ACNE TARDA Debut of late acne*
occurs more often in women than in men. Acne in patients over 25 years of age is characterized by the presence of comedones, the predominance of inflammatory elements such as papules and pustules in the cheeks, chin and neck. The severity of dermatosis in women varies from mild to moderate. The appearance or exacerbation of late acne in women is often associated with hormonal changes before and during menstruation, taking medications, and hyperandrogenism.
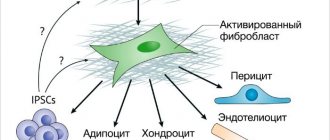
Clinical signs of hyperandrogenism that develops in diseases of the hypothalamic-pituitary system include hirsutism, acne, alopecia, baryphonia, and masculinization. There are adrenal and ovarian forms of hyperandrogenism. Polycystic ovary syndrome is one of the most common forms of endocrinopathies in women of reproductive age. The literature also describes MARSH syndrome, when the patient is diagnosed with a combination of melasma, acne, rosacea, seborrheic eczema and hirsutism.
Due to drug treatment, irrational home care, excessive exposure to ultraviolet rays on the skin and other reasons, patients with late-onset acne show signs of skin dehydration against the background of age-related skin changes.
Of course, the diagnosis of late acne is based on anamnesis and clinical picture, but it is also important to evaluate the results of laboratory (determination of the level of free testosterone, dehydroepiandrosterone sulfate, luteinizing hormone, follicle-stimulating hormone, etc.) and instrumental (ultrasound of the pelvic organs, etc.) studies. According to indications, consultations with an endocrinologist, gynecologist and other specialists are prescribed.
Treatment for acne in adult women includes not only external agents, but also systemic drugs, depending on the severity of the disease. To correct atrophic scars, post-inflammatory hyperpigmentation and age-related skin changes in patients with advanced acne, chemical peels, hardware and injection methods are used.
We present to your attention the drug HYALRIPAIER®–06 Bioreparant
(Lab. THOSCANE, Russia,
Fig. 1
), the complex action of which allows it to be used to correct several aesthetic problems at once, including age-related skin changes combined with a tendency to the appearance of inflammatory elements.
*Acne (acne vulgaris)
- multifactorial dermatosis, manifested by open and closed comedones, inflammatory skin lesions in the form of papules, pustules, nodules. Acne is one of the most common dermatoses. According to J. Leyden, acne affects 85% of people aged 12 to 24 years, 8% of people aged 25 to 34 years and 3% of people aged 35 to 44 years. Factors contributing to the development of acne include heredity, hormonal disorders, the patient’s lifestyle, nutrition, self-medication, etc. As a rule, against the background of increased levels of androgens, the sebaceous glands hypertrophy, sebum production increases, the keratinization process is disrupted, the number of Propionibacterium acnes increases and the development of inflammatory process in the skin. Resolution of inflammatory elements is often accompanied by the formation of scars and post-inflammatory hyperpigmentation.
HYALRIPAYER®–06 BIOREPARANT
HYALRIPAYER®–06 Bioreparant contains hyaluronic acid at a concentration of 6 mg/ml, modified with vitamin C and riboflavin. The drug has a gel form and is available in a dark glass bottle of 5 ml. For the production of the drug, hyaluronic acid of a pharmacopoeial class of high purity with an optimal molecular length (2 million Da) is used.
The drug is evenly distributed in the skin, hyaluronic acid ensures the straightening of the intercellular space and maintaining the three-dimensional organization of the components of the intercellular matrix, is responsible for skin turgor, is involved in protecting cells from oxidative stress and in regulating the processes of its own synthesis and decay, plays an important role in the hydrodynamics of cells and tissues, ion exchange, transport of substances from blood capillaries into the cell and from the cell into the lymphatic capillaries.
Replenishing the deficiency of hyaluronic acid by injecting it into the skin accelerates the processes of physiological and reparative regeneration.
