it is only important that there are no areas of inflammation on the face, neck or under the hair.
The doctor makes several injections in the areas of the most severe sweating of the head or neck: the needle of the syringe is so thin that the procedure does not even require additional anesthesia, the patient experiences virtually no discomfort. Immediately after the procedure, you can return to your normal lifestyle; no additional rehabilitation is required.
The pronounced effect of Botox injections will be noticeable already on the 3-4th day and will last up to 8 months, then the procedure will need to be repeated.
Pheochromocytoma - sweating due to adrenal tumors
Pheochromocytoma is a tumor of the adrenal gland that stimulates the production of catecholamines - adrenaline and norepinephrine. The disease is characterized by crises, during which panic attacks, tachycardia, nausea, gag reflex, and increased sweating are observed.
The attack is impossible not to notice, because it is accompanied by impaired cerebral circulation, trembling in the body and pulmonary edema. It lasts 2-3 minutes, but is extremely stressful for a person.
In the absence of an adrenal tumor, an increase in catecholamines is caused by heart disease, alcohol withdrawal, and refusal to take certain medications.
Ovarian dysfunction
The pathology occurs in every 10th woman of reproductive age. This may be an ovarian cyst, but polycystic disease often occurs - a complex disease in which ovulation does not occur and the follicle begins to grow. Over time, the ovary becomes like a bunch of grapes due to the many cysts that form.
Hormonal imbalance and lack of female sex hormones lead to increased production of testosterone, the male sex hormone. It increases metabolism, causing increased sweating.
It is also promoted by autonomic disorders, accompanied by irritability, aggressiveness, and sleep disorders. Symptoms of ovarian dysfunction, in addition to sweating, are menstrual irregularities, weight changes, deterioration in health, increased hair growth, etc.
Classification
The difficulty of identifying individual variants of excessive sweating is due to the great subjectivity in assessing symptoms. Depending on the frequency of occurrence, hyperhidrosis is classified into permanent, the severity of which does not depend on the time of year, seasonal, in which sweating increases in the hot months, and intermittent, characterized by periodic relapses. In clinical practice, the classification of symptoms by prevalence is important, according to which they distinguish:
- Limited (local) hyperhidrosis
. Characterized by increased secretion of sweat glands in certain areas of the skin. In accordance with this, the local form is divided into facial, palmar, plantar, axillary (axillary) hyperhidrosis. This variant is more often associated with dysfunction of the apocrine glands. - Generalized hyperhidrosis
. Increased sweating is observed over the entire surface of the skin. The development of this disorder is due to the increased work of all sweat glands, which is often associated with changes in hormonal levels, infectious diseases, and other systemic pathological disorders.
Various pathogenetic mechanisms determine the division of pathologically increased secretion of sweat into two forms: primary idiopathic, the causes of which have not been established, and secondary, caused by damage to different organ systems. Night sweats associated with chronic infectious processes or hormonal fluctuations are classified as a separate type. Due to a special development mechanism, doctors distinguish stress sweating (the so-called “cold sweat”), provoked by an increased concentration of catecholamines (adrenaline) in the blood. Taking into account the degree of social discomfort, there is:
- a mild form of sweating that does not limit the patient’s interaction with other people;
- moderate hyperhidrosis, in which daily activity is somewhat limited and discomfort occurs when shaking hands or close contact with people;
- a severe form, characterized by heavy sweating with a pungent odor, which forces the patient to avoid other people and provoke psychological disorders.
Sweating and central nervous system diseases
The autonomic nervous system is controlled by centers in the medulla oblongata and spinal cord, and the center is located in the hypothalamus. Ganglia, sympathetic nerve ganglia, are located near the spine, and nerve impulses emanating from them travel along nerve fibers to various parts of the body. If there is a disturbance in the functioning of the central nervous system, increased sweating occurs, regardless of the cause of the malfunction.
But this is only a secondary sign, indicating more significant symptoms:
- with Parkinson's disease,
a person's hands and head shake, muscles have increased tone, and their gait changes; - a stroke
is characterized by speech impairment, changes in facial expressions, and severe headache; - with epilepsy,
a person experiences convulsive seizures, during which hyperhidrosis occurs due to severe overexertion; - with a concussion,
loss of consciousness, nausea, and perspiration may appear on the forehead; - injury to the hypothalamus
manifests itself not only by increased sweating, but also by pressure surges, vascular problems, and sleep disturbances; - hormonal changes.
