Oxolinic ointment for condylomas and other types of ointments are used for topical treatment of HPV. These remedies are intended to get rid of defects and discomfort caused by the disease. There is a fairly wide range of drugs recommended by doctors for papillomavirus, however, the choice of drug is made individually.
In this article we will talk about how condylomas manifest themselves, as well as what ointments are used to treat them and what the effect of these drugs is. In addition, we will consider means that, contrary to popular belief, are ineffective.
Additional use of other forms of drugs enhances the effectiveness of treatment
What are condylomas
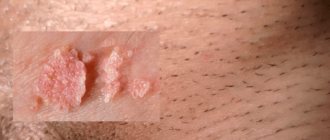
Condylomas are one of the types of manifestations of the human papillomavirus. They look like papillary growths or cauliflower and tend to merge.
Their color can vary from flesh-colored to reddish. They affect the mucous membranes and skin, mainly in intimate places: the glans penis, frenulum, perianal area, perineum, vestibule of the vagina, labia minora, cervix.
Condylomas have a long chronic course, wide distribution and high susceptibility. In addition, they can degenerate into malignant neoplasms and provoke bleeding. The disease is transmitted sexually through any type of unprotected sexual contact. Intrauterine infection of the fetus from an infected mother also occurs.
The virus changes the nature of tissue growth, which causes various changes in the mucous membranes and skin, including precancerous ones. The occurrence of infection and its development occurs against the background of weakened immunity.
Factors that increase the risk of infection for men and women are:
- previous STDs;
- frequent change of sexual partners and lack of contraception;
- lack of vitamins;
- frequent stress;
- decreased immunity;
- vaginal dysbiosis;
- pregnancy.
Subsequently, HPV develops, after the end of the incubation period, condylomas with a certain oncogenic risk appear, and clinical symptoms appear, for example:
- the appearance of condylomas in the genital area, perineum;
- difficulty urinating when condylomas are localized in the urethra;
- bleeding due to injury from underwear;
- pain and discomfort;
- slight redness around condylomas;
- itching may occur.
Important! With condylomatosis, complications are possible that lead to injuries and the appearance of ulcers, inflammation of condylomas, phimosis and paraphimosis in men, progression of the disease, and, consequently, an increase in the size of tumors and their number.
Condylomas tend to merge with each other, forming something like cauliflower
Nosological classification (ICD-10)
- A41.9 Septicemia, unspecified
- A49.3 Mycoplasma infection, unspecified
- A59.0 Urogenital trichomoniasis
- A74.9 Chlamydial infection, unspecified
- B00.0 Herpetic eczema
- B00.1 Herpetic vesicular dermatitis
- B18 Chronic viral hepatitis
- B25.9 Cytomegalovirus disease, unspecified
- B34 Viral infection of unspecified localization
- B37.3 Candidiasis of the vulva and vagina (N77.1*)
- G03.9 Meningitis, unspecified
- J06 Acute upper respiratory tract infections of multiple and unspecified localization
- J11 Influenza, virus not identified
- J18 Pneumonia without specifying the pathogen
- N39.0 Urinary tract infection without established location
- N76 Other inflammatory diseases of the vagina and vulva
- O35.3 Fetal injury (suspected) due to maternal viral disease requiring maternal medical attention
- O35.8 Other fetal anomalies and lesions (suspected) requiring maternal medical attention
Use of ointments
Ointment for condylomas is classified as a medicinal treatment that is aimed at eliminating the growths of defective epithelium. The drugs act on damaged tissues and viral cells, which provoke the growth of new tumors, and also improve the appearance of the affected areas without leaving scars after use.
Ointment for genital warts will be quite effective only with regular use and personal hygiene.
The following types of ointments are used:
- Condylox - a drug that can prevent the growth of certain types of cells, is used to treat condylomas on the genitals. Not suitable for use against warts in the urethra, vagina or rectum. The drug is used for 3 days, after which a four-day break is taken. This treatment cycle is repeated about 4 times, or until most of the tumors disappear. In any case, the frequency of use and the amount of the drug required for application are discussed with a specialist.
- Oxolinic ointment for condylomas fights well against the virus by disrupting the reproduction of its cells. Apply 3% ointment for treatment for 3 months. Treatment of condylomas with oxolinic ointment occurs according to the following algorithm: first, healthy skin and the edges of the formation are treated, and then they move to the center. When applied to intact skin, the ointment does not leave marks or scars. The drug should be used 2-3 times a day. The drug has shown high antiviral activity, absolute safety and no contraindications; in addition, oxolinic ointment against condylomas has a low price.