Ascorbic acid
in the composition of the drug is necessary for the synthesis of collagen, reducing capillary permeability. In addition, it blocks melanin synthesis by inhibiting the action of tyrosinase. Ascorbic acid affects the formation of glycosaminoglycans, stimulates the proliferation of fibroblasts and reduces the production of metalloproteinases. Vitamin C is a powerful antioxidant.
Riboflavin
accelerates the process of tissue regeneration. Vitamin B2, regulating redox processes, participates in protein, fat and carbohydrate metabolism. As a result of phosphorylation, coenzymes are formed from riboflavin - flavin mononucleotide and flavin adenine dinucleotide, which are part of a number of enzymes. With a lack of vitamin B2, a deficiency of ascorbic acid occurs, and with a lack of ascorbic acid, the need for riboflavin increases.
After introducing hyaluronic acid modified with vitamin C and riboflavin into the dermis, a depot of biologically active substances is formed in the skin, which persists for a long time. During this period, there is a gradual release of biologically active components that perform the functions of nutrition, protection, restoration and stimulation. Physiological concentrations of substances ensure their maximum bioavailability, which creates optimal conditions for maintaining vital activity and rapid restoration of cells after damage.
Thanks to HYALREPAIR® technology, there is a prolonged stimulation of cellular activity - the production of one’s own young collagen, elastin and glycosaminoglycans, including hyaluronic acid (that is, the process of self-rejuvenation). Thus, HYALRIPAYER®–06 Bioreparant allows you to start rejuvenation processes, and is also recommended for patients with inflammatory elements, atrophic scars, post-inflammatory hyperpigmentation and other skin changes that have arisen as a result of acne.
Bioreparation: indications and contraindications
Bioreparation is a revolutionary technique for combating skin imperfections, which has much in common with biorevitalization. It involves the use of multicomponent preparations with hyaluronic acid, which cope with a huge number of cosmetic problems. Among them are 187:
- hyperpigmentation;
- excessive secretion of the sebaceous glands;
- decreased soft tissue turgor;
- scars, cicatrices, post-acne;
- rosacea;
- dehydration of the epidermis.
To treat acne with injections, formulations with coenzymes, nucleic acids, vitamins, peptides, and amino acids are used. Thanks to the expanded composition, in addition to the anti-aging effect, they additionally187:
- improve microcirculation, lymphatic drainage;
- relieve tissue swelling;
- even out skin tone;
- reduce subcutaneous fat tissue;
- protect cells from free radicals;
- increase skin immunity.
Due to the prolonged action of bioremedies, the effect of the procedure lasts up to 4-6 months. But there are a number of contraindications that limit the possibility of carrying out the procedure. Among them are 187:
- epilepsy;
- oncology;
- autoimmune diseases;
- increased tendency to tissue scarring;
- coagulation disorder;
- herpetic infection.
Like many other injection techniques, bioreparation is also not carried out during pregnancy and lactation.
BIOREPARATION PROCEDURE IN THE “FACE – NECK – DECOLLETE” AREA
Indications:
- age-related decrease in skin firmness and elasticity combined with a tendency to the appearance of inflammatory elements;
- acne;
- change in micro- and macrorelief (enlarged pores, hyperkeratosis);
- skin reactivity and sensitivity;
- atrophic scars (striae, post-acne);
- xerosis of the skin;
- seborrhea.
Target:
prevention and correction of aesthetic imperfections of the skin: smoothing superficial and deep wrinkles, lightening age spots, strengthening the walls of blood vessels, increasing skin turgor and tone, moisturizing it, reducing skin sensitivity, accelerating the regression of inflammatory elements, reducing the severity of stagnant spots.
Preparations:
HYALRIPAYER® - 06 Bioreparant, 5 ml bottle (Lab. THOSCANE, Russia); Cleanser Mousse (Medic Control Peel, Lab. THOSCANE, Russia); local anesthetic; antiseptic (chlorhexidine); Post Procedure Cream (MESALTERA by Dr. Mikhaylova, Lab. THOSCANE, Russia).