Teenagers tend to sweat a lot. This is due to a sharp hormonal surge, as well as intensive development of the whole organism and an increase in the functioning of most glands. There is nothing pathological about this, but sweating can cause discomfort for a teenager.
Treatment
Help before diagnosis
To reduce the discomfort from increased sweating, it is necessary to observe hygiene standards and avoid wearing hats made of synthetic materials. It is advisable to exclude hot and spicy foods and alcohol from the diet, which often increase sweating. To eliminate symptoms during public speaking, you can use sedatives of herbal origin. In case of local cranial hyperhidrosis, you should consult a specialist to identify the cause of unpleasant manifestations and choose the optimal treatment tactics.
Treatment of scalp hyperhidrosis with botulinum toxin
Conservative therapy
If the disease that causes excessive sweating is determined, the symptoms disappear after the cause is eliminated. In the acute period of injuries and neurological diseases, therapy is aimed at correcting vital functions and restoring the functional capabilities of the body, and the elimination of increased sweating is carried out by symptomatic means. When sweating is combined with erythrophobia, psychotherapeutic methods are effective. For the medical treatment of scalp hyperhidrosis, the following pharmaceuticals are used:
- Anticholinergics
. Drugs from the atropine group selectively inhibit the activity of neurons of the sympathetic nervous system, due to which sweat production decreases. Medicines are taken orally or administered intravenously. - Sedatives
. For moderate hyperhidrosis, herbal and synthetic sedatives are effective. If your scalp sweats a lot, you may need light “daytime” tranquilizers that do not affect performance. - Local agents
. Use rubbing the skin with aluminum chloride hexahydrate, which is diluted in alcohol. In some patients, local iontophoresis with saline solutions and anticholinergics is effective. - Antiparkinsonian drugs
. For increased sweating caused by Parkinson's disease, specific medications are prescribed that affect the metabolism of dopamine in the brain. Treatment is carried out in long courses. - Antihypertensive drugs
. To quickly relieve a hypertensive crisis, loop diuretics and beta-blockers are administered. In the future, an individual treatment regimen for hypertension is selected to prevent exacerbations. - Botulinum toxin
. If other drug methods are ineffective, intradermal administration of the drug is recommended. The drug allows you to reduce the number of nerve impulses entering the sweat glands, and thereby reduce sweating.
Surgery
Hyperhidrosis of the head and face, refractory to conservative treatment measures, requires surgical interventions. Most often they resort to endoscopic sympathectomy (destruction or clipping of the sympathetic trunk), which is aimed at reducing the functional activity of the sweat glands. To eliminate the consequences of severe TBI as the leading cause of hyperhidrosis, removal of intracranial hematomas for decompression of brain structures is indicated, and, if necessary, repositioning of bone fragments is carried out.
Sweating during menopause and pregnancy
In women before menopause, the levels of progesterone and estrogen decrease and the amount of FSH increases. This is a rather long process; menopause does not occur in one day. Several years before the onset of hormonal changes, a woman feels changes at the physiological level: her body odor changes, she sweats more often, quickly gains weight and has difficulty losing it.
Gradually, the level of female sex hormones falls, and male sex hormones (androgens) are produced more than during the fertile period.
Sweating is not the biggest problem; it only indicates irreversible changes in the body. If a woman notices an unusual increase in sweating, she should contact an endocrinologist. The doctor will conduct all the necessary tests and prescribe hormone replacement therapy.
Also, increased sweating often occurs in pregnant women, especially in the 1st trimester. The reason is a sharp restructuring in the body caused by implantation of the embryo to the wall of the uterus. The hypothalamus actively stimulates the production of progesterone, while other hormones are produced in smaller volumes.
A characteristic feature is sweating of the feet, regardless of the intensity of physical activity or its absence. At the same time, in other parts of the body, dehydration and dry skin occurs, even to the point of peeling. This is not a pathology, and by the 2nd trimester, local hyperhidrosis appears much less pronounced.
Where did hyperhidrosis come from?
Sweating of the head occurs due to external and internal reasons. In a person with this symptom, it is worth studying:
- is he dressed for the weather (maybe he’s just hot);
- whether its actions are active (during physical activity there is a physiological increase in sweating;
- emotional state (during stress, sweating increases under the influence of neurotransmitters);
- Is your hair clean (sebum accumulates, creating a “greenhouse”);
- what material is the headdress made of (synthetics do not dissipate heat well and almost do not absorb sweat);
- Are there any styling products on the hair (if used frequently and poorly removed from the skin, they provoke increased sweating).
