Relationship between the number of moles and the risk of melanoma
There is a lot of research on this issue. If you start reviewing everything, you will end up with a long and boring article that you will not be interested in reading, and I will not be interested in writing.
I have selected some of the largest studies that will help us form our own opinion on this issue.
However, before considering research data, let’s move from the folk concept of “mole” to the medical concept of “nevus”.
Prevention of angiomas
After establishing the true cause of the appearance of red moles, it is important to avoid provoking factors. As a preventative measure, experts recommend:
- drink at least 1.5 liters of water per day;
- eat more fresh fruits and vegetables rich in fiber;
- add olive oil to your diet;
- try to spend less time under the scorching sun;
- sunbathe only in the morning or evening (using sunscreen);
- stick to a balanced diet.
What is a mole and what moles are important?
Already at this stage, interesting things become clear. Not every brown formation on the skin fits the definition of a “mole” and will be counted.
In 1990, the International Agency for Research on Cancer (IARC) clearly defined the concept of a “nevus” (pigmented nevus) for epidemiological studies of this type.
Brown or black pigment spots or nodules (papules), which stand out quite well in a darker color against the background of the surrounding skin. Lesions to be counted should not show signs of freckles, solar lentigines, seborrheic keratosis, café-au-lait spots, or other non-melanocytic lesions.
The conclusions from this definition are both pleasant and not so pleasant:
1) What you previously thought was a mole may not be, and your risk of melanoma will be lower than you thought.
2) You will not be able to independently count the number of nevi on the skin. This can only be done by a doctor - a dermatologist or dermato-oncologist. I will say more, in some cases, without a dermatoscope, even an experienced specialist will not always be able to distinguish solar lentigo from a pigmented nevus.
Formation of nevi during pregnancy
Moles on the chest and other parts of the body during pregnancy appear against the background of active hormonal activity and its restructuring.
In particular, the appearance of new moles is influenced by an increase in progesterone, a hormone necessary to maintain pregnancy.
It is quite difficult to judge whether the appearance of new nevi is accompanied by a pathological process.
It will be helpful to see a dermatologist regardless of when new moles appear, during pregnancy or after it.
It is possible that many moles appear during pregnancy.
As a rule, they are not dangerous.
But dermatologists recommend that expectant mothers pay attention to formations and monitor their development.
At the first incomprehensible changes, contact a specialist.
How many moles is that? And which ones?
I will give 2 of the largest and most recent studies that I was able to find. Both works represent a meta-analysis, i.e. a synthesis of data from several clinical studies. In my opinion, this type of research is often more credible than a single study.
1. Study by Italian authors from 2005
Meta-analysis of risk factors for cutaneous melanoma: I. Common and atypical naevi.
The results of 46 individual studies are summarized.
Everything is the same, but in words: the risk of melanoma increases in direct proportion to the number of nevi, both ordinary and atypical. The minimum risk of developing melanoma is in a person with 15 or fewer nevi on the skin, no nevi on the hands, and no atypical nevi.
The maximum risk is for a person with more than 100 regular nevi, 15 nevi on the hands and 5 atypical nevi.
2. American study from 2010
Catherine M. Olsen, Heidi J. Carroll and David C. Whiteman
Estimating the Attributable Fraction for Cancer: A Meta-analysis of Nevi and Melanoma
The results of 49 studies were summarized.
The results are consistent with previous research.
The risk of melanoma increases with the number of common and/or atypical nevi on the skin.
In contrast to the previous study, it was noted that 42% of patients with melanoma had 25 or more common nevi and/or 1 or more atypical nevus.
The authors consider these patients to be a high-risk group and recommend more careful monitoring and training in self-diagnosis methods.
Unfortunately, neither in the first nor in the second study the authors make specific recommendations on the frequency and format of observation of patients at risk. We will try to formulate answers to these questions a little later.
Removal methods
If hanging moles cause discomfort, are often injured, or increase in size, their removal is indicated. There are several methods for removing hanging moles.
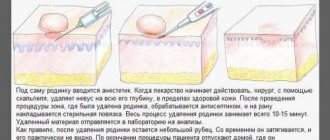
Surgery
The method of excision of a mole using surgical instruments is the most traumatic method of removing tumors. It is used primarily in cases where it is necessary to further examine the neoplasm material. It is performed under general anesthesia. After the procedure, scars and scars may appear, so if possible, this method is not used when removing hanging moles on visible areas of the body. To prevent the reappearance of the growth along with the mole, a small area of healthy skin is excised.
Cryodestruction
This method uses liquid nitrogen, under the influence of which the mole freezes and then falls off. This is an effective method that is suitable for removing tumors of various sizes. After removal of large moles, unaesthetic scars may appear.
Electrocoagulation
With electrocoagulation, the neoplasm is evaporated under the influence of high frequency current. A crust forms at the site of the removed mole, which falls off naturally within two weeks. After removing hanging moles, no traces remain on the body. But during the procedure, the patient may feel an unpleasant burning or tingling sensation. Therefore, patients with a low pain threshold are prescribed local anesthesia before electrocoagulation.
Laser correction
One of the safest and most effective ways to get rid of hanging moles on any part of the body. A beam produced by a special device affects the nevus and completely burns it out. After some time, clean, healthy skin forms at the site of the growth. With laser correction, bleeding and infection of the wound are excluded. The laser beam acts locally on the pathological area without damaging neighboring tissues. The procedure lasts no more than 20 minutes.