Syringe
volume 5.0 ml.
Needles:
0.3 × 4.0 mm (30G); 0.3 × 13.0 mm (30G); 0.23 × 4.0 mm (32G).
Duration of the procedure:
40-60 min.
Recommended course:
3-5 procedures with an interval of 2 weeks. Maintenance procedures: 1 time per month.
Before the procedure, the doctor conducts an examination, the patient fills out an informed voluntary consent to perform the bioreparation procedure and to take photographs.
Preparation for the procedure:
Makeup removal and exfoliation with Cleanser Mousse with bromelain and papain.
Application of a topical anesthetic to the skin under an occlusive film (exposure time 20-30 minutes). Double treatment of the skin with a 0.05% aqueous solution of chlorhexidine.
Improving the prevention and treatment of acne is one of the priority areas of dermatovenereology and cosmetology due to the chronic recurrent course of the disease, a significant decrease in the quality of life, regardless of the area and nature of the rash. Often the process is accompanied by the development of psychological and social maladjustment, depressive states, anxiety and dysmorphophobia [1, 2].
The psychological and social consequences of this disease are sometimes underestimated by both dermatologists and doctors of other specialties [3].
According to a number of epidemiological studies [4], in developed countries, acne affects 50-95% of adolescents. Of these, about 70% have mild to moderate acne. Acne is an inflammatory skin disease associated with changes in pilosebaceous structures. The social significance of acne is characterized not only by its prevalence throughout the world, but also often by the formation of secondary skin damage - post-acne, in which areas of scarring are formed.
In recent decades, numerous data have been obtained from various researchers about the role of Propionibacterium acnes
in the pathogenesis of acne.
The following effects have been reliably established and studied: stimulation of the proliferative activity of cells at the mouth of the pilosebaceous follicle due to an increase in the content of abnormal keratins; impaired differentiation of epidermal cells, increased their adhesion; stimulation of sebum production processes with an effect on sebocytes in the retention stage. The immune mechanisms of acne formation have also been studied. In particular, under the influence
of
P. acnes,
activation of toll-like receptors TLR-2 and TLR-4, antimicrobial peptides, matrix metalloproteinases occurs, activation of the synthesis of pro-inflammatory cytokines interleukin (IL)-1α, IL-1β, IL-6, IL-8 by immunocompetent skin cells and epidermal cells, IL-12, tumor necrosis factor-α. As a result, in addition to the formation of a local inflammatory process, its persistence and destruction of the dermal matrix occur [5, 6]. The proinflammatory cytokines IL-8 and TNF-α play a key role in maintaining the inflammatory response [7].
The main stages of acne development are follicular hyperproliferation and blockage, increased sebum production, P
.
acnes
and inflammation [8].
According to the modern classification of acne, the following main forms of the disease are distinguished:
- comedonal - represented predominantly by non-inflammatory elements (closed comedones) in limited areas (mainly in the central part of the face);
- papulopustular form - represented by both open and closed comedones in limited areas, mainly in the central part of the face, in the cheek area; in addition to comedones, there are a small number of pustules;
- nodular form - is represented mainly by inflammatory elements (pustules) in an amount of up to 25 pieces, against which there may be a small number of comedones;
- acne conglobata - a severe form of the disease in which pustules merge into nodes and adjacent areas of the skin become inflamed; with this form there is a high risk of scar development [9].
The first clinical sign of the onset of the disease is the formation of a comedonal rash [10].
The main manifestations of acne are non-inflammatory (open or closed comedones) and inflammatory lesions (papules, pustules or nodules) [11]. Currently, when treating acne, a number of clinical factors are taken into account, in particular the severity of the disease, the morphological nature of the elements of the rash, their number and prevalence, the results of previous treatment, as well as data on the side effects of drugs used previously [1].