Read also: Headache in the forehead area
If there are no external causes, they move on to looking for problems from within. Factors that cause your head to sweat:
- prolonged stress;
- frequent drinking of alcohol;
- smoking a large number of cigarettes (more than 2 packs per day);
- increased anxiety;
- eating large amounts of spicy and fatty foods;
- hormonal disbalance;
- taking certain pharmacological drugs.
If none of the reasons apply, you should visit a doctor. Sometimes sweating of the head is a symptom of a serious pathology that requires treatment.
Cardiovascular disease and sweat
They are also characterized by hyperhidrosis caused by activation of the central nervous system. Other symptoms, depending on the disease, include the following:
- for hypertension: increased blood pressure, increased heart rate, tinnitus, headaches, numbness of the hands;
- with coronary heart disease: pain behind the sternum (angina pectoris), inability to take a full breath, nausea and very profuse sweating;
- during myocardial infarction, perspiration covers the entire body, a feeling of fear arises, blood pressure drops, and the person feels very severe pain in the heart area;
- hyperhidrosis with thrombophlebitis occurs in advanced forms of blockage of the vein lumen;
- tachycardia occurs as a reaction to stress or fear, while a person’s adrenaline level increases, the body becomes covered in perspiration, and it becomes difficult to breathe. With tachycardia, there is heat in the head, but the hands remain cold;
- with vegetative-vascular dystonia, sweating is a reaction to stress, even the slightest one.
But with this pathology, the body mobilizes regardless of the reality of the situation. Often a person suffering from VSD experiences bouts of sweating and panic attacks completely unexpectedly: in the subway, in a crowd or in a quiet environment. In this case, hyperhidrosis is a side reaction to imaginary or real stress.
Causes of sweating head
Emotional turmoil
The symptom often develops in stressful situations, with fear. Patients prone to emotional lability report that severe sweating of the head and face occurs during public speaking, taking exams, and important interviews. Sweating can be so profuse that sweat runs down the skin in streams. The face and ears also become very red, and there is a disturbing feeling of heat and a rush of blood to the head. Such symptoms cause severe psychological discomfort, which is why patients try not to attract attention to themselves and avoid new acquaintances, which leads to social maladjustment.
Nightmares
Unpleasant dreams are common causes of scalp hyperhidrosis, especially in children. The patient sleeps restlessly at night, tosses about in bed, and screams. In this case, profuse sweating is observed, especially pronounced in the facial area and scalp: hair may become wet, and wet spots form on the pillowcase. After awakening, a person does not immediately become aware of the surrounding reality; for some time he is in a state of severe fright. If nightmares persist for several nights in a row and are accompanied by a fear of falling asleep, you should seek medical help.
Vegetative-vascular dystonia
Disturbances in the coordinated work of the sympathetic and parasympathetic parts of the nervous system increase the function of the sweat glands of the face, and increased sweating of the palms and armpits is also possible. Excessive sweating in the head area during VSD is provoked by various reasons: anxiety, eating spicy or too hot food, natural hormonal changes in women. Sweating begins suddenly, sweat appears in drops on the forehead or runs down the face, and the hair becomes wet. Such attacks are repeated up to several times a day.
Hypertensive crisis
A sudden increase in blood pressure is combined with dilation of the blood vessels of the scalp and face, which causes profuse sweating. According to the observations of patients, severe sweating occurs against a background of severe headaches and dizziness. Often there is a lot of noise in the ears, vision becomes blurred (“spots flash” before the eyes). In addition to the head, sweat is released and flows in droplets in the neck and upper torso. The skin in this area is red and hot to the touch. Such symptoms are more typical for the neurovegetative form of hypertensive crisis.
Cranial nerve damage
The development of increased sweating of the head may be associated with irritation of peripheral nerve endings. The most common is Lucy-Frey syndrome, which is caused by damage to the auriculotemporal nerve for various reasons (after mumps, sialadenitis, operations on the salivary gland). With this disorder, the head sweats heavily in the area of the ear and temple on one side, which often occurs after eating. The unreasonable appearance of beads of sweat on the chin is a sign of chorda tympani syndrome, which occurs after surgical trauma.