Using a laser, you can remove any benign tumors. There are a minimum of contraindications, but you must first consult with a specialist. The crust formed at the site of the mole must be protected from exposure to sunlight and moisture. A small hole may form at the site of the nevus. But there is no reason to panic. It will heal on its own within a few weeks.
You should not put off visiting a doctor if a mole has changed its color or shape or is bleeding heavily. The specialist will determine the method of removal individually based on the medical history, size and location of the tumor. Before surgery, it is important to identify the cause of the tumor. Hanging moles are often confused with papillomas.
What to do if there are a lot of moles on the body?
From the first study , we found that the likelihood of developing melanoma increases in direct proportion to the number of regular and/or dysplastic (atypical) nevi.
A second meta-analysis suggests that people with 25 or more common nevi and/or 1 or more atypical nevi are at risk for developing melanoma.
I think that after reading the previous paragraph, all readers were most likely divided into 3 groups:
- “I have a lot of moles and definitely more than 25, I’ll get melanoma! Oh God!"
- “I have less than 25 moles and I can now relax 100% about melanoma.”
- We ran to count the moles and realized that they couldn’t cope without a doctor.
It seems to me that there is no need to divide everything into black and white. Unfortunately, anyone can get melanoma. And those who have more than 25 moles, and those who have fewer, and even those who have only one or two moles. No one is 100% insured, it’s just that the probability is different for everyone. It is important to understand that the number of moles is just one of 17 risk factors for melanoma. I think that you shouldn’t draw any fatal conclusions and panic just because you have a lot of moles.
Brown moles
Such moles are a cluster of nevus cells. These cells are very similar to melanocytes and, like them, produce the pigment melanin. This pigment is brown in color, which makes our skin darker if there is a lot of it and lighter if there is not enough of it. Its production also increases after prolonged exposure to the sun.
Melanocytes and nevus cells
Melanocytes and nevus cells have certain differences, which we will not delve into. Let’s just note that brown moles most often consist of nevus cells. It is nevus cells that can turn into melanoma cells - one of the most malignant human tumors (more about it here)
How to be monitored if you have many moles?
In my practice, if a person does not have risk factors for developing melanoma, I recommend being seen by an oncologist for an examination with a dermatoscope annually in May at Melanoma Diagnosis Day. In addition to this, conduct a complete self-examination of the entire skin once every six months; you can examine a mole in a hard-to-reach place using two mirrors.
If a person has one or more risk factors, he or she should visit a dermato-oncologist for dermatoscopy once every 6 months and conduct a self-examination once every 3 months.
For those who have many moles (25, 50 or 100 - it doesn’t matter) and it seems difficult to monitor them, there is a type of dynamic monitoring called digital mapping of nevi.
Here's an example of how this happens in Germany:
This type of observation, according to the European Society of Clinical Oncology (ESMO), is considered the most adequate for patients with a large number of nevi:
According to data as of October 2022, such devices are available in Russia, Moscow and Yekaterinburg, the price for an examination can reach 10 thousand rubles.
Updated December 2022.
I am proud to announce that I am now conducting a similar examination in St. Petersburg.
Diagnosis of moles during pregnancy
What to do if you notice the appearance of new age spots on the skin or an old mole has enlarged during pregnancy?
It is necessary to make an appointment for an in-person consultation with a dermatologist.
The doctor will conduct a visual examination of the pigment formation, assess its condition and appearance.
Dermoscopy is mandatory to determine the possible pathogenicity of the nevus.
Dermatoscopy is a non-invasive method for the differential diagnosis of pigmented skin lesions and early diagnosis of malignant melanoma.
This technique is also known as dermoscopy, reflected light microscopy, and epiluminescence microscopy.
Dermatoscopy is an integral part of the dermatological examination of the skin.
Today, the dermatoscope is considered the “dermatologist’s stethoscope.”
In addition to the diagnosis of pigmented and non-pigmented skin tumors, the method will be able to establish the diagnosis of infectious, parasitic and inflammatory lesions of the dermis.
In the field of dermato-oncology, dermatoscopy contributes to preoperative planning for the removal of pigmented skin lesions.
Helps you choose the best treatment option and subsequent care.
The main task of a dermatological examination is to find out the following points:
- whether the lesion is melanocytic or non-melanocytic;
- whether the formation is benign, suspicious or malignant.
In modern dermatology, digital dermatoscopy is more often used.
Where diagnostics displays the results of the procedure on a computer monitor.
This allows you to create reports with patient data and images of his pigmented lesions.
This makes it easier to make a diagnosis and makes it possible to consult with other specialists.
Another advantage of this method is that the images can be printed and given to the patient.
Alternatively, the digital images can be transferred to a CD and sent to the appropriate physician.
Removal of angiomas in Moscow
Listratenkov Kirill Viktorovich is a highly qualified surgeon who has more than 12 years of experience. He can remove a red mole on the body without any problems. By conducting the procedure under sterile conditions using reliable equipment, safety and effectiveness are guaranteed.
For the convenience of clients, Kirill Viktorovich practices online consultations: on the website you can ask a question with an attached photo. He will give an answer soon. Despite the high quality of the services provided, the pricing policy is loyal. To make an initial appointment, just call the number provided or fill out a standard form with contact information.