- Veregen - ointment is used for the treatment of external condylomas on the genitals and in the perianal area. Before using the drug, you should consult a doctor, as side effects such as itching, irritation, erythema and burning can often occur. The product is applied to previously washed skin three times a day, and therapy is continued until the condylomas completely disappear.
- Panavir – has a pronounced virostatic effect; it contains plant components. Used for the treatment of infectious and inflammatory changes in the skin and mucous membranes, incl. for oral and genital herpes, papillomas and condylomas. It is recommended to apply the ointment externally twice a day for 7-10 days, however local allergic reactions may occur. In addition to its effect on condylomas, the drug has a positive effect on the immune system.
- Viferon - used for therapy for human papillomavirus infection. This is a complex product that contains human interferon recombinant alpha-2 and ascorbic acid. The drug has antiviral, antiproliferative and immunomodulatory effects. One of the features of the drug is the lack of formation of antibodies necessary to neutralize its active components. The ointment is applied 3-4 times a day in a thin layer to the affected areas, the duration of therapy varies from 5 to 30 days. Local allergic reactions may occur, which disappear within 72 hours after stopping use of the drug.
- Galaderm is used to treat various skin lesions; in addition to condylomas, it successfully copes with other growths. The drug is used three times a day for a month, applied to the affected areas. With long-term treatment, allergic reactions may occur.
- Salicylic ointment - in a dosage of 3% or 5% is often used to treat condylomas and other skin lesions (psoriasis, eczema, oily seborrhea). Its main effect is an irritant effect on mucous membranes and skin. The ointment is applied only to the affected areas, and healthy skin is protected with gauze or adhesive tape. The drug is used twice a day; it has the ability to soften condylomas, relieve pain and relieve inflammation. If the ointment is rubbed into the skin excessively, a burning sensation and minor pain may occur. The product is used for 3 months, during which time most condylomas completely disappear.
As practice shows, oxolinic ointment has the best quality-to-price ratio; when used, condylomas disappear in a fairly short period of time. The only minor drawback of the ointment is its careful use during pregnancy.
Drugs with low effectiveness
When treating HPV with these drugs, frequent relapses occur, or there is no therapeutic effect at all. One such remedy is acyclovir for condylomas. The drug is produced in the form of tablets, ointments, creams, injections. The active component of the drug has the ability to stop the replication of the pathogen due to the formation of defective DNA.
Despite the fact that acyclovir ointment is an antiviral agent, patient reviews indicate its ineffectiveness. Upon careful study of the instructions, it becomes clear that prescribing acyclovir for condylomas is not justified, since its main spectrum of action is aimed at combating the herpes virus.
However, the use of acyclovir is possible in the presence of a combined infection, for example, with genital herpes and condylomas on the genitals. This happens quite often, because condylomas can be combined with other diseases that are sexually transmitted.
In any case, the selection of drugs for local or systemic treatment should be carried out by the attending physician. This could be a dermatovenerologist, urologist or gynecologist. It is very important not to try to get rid of tumors on your own and not to use traditional medicine methods.
Condoms reduce the risk of HPV infection, but do not protect completely
Compound
| Ointment for local and external use | 1 g |
| active substance: | |
| interferon human recombinant alpha-2 | 40000 IU |
| excipients: tocopherol acetate - 0.02 g; anhydrous lanolin - 0.34 g; medical petroleum jelly - 0.45 g; peach oil - 0.12 g; purified water - up to 1 g |
| Gel for local and external use | 1 g |
| active substance: | |
| interferon human recombinant alpha-2b | 36000 IU |
| excipients: alpha-tocopherol acetate - 0.055 g; methionine - 0.0012 g; benzoic acid - 0.00128 mg; citric acid monohydrate - 0.001 g; sodium tetraborate decahydrate - 0.0018 mg; sodium chloride - 0.004 g; human serum albumin solution 10% - 0.02 g; distilled glycerin (glycerol) - 0.02 g; carmellose sodium - 0.02 g; ethanol 95% - 0.055 g; purified water - up to 1 g |
| Suppositories for rectal use | 1 sup. |
| active substance: | |
| interferon human recombinant alpha-2b | 150000 IU |
| 500000 IU | |
| 1000000 IU | |
| 3000000 IU | |
| excipients: alpha-tocopherol acetate - 0.055/0.055/0.055/0.055 g; ascorbic acid - 0.0054/0.0081/0.0081/0.0081 g; sodium ascorbate - 0.0108/0.0162/0.0162/0.0162 g; disodium edetate dihydrate - 0.0001/0.0001/0.0001/0.0001 g; polysorbate 80 - 0.0001/0.0001/0.0001/0.0001 g | |
| base: cocoa butter and confectionery fat - up to 1 g |
Pharmacodynamics
Human recombinant interferon alpha-2b has pronounced immunomodulatory, antiviral, antiproliferative properties, suppresses the replication of RNA and DNA viruses.