According to many researchers [12], acne resistance to antibiotic therapy is one of the potential and significant reasons for treatment failures. This is further complicated by the fact that modern both European and Russian clinical guidelines do not indicate the possibility of monotherapy for acne with antibiotics. At the end of the 20th century, data began to appear on an increase in the number of P
.
acnes
, resistant to many broad-spectrum antibacterial drugs. Most often, resistance was determined in patients with moderate to severe acne. Researchers associate the development and spread of antibiotic resistance with iatrogenic causes, in particular with the incorrect regimen of drug use, deviation from the recommended regimen of drug use in the direction of reducing the dose of the antibiotic, frequent courses of treatment with these drugs, long courses of antibiotic therapy and the free availability of drugs for patients due to over-the-counter sales in a number of cases. countries [1].
In terms of increasing the clinical effectiveness of therapy, reducing the risk of resistance to antibacterial therapy P
.
acnes
, as well as increasing compliance with therapy, the most effective is the use of combination drugs [13].
The most significant is the use of combination drugs with a complementary mechanism of action. Combinations of drugs or active ingredients in the drug have an effect on a greater number of links in the pathogenesis of acne, in particular on follicular hyperkeratosis, colonization
of
P. acnes
, an inflammatory reaction of the skin [14].
Severe forms of acne require the prescription of systemic antibiotics. Previously, a number of methods were used with unproven effectiveness. Such methods include autohemotherapy, antistaphylococcal gamma globulin, vitamin A, estrogens [9]. In addition to vitamin A, the use of polyunsaturated fatty acids, such as omega-3, is effective [9].
Combined estrogen-gestagen drugs are also effective. Hormonal methods of therapy are relevant not only for patients with laboratory-confirmed hyperandrogenism, but also in cases of severe acne that is resistant to therapy, as well as with frequent episodes of exacerbation [15].
Estrogen in combined estrogen-progestogen preparations is usually represented by ethinyl estradiol, less often by mestranol, and progestin is often represented by chlormadinone, drospirenone and 19-nortestosterone derivatives. These components interact with testosterone receptors. Testosterone derivatives have an androgen-like effect – they promote the development of acne, cause irritability, and fatigue [15].
Estrogens in large doses have a sebosuppressive effect, but their isolated use and high dosage are associated with an increased risk of undesirable effects. Combined oral contraceptives (COCs) on the pharmaceutical market typically contain low doses of estrogens. Such COCs do not have a sebosuppressive effect, but compensate for hyperandrogenism in other ways:
- suppress the production of gonadotropic hormones of the pituitary gland, inhibit ovulation, thereby reducing the production of androgens by the ovaries;
- block androgen receptors;
- stimulate the production of globulin in the liver, which binds sex hormones, reduce the production of testosterone;
— progestins included in the drug suppress the activity of 5α-reductase, thereby inhibiting the formation of active androgens [16].
The effectiveness of oral contraceptives in the treatment of acne has been confirmed by numerous studies [17]. In addition, these effects may be masked by taking these drugs for other indications, while simultaneously preventing the development of acne. However, it is important to note that previous studies have shown that progestin-only medications, etonogestrel, and levonorgestrel may worsen acne symptoms [18].
Spironolactone can be used as an antiandrogen and potential inhibitor of sebogenesis, which is a possible alternative to oral isotretinoin and COCs, allowing to reduce the risk of side effects when taking drugs of these groups [18]. A number of studies [19] have shown the effectiveness of oral spironolactone in the treatment of acne in middle-aged women.
To date, there is information about 10 randomized controlled trials on the effectiveness of spironolactone in exacerbation of acne, and three articles have been published on the side effects of spironolactone in the treatment of acne in women [20, 21]. However, there are no generalized data on long-term treatment results.
All 10 studies were single-center and were conducted in Canada, Bangladesh, Thailand, Israel and China (one study each), the UK (2), and India (3). The severity of acne varied from mild to severe; was not specified in four studies [20]. In 7 studies, acne elements were localized only on the face [22].