Neurological diseases
Excessive sweating of the head occurs in various brain pathologies that cause dysfunction of the sweat glands. In acute neurological problems, profuse sweating begins suddenly and is usually short-lived. In patients with chronic degenerative processes, the head sweats for a long time. Sweating may be accompanied by a decrease in memory and attention, speech disorders (long pauses between answers, incoherent speech), and temporary paresis of the limbs. Hyperhidrosis is caused by reasons such as:
- Parkinson's disease.
Sweating is a compensatory reaction to damage to the autonomic nervous system. In addition to increased sweat production in the area of the scalp and face, pathognomonic symptoms of the disease are noted: tremor of the fingers, gait disturbances, decreased memory, attention, and other cognitive functions. - Neurosyphilis.
Damage to the roots of the cranial nerves due to an infectious cause often leads to disruption of the normal functioning of the sweat glands, so patients have a profuse head sweat. In addition, debilitating headaches, dizziness, and tinnitus bother me. - Stroke.
Increased sweating occurs when the thermoregulation center in the hypothalamus is damaged. Characteristic feature: sweating is observed only on half of the head and neck (usually on the side of the muscle paresis). Speech and motor disturbances appear at the same time.
Traumatic brain injuries
After head injuries, severe sweating may occur, which is caused by damage to the nerve structures of the brain responsible for thermoregulation, or ruptures of the peripheral cranial nerves. The degree of disruption of the secretion of sweat glands depends on the cause of the TBI and the extent of the damage received. In addition to hyperhidrosis, painful headaches develop, accompanied by nausea and repeated vomiting, and loss of consciousness is possible. In severe injuries, local sweating gives way to cold sweat.
Complications of pharmacotherapy
The side effect usually occurs within minutes of rapid intravenous administration of nitrates, drugs used to treat stable angina and acute coronary syndrome. The appearance of severe hyperhidrosis in the face and head is preceded by a feeling of heat. Sweating is combined with severe redness of the skin. Headaches and dizziness are typical, and when suddenly getting out of bed, a pre-fainting state is observed. The presence of such disorders should be reported to your doctor in order to adjust the dosage of the drug.
Rare causes
- Essential local hyperhidrosis
. - Gustatory hyperhidrosis
: symmetrical sweating due to the trigeminovascular reflex. - Dermatological diseases
: organoid or diaphoretic nevus, exocrine hair angiomatous hamartoma, glomus tumors. - Hereditary diseases
: Hamstorp-Wohlfahrt syndrome, congenital dyskeratosis (Zinsser-Engman-Cole syndrome).
Sweating due to infection
The vital activity of viruses and bacteria is accompanied by the production of pyrogens that affect the thermal sensitivity of neurons. During the period of exacerbation of an infectious disease, body temperature always rises significantly, which is why hyperhidrosis occurs. The virus is accompanied by muscle pain and body aches, the bacterial infection is accompanied by a skin rash and general toxicity.
Rheumatism is also infectious in nature. The patient's body temperature is constantly elevated, which causes severe sweating. Damage to joints and connective tissue prevents normal movement, but people sweat as if after intense training.
Syphilis is a sexually transmitted disease that affects the mucous membranes. It is characterized by damage to the nerve roots located along the spine, which is expressed by a local increase in sweating.
Clinical researches
Clinical studies have proven the effectiveness, safety and tolerability of the products. The products are suitable for daily care of children's skin with mild to moderate forms of atopic dermatitis and during remission, accompanied by a decrease in the quality of life of patients.
Based on the results of clinical studies, the product packaging contains information that the creams are recommended by the St. Petersburg branch of the Union of Pediatricians of Russia.
Sources:
- Molochkova Yulia Vladimirovna, Dermatology. Brief reference book, GEOTAR-Media, 2022.
- Baumann Leslie, Cosmetic Dermatology. Principles and practice, MEDpress-inform, 2016.
- Ratner Desiri, Avram M.R., Avram M.M., Procedures in Dermatology. Clinical cosmetology, GEOTAR-Media, 2022.
Malignant and benign tumors
The center of thermoregulation is the hypothalamus, and tumors of any nature in this area cause hyperhidrosis. Sweating especially increases at night, regardless of the temperature in the room.
If this happens without explanation, then the following diseases can be assumed:
- histiocytic lymphoma (malignant lesion of lymphoid tissues);
- lymphocytic lymphoma (oncological damage to the lymph nodes);
- mixed lymphoma (complex cancer of the lymph nodes);
- Burkitt's lymphoma (malignant tumor of the jaw).