The complex composition of the drugs (ointment, suppositories, gel) causes a number of new additional effects: in the presence of antioxidants (tocopherol acetate and/or ascorbic acid), the specific antiviral activity of human recombinant alpha-2b interferon increases, its immunomodulatory effect on T- and B-lymphocytes increases , the level of secretory immunoglobulins of class A increases, the level of immunoglobulin E normalizes, and the functioning of the endogenous interferon alpha-2b system is restored. Ascorbic acid and alpha-tocopherol acetate, being highly active antioxidants, have anti-inflammatory, membrane stabilizing, and regenerating properties. The use of the drug VIFERON® as part of complex therapy makes it possible to reduce therapeutic doses of antibacterial and hormonal drugs, as well as reduce the toxic effects of this therapy.
It has been established that when using the drug VIFERON® there are no side effects that occur with parenteral administration of interferon alfa-2b preparations, and no antibodies are formed that neutralize the antiviral activity of interferon alfa-2b.
Verruxin
You can find effective remedies for papillomas among foreign drugs. Thus, an excellent effect can be achieved using the Finnish drug “Verruxin”, which is based on salicylic acid. The product is applied once a day with a cotton swab directly to the papilloma. As a rule, the formations disappear painlessly within 3-4 days, but if necessary, the therapeutic course can be extended to 14 days.
Verruxin ointment
This is a fairly safe product that is suitable for both adults and children. Nevertheless, the drug "Verruxin" cannot be called a cheap remedy - you will have to pay at least 1,100 rubles for a tube of gel. But no matter what remedy is preferred, you should not start treatment without first consulting a doctor.
Warts on intimate places: diagnosis
It is impossible to make an accurate diagnosis only with an external examination.
To correctly determine the form of the disease, the doctor will need to conduct laboratory and instrumental studies.
Only a venereologist can reliably establish a diagnosis based on clinical manifestations.
If it is necessary to diagnose formations on the cervix/endourethral, instrumental methods (colposcopy, urethroscopy) are used.
In a number of situations, additional laboratory testing may be required (using PCR methods, histo-, cytological studies).
For laboratory tests, tests of blood and affected tissues are used.
A detailed diagnosis will help the doctor prescribe the optimal treatment.
Treatment of intimate warts at home
If intimate warts appear, home treatment is possible.
Only a doctor can prescribe it, and the patient will be required to strictly follow his instructions.
With home therapy, warts in the intimate area are removed using cauterizing and antiviral agents.
These medications are mainly produced in the form of ointments for intimate warts.
Such drugs should be used strictly according to the instructions received from the doctor.
Remember! Self-medication of warts in the intimate area can greatly harm your health.
If you choose the wrong drugs, you can get a burn instead of a therapeutic effect.
Often, symptoms worsen and the process spreads when trying to remove the formation on their own.
Use during pregnancy and breastfeeding
Ointment: since when applied externally and locally, the systemic absorption of interferon is low and the drug has an effect only in the lesion, it is possible to use the drug VIFERON® during pregnancy and lactation.
Gel: since the systemic absorption of interferon when applied topically is low and the drug has an effect only in the lesion, it is possible to use the drug VIFERON® during pregnancy and breastfeeding. During lactation, do not use the drug on the area of the nipples and areola.
Suppositories: the drug is approved for use from the 14th week of pregnancy. There are no restrictions for use during lactation.
Intimate warts: how to treat and who to contact?
To properly treat the infection and its consequences, you need to consult a dermatologist-venereologist.
A specialist will be able to accurately determine the course of the disease and select the optimal treatment.
If consultations with other specialists are necessary, they will be prescribed by the attending physician.
The compulsory health insurance system allows you to seek help from state medical institutions.
You can wait several weeks for an appointment at such institutions.
Paid services are available to the patient much faster and allow you to choose a convenient time to visit the doctor.