The sources of funding for six studies are unknown; one study was funded by the manufacturer of spironolactone, two by organizations other than the manufacturer [22], and one study did not receive any support from pharmaceutical companies [20]. Information about the absence of conflicts of interest was provided in 2 studies [20, 22].
In 7 studies that assessed changes in blood potassium levels (due to the risk of hyperkalemia), there were no cases of increased levels in women [20, 22]. Similar data were obtained by M. Plovanovich et al. [21], who retrospectively analyzed serum potassium levels in 974 women aged 18–45 years taking spironolactone 50–200 mg/day for the treatment of acne. The study was conducted at two study sites in the United States between December 2000 and March 2014.
Based on these data, the researchers concluded that regular monitoring of serum potassium levels in women taking spironolactone for acne is not required [21]. In a study by M. Saint-Jean et al. [23] the effectiveness of spironolactone (75-150 mg/day) in the treatment of acne was noted in 14 women.
When comparing the effectiveness of the antiandrogens flutamide, finasteride, cimetidine, as well as ketoconazole and various COCs, no significant differences were found in comparison with the effects of spironolactone. The exceptions were COCs with unknown anti-acne efficacy [24, 25].
The effectiveness of spironolactone monotherapy for non-inflammatory acne has not been established. Expert opinions, commentaries, and clinical guidelines for the treatment of acne that include spironolactone (for example, in the USA) do not contain information on this [19, 26, 27].
Side effects of spironolactone were dose-dependent and were observed when the daily dose exceeded 200 mg. The most common side effect was menstrual irregularity. Many experts [19, 26] recommend simultaneous use of COCs, which can significantly reduce the frequency and severity of side effects. However, there are experts [19, 26, 28] who, paradoxically, recommend increasing the dose of the drug if it is ineffective. It is important to note that some current clinical guidelines include spironolactone [27, 29, 30].
Despite these data, there is no evidence of the benefits of oral spironolactone for the treatment of acne in women, and there is no reliable data on side effects and long-term results. Nevertheless, a statistically significant reduction in inflammatory phenomena in acne was shown when taking the drug at a dose of 200 mg/day [21].
There is evidence of the prescription of systemic glucocorticoids for severe inflammatory acne. In this case, it is necessary to take into account the side effects of prednisolone, in particular osteoporosis, increased blood glucose levels. The use of such drugs for more than 6 months is not recommended due to suppression of adrenal function [15].
Low doses of prednisolone (2.5-5 mg) or dexamethasone (0.25-0.75 mg) once a day (at night) prevent the production of androgens under the influence of adrenocorticotropic hormone (ACTH). This evening dose suppresses the morning ACTH peak and thereby helps reduce androgen levels [31].
Oral hormonal drugs in large doses may be effective in patients with severe inflammation due to acne, regardless of the presence of hormonal disorders, while low doses of glucocorticoids suppress adrenal function in the presence of hyperfunction. Excessive adrenal function may be indicated by elevated levels of dihydroepiandrosterone, 17-hydroxyprogesterone and androstenedione [28].
European guidelines recommend hormonal therapy as an alternative to isotretinoin for severe pustular as well as moderate nodular cystic acne. For nodular and conglobate acne, the combined use of antibiotics and hormonal drugs is the method of choice. An absolute contraindication for systemic hormonal therapy is the comedonal form of acne [1].
The combination of oral isotretinoin and corticosteroids is the regimen of choice for fulminant acne, but relapses are common, especially with low doses of corticosteroids [32]. To date, only one study has been published describing a good response to combination therapy with isotretinoin and prednisolone in fulminant acne [33].
The main effects of systemic administration of hormonal drugs are the suppression of androgen production in the ovaries, adrenal glands and pituitary gland (tropic hormones), as well as the inhibition of androgen receptors in pilosebaceous structures [34].
In the treatment of acne, the following groups of hormonal drugs are mainly used:
- androgen receptor blockers;
- COCs that suppress the production of androgens by the ovaries;
- glucocorticoids, which inhibit the production of androgens by the adrenal glands;
— 5α-reductase inhibitors [35].