Oncological neoplasms are accompanied not only by hyperhidrosis, but also by sudden weight loss, sleep disturbances, general weakness and fatigue.
What research is being done to identify the true causes of hyperhidrosis?
Excessive sweating is a subjective concept. Not everyone is alarmed by hyperhidrosis, so we need to talk about pathology if increased sweating is not typical for a person, causes him severe discomfort and causes anxiety.
The initial examination is carried out by an endocrinologist or therapist, because in most cases the cause of excessive sweating is a disruption in the functioning of the endocrine system. The specialist gives a referral for standard tests showing the general condition of the patient’s body.
These include:
- general blood analysis;
- general urine analysis;
- blood chemistry;
- analysis of thyroid hormones (T3, T4, TSH);
- ECG.
Depending on the test results, the patient undergoes additional examinations.
Diagnostics
The cause of sweating of the head is identified by a general practitioner, who either makes a diagnosis independently or refers the patient to specialized specialists. A comprehensive examination is prescribed to assess the general condition of the body and exclude organic pathology that could cause increased sweating. The following methods have the greatest diagnostic value:
- Neurological examination
. The initial examination includes assessment of superficial and deep tendon reflexes, testing of cognitive abilities and muscle reactions. Dermographism must be examined, an orthostatic test and the Danini-Aschner maneuver must be performed, which help to exclude dysfunction of the autonomic system. - Electroneurography.
The study of the functional capabilities of the peripheral nerves of the head area is carried out using their local stimulation with electrical impulses. The method is necessary to identify specific syndromes (Lucy-Frey, chorda tympani). If there is possible brain damage, an EEG is indicated. - X-ray examination
. To exclude organic pathologies of the nervous system as the cause of hyperhidrosis of the face and head, the results of radiography are indicative. If suspicious formations or traumatic injuries are detected, a CT or MRI of the brain is prescribed to clarify the nature of the disease. - Functional tests
. The rate of sweat secretion is assessed using quantitative methods - gravimetry and evapometry. Hyperhidrosis is said to occur when sweating rates exceed 10 mg per minute. Qualitative tests are effective for detecting the affected area - starch iodine test, ninhydrin test. - Laboratory methods
. The examination plan includes standard general and biochemical blood tests. In women, estrogen and progesterone levels are determined. If syphilis of the brain is suspected, microscopic and bacteriological examination of the cerebrospinal fluid and serological tests are recommended.
If severe sweating of the head and face occurs against the background of intense skin hyperemia and painful headaches, blood pressure is measured, an ECG is recorded, and, if necessary, an ultrasound of the heart is performed. If symptoms develop in emotionally labile patients, psychiatric evaluation is required. For patients with primary local hyperhidrosis, consultation with a geneticist is advisable.
Description of tests and ultrasounds prescribed for excessive sweating
| Preliminary diagnosis | Research | What is the essence of the study? |
| Suspicion of cancer | Analysis for tumor markers | Analysis for tumor markers Tumor markers are specific proteins, the concentration of which increases in the body only during oncological processes. In healthy people, tumor markers are contained in minimal quantities. The main tumor markers are: PSA is a protein that concentrates in a man’s blood during the development of prostate cancer. An increase in protein also occurs with adenoma (benign tumor) of the prostate gland. HCG is present in the body of both women and men. It increases significantly during pregnancy, so it is additionally taken along with a blood test for alpha-fetoprotein (AFP). When the concentration of both proteins increases, a preliminary diagnosis of testicular cancer is made, and in women with ovarian cancer, the AFP level increases significantly. Also, an increase in hCG is observed in cancer of the stomach, uterus, intestines, liver, as well as uterine fibroids. AFP - increases in oncological processes, especially in the liver, as well as in cirrhosis, hepatitis and renal failure. In a pregnant woman, it indicates fetal pathology. Ca-125 is a tumor marker that helps identify cancer of the uterus, breast, stomach, liver, pancreas, etc. It also increases with endometriosis, ovarian cysts, and peritonitis. |
| Suspicion of a pituitary tumor | MRI and angiography Analysis for prolactin X-ray with an eye to the sella turcica Analysis of cerebrospinal fluid (CSF) | For pituitary tumors, a combined MRI and angiography technique is used - studying cerebral circulation. The technique allows you to detect tumors as small as 5 mm. Prolactin is a pituitary hormone that is responsible for milk production in women, but is also present in men. It increases with uterine fibroids, pregnancy, ovarian tumors, and pituitary tumors. Breast discharge in men is associated with an increase in prolactin, which reduces the concentration of male sex hormones and increases the levels of estrogen and progesterone. A pituitary adenoma is indicated by a prolactin concentration in the blood of more than 250 ng/l. The sella turcica is a bone formation in the bed of which the pituitary gland is located. When the walls of the sella turcica are deformed, one can judge the growth of a pituitary tumor. The only drawback is that bone deformation occurs only when the tumor is large. When identifying pituitary tumors, myelin basic protein (MBP) is of great importance. In a healthy person, its value does not exceed 4 mg/l. Also, with neoplasms, epithelial cells are detected in the cerebrospinal fluid, which should not normally be present. The analysis does not yet confirm pituitary adenoma, but is an indication for a more in-depth study. |
| Suspicion of diabetes mellitus | Blood and cerebrospinal fluid test for glucose | A feature of hyperhidrosis in diabetes mellitus is excessive sweating in the armpits, palms, neck, but dry skin of the legs and feet. A blood test will quickly indicate an increase in blood sugar. with an increased glucose content in the cerebrospinal fluid, we can talk about viral lesions of the brain (meningitis). |
| Menopausal syndrome | Sex hormone analysis | “Hot flashes” shortly before the onset of menopause are associated with a decrease in the level of female sex hormones and an increase in androgens. Determining the ratio of estrogen, progesterone, LH and FSH shows a complete picture of hormonal levels. |
| Suspicion of tuberculosis | PCR diagnostics | Polymerase chain reaction helps identify Koch's bacillus within 4 hours. Unlike Mantoux, PCR detects even one bacilli of the pathogen at the earliest stage of the disease. The analysis will also help to select an effective drug and identify resistance to certain drugs. |
| Suspicion of infection | Linked immunosorbent assay | ELISA allows you to see the connection between the body’s immune cell and the cell of the infectious agent. Depending on the type of immunoglobulin (IgE, IgD, IgG, IgM, IgA), the type of pathogen is identified. The analysis identifies more than 600 infectious agents and viruses. |
| Suspicion of heart disease | Laboratory blood test | ESR increases with endocarditis, rheumatic heart disease. In chronic heart failure, the level of protein, as well as potassium and sodium in the blood serum increases. High cholesterol indicates atherosclerotic vascular disease. An increase in white blood cells indicates inflammation. A large number of platelets is observed with venous thrombosis. Enzymes ALT and AST increase during myocardial infarction. An increase in electrolytes occurs when the heart rhythm is abnormal. C-reactive protein is concentrated during myocardial infarction. |
| Suspicion of pheochromocytoma | Ultrasound of the abdominal organs | Pheochromocytoma is a tumor of the adrenal glands that leads to hormonal imbalance. The tumor is visualized on ultrasound as an oval or round formation of increased echogenicity. |
| Suspicion of acromegaly | Analysis for somatotropin | Somatotropic hormone (GH) affects not only growth, but also overall metabolism. A high concentration of the hormone indicates a tumor of the pituitary gland, stomach or lungs, anorexia nervosa, cirrhosis of the liver, and renal failure. Sometimes an illiterate diet leads to an increase in growth hormone, leading to depletion of the body. Low levels of growth hormone indicate pituitary insufficiency caused by infectious lesions of the brain, autoimmune pathologies, vascular disorders and postpartum blood loss. |
general characteristics
Excessive sweating is a subjective complaint: patients notice that they sweat more than other people.
A person finds wet stains from sweat on clothes, not only in the armpits, but also on the chest or back. Sweating is combined with cold skin and an unpleasant, pungent odor that can be easily felt from a distance. Patients may note that a large amount of sweat appears only on certain parts of the body - for example, on the palms and soles of the face. Increased sweating is provoked by stress, minor physical activity, and food intake. The symptom also causes psychological disorders: the person begins to experience a feeling of shame, discomfort, and avoid contact with others. Great inconvenience is caused by excessive sweating of the palms, which interferes with professional activities and makes it difficult to meet people and shake hands. A short-term increase in sweat production in response to physical labor or emotional shock is considered normal, but persistent hyperhidrosis, which disrupts the quality of life, is an indication for contacting a specialist.