Hormonal therapy is often used as part of complex therapy rather than as monotherapy. Most often, these drugs are combined with antibiotics, benzoyl peroxide, azelaic acid, and less often with retinoids. Usually, to achieve significant clinical improvement, it is necessary to take hormonal drugs for at least 3 months [36].
Before prescribing COCs in the treatment of acne, it is necessary to take into account the risk of side effects, in particular vascular thrombosis. When taking such drugs, the risk of thrombosis increases 3 times. However, these risks are significantly lower when taking new generation products containing low doses of estrogens, as well as in non-smoking women under 35 years of age. During the 1st year of COC use, the risk of venous thromboembolism is highest [37].
There is some evidence for the use of flutamide in the treatment of acne. This drug is used mainly for the treatment of prostate cancer, as well as in the treatment of hirsutism and androgenetic alopecia. The drug prevents the binding of dihydrotestosterone to its receptors, and also enhances the breakdown of the active form of testosterone into inactive metabolites. Doses of the drug range from 62.5 to 500 mg [25].
There are also limited data on the use of gonadotropin-releasing factor. Such drugs are produced in the form of nasal sprays, subcutaneous and intramuscular injections. There are currently no clear results of studies on the effectiveness of these drugs for acne, since there are a number of restrictions on the use of these drugs (for example, bleeding, osteoporosis and hot flashes) [39].
Since insulin resistance may be involved in the pathogenesis of acne, drugs that increase insulin sensitivity may be used in therapy. Thus, metformin can be used for acne in combination with polycystic ovary syndrome, HAIR-AN syndrome, obesity, or with laboratory confirmation of hyperinsulinemia. However, the drug does not cause hypoglycemia. Therapy begins with a dose of 500 mg/day, which can subsequently be increased to 2000 mg/day. If there is no positive dynamics within 6 months from the date of prescription of the drug, it is advisable to discontinue it. Side effects of metformin are dose-dependent. The most common symptoms are nausea and vomiting, which can be avoided by taking the drug after meals and reducing the initial dose to 250 mg/day [40].
For severe and treatment-resistant acne, the use of systemic retinoids is indicated. However, oral isotretinoin, which is a very effective drug for the treatment of acne, usually causes dry skin, cheilitis, and photosensitivity [38]. Systemic retinoids, according to many authors [44], are the most effective group of drugs for the treatment of acne. The main indications for their use are nodular cystic acne, often recurrent inflammatory acne, ineffectiveness of antibiotic therapy, and a tendency to form hypertrophic scars in place of resolved acne elements. Isotretinoin affects pathological follicular hyperkeratosis, reduces sebum production, and has anti-inflammatory and antichemotactic properties. Isotretinoin affects phagocyte chemotaxis and thus has indirect antibacterial properties against P
.
acnes
.
A decrease in sebum production is noted after approximately 2 weeks of therapy. Colonization of microorganisms and concentrations of inflammatory mediators in lesions are reduced. This occurs due to the interaction of isotretinoin with nuclear receptors, due to which the differentiation of sebocytes and, as a result, the synthesis of sebum are reduced [45].
Systemic antibiotics are prescribed in the presence of severe symptoms with a predominance of the inflammatory component. There are a number of limitations to antibiotic therapy, and it is also associated with a significant number of side effects. For example, amoxicillin affects the gastrointestinal tract, causing, for example, nausea and vomiting [41]. Macrolide antibiotics, such as erythromycin, have good clinical efficacy against acne [42]. In fulminant acne, oral antibiotics as monotherapy have low effectiveness [32].
Frequent and unjustified prescription of antibiotics for acne can provoke the development of antibiotic resistance. The drugs have only an antibacterial effect and do not affect the synthesis of sebum [43].
As a means of therapy and prevention of acne, it is possible to use enzyme preparations with anti-inflammatory and immunomodulatory effects. Such agents may include pancreatin, papain, rutoside, bromelain, trypsin, lipase, amylase, chymotrypsin.
EM. Dolzhikova et al. [46] assessed the effectiveness and pathogenetically substantiated the use of systemic enzyme therapy for various dermatoses, including acne. The therapeutic effectiveness of these drugs for acne is based on anti-inflammatory and immunomodulatory effects, as well as the ability to increase the concentration of antibacterial drugs in the lesion. Against the background of systemic enzyme therapy, a positive clinical effect is noted in the form of a decrease in erythema and itching, a decrease in the number of rash elements, and an increase in the processes of repair and epithelization. In addition, the risk of developing conglobate acne and hypertrophic scars after healing is reduced, and the period of remission is significantly increased.
The clinical effectiveness of systemic enzyme therapy has also been noted for diseases such as atopic dermatitis, eczema, scleroderma, psoriasis, porphyria cutanea tarda, and alopecia.
Convincing data were obtained by S. Wilson et al. [47] when using local injection of acidic peptidoglycan of plant origin as the main method of treatment for papulopustular acne. At the same time, a significant clinical effect was achieved. The immunological effect was manifested by an increase in the level of various subclasses of leukocytes, their activation, and an increase in their phagocytic activity. In addition, with this form of drug administration, there was no significant increase in the concentration of proinflammatory cytokines.
Thus, acne is a serious medical and social problem, and the arsenal of systemic therapy is limited. Only a small number of therapies are highly clinically effective in most patients. This circumstance requires a search for new therapeutic agents and a more in-depth study of the effectiveness of existing ones.
The authors declare no conflict of interest
.
1e-mail
STAGE I. DIFFUSE TREATMENT OF THE "FACE - NECK - DECOLLETE" AREA
Technique:
"papules".
Needles
caliber 30G.
The technique is used for the purpose of uniform distribution and deposition of the drug in the dermis. The needle is inserted at a minimum angle to the surface of the skin to the depth of the cut, which is directed upward. Injections are performed along Langer's lines from the center to the periphery from bottom to top.
Diameter of papules: on the face and neck - 2 mm, in the décolleté area - 3 mm. Distance between injections: on the face - 1.0 cm, on the neck - 1.5 cm, in the décolleté area - 2.0 cm (Fig. 2).
STAGE II. TREATMENT OF PROBLEM AREAS
1ST SUB-STAGE:
skin treatment in the periorbital area
(Fig. 3)
.
Technique: “papules”.
Needles
caliber 32G.
Injections are made into the skin of the upper and lower fixed eyelids, not reaching 5 mm from the eyelash edge. When performing injections, anatomically dangerous areas should be avoided (the medial part of the lower eyelid is the projection of the exit of the angular artery, the part of the upper fixed eyelid medial to the midpupillary line). The diameter of the papules is no more than 1 mm. The distance between injections is 0.3 cm. Injections are performed in a checkerboard pattern in the direction from the center to the periphery (Fig. 3)
.
2ND SUB-STAGE:
treatment of wrinkles and folds (Fig. 4).
Technique:
linear.
Needles:
0.3 × 13.0 mm (30G).
The linear technique is performed with the aim of mechanically damaging wrinkles and creases in the skin and creating a drug depot in these areas. HYALRIPAYER® 06 is injected directly under the wrinkle into the dermis at the exit of the needle. This technique is used to treat wrinkles such as nasolabial, labiomental, glabellar, and periauricular. The needle is inserted with the bevel upward at a minimal angle to the skin over its entire length with retrograde delivery of the drug. The needle can contour, but if the injection is performed correctly, it should not show through the skin. The distance between injections is the length of needle insertion. The direction of injection is along wrinkles and folds. The volume of the drug per injection is 0.1 ml (Fig. 4)
.
3rd SUBSTAGE:
treatment of areas with cavity-free inflammatory elements
(Fig. 5)
.
Technique:
"tubercles".
Needles:
0.3 × 4.0 mm (30G).
The needle is inserted at an angle of 45° to the skin surface over its entire length. The bevel of the needle is directed downwards. Injections are carried out at a distance of 0.5 cm from the inflammatory element in order to speed up its resolution. The amount of drug per injection is 0.1 ml (Fig. 5)
.
4TH SUBSTAGE:
treatment of areas with stagnant spots, enlarged pores and facial oval
(Fig. 6)
.
Technique:
"middle nappage".
Needles:
0.3 × 4.0 mm (30G).
Used to stimulate regeneration, mainly through microtraumatization and reflex enhancement of blood circulation in the skin.
Injections are performed at a fast pace with a constant supply of the drug at an angle of 30° to the skin surface to the depth of the needle cut. The bevel of the needle is directed upward. The distance between injections is 0.3 cm. The distance between injection lines is 0.5 cm. The lines are arranged in a grid (Fig. 6)
.
Hydro reserve
The hydroreserve (bio-reinforcement) technique is based on the introduction of special skin boosters under the skin, the main task of which is to restore the water balance of cells, regenerate the structure of the skin, and ensure antioxidant status.
Skinboosters are based on hyaluronic acid, which helps normalize tissue respiration, moisturize the deep layers of the skin, and enhance metabolic processes. The active components present in the preparations have a complex effect188:
- restore damaged cells;
- help speed up rehabilitation after aesthetic procedures;
- optimize work and mitigate the effects of botulinum toxin.
The preparations can be used for any skin type. Skinbooster not only fills subcutaneous voids, but also heals the skin from the inside. It stimulates the long-term production of hyaluronic acid, which in turn has a beneficial effect on problem skin.188
But for hydroreservoir, as for other injection procedures, there are a number of restrictions. The procedure cannot be performed if the following conditions are present:
- ARVI;
- exacerbation of chronic diseases;
- blood clotting disorder;
- pregnancy, lactation;
- autoimmune diseases;
- open wounds, infections in the injection area;
Skinboosters, which are used to create a hydraulic reserve, have high biological compatibility. They are produced biotechnologically, which minimizes the risk of allergic reactions to protein components.
Often, preparations for hydro reserves do not require preliminary testing, because they are perceived by the body as a related substance. Due to their high biological compatibility, the active substances do not cause immune or allergic reactions.
POST-PROCEDURAL CARE
Skin treatment with 0.05% aqueous solution of chlorhexidine. Application of Post Procedure Cream, intended for the care of damaged skin. The cream has a pronounced anti-inflammatory effect, reduces swelling, reduces burning sensation and moisturizes the skin, resolves stagnant spots.
For daily care, the patient is recommended a moisturizing cream for oily and normal skin Anti Acne Hydrating cream
(MESALTERA by Dr. Mikhaylova, Lab. THOSCANE, Russia). Thanks to the Ac.Net complex, the cream normalizes sebum production, reduces the severity of hyperkeratosis and the number of inflammatory elements. The AcquaCell complex instantly moisturizes the skin, and shea butter restores the lipid barrier. Apply to cleansed, dry facial skin twice a day - morning and evening.
RESULTS OF THE PROCEDURE
As a result of one bioreparation procedure using the drug HIALRIPAYER®–06 Bioreparant in a bottle, the following effects were achieved:
- improvement of skin color;
- reducing the severity of stagnant spots;
- increased skin turgor;
- regression of inflammatory elements.
In order to lift the skin, correct wrinkles, lighten age spots, strengthen the vascular wall, the patient was recommended to undergo a course of 5 bioreparation procedures with an interval of 2 weeks. After achieving the desired result, the patient will be prescribed maintenance bioreparation procedures (once a month). The results can be assessed by comparing photographs of the patient before and after the procedure (Fig. 7)
.
LITERATURE:
1
James J. Leyden. New Understandings of Acne Pathogenesis, Journal of Cutaneous Medicine, Volume 1, Supplement 2, 1996.