Causes of nevus
Pigmented nevi appear in utero, in other words, they are often congenital. Somewhere between 15 and 24 weeks of pregnancy, pigment cells migrate from the neuroectodermal tube to the superficial layers of the skin and form clusters of nocytes there, leading to the appearance of a birthmark. It is believed that such migration occurs under the influence of unfavorable factors affecting a pregnant woman. These include: infections (especially viral ones), taking certain medications, excessive insolation, radiation, and the effects of toxic substances. Genetic predisposition is also no exception.
With age, new nevi may appear, however, there is an opinion that this is only a manifestation of long-existing skin changes that arose in utero. Pregnancy, menopause, allergic and autoimmune diseases, exposure to harmful production factors, and much more can push the body to the appearance of new moles.
Diagnostics
It is necessary to diagnose melanoma in time and determine the stage of its development in order for the treatment of the disease to be successful.
First, an anamnesis is collected, the doctor learns about changes in the nevus.
Do not take a biopsy or expose the mole to chemical and electrical effects unnecessarily.
To diagnose you need to do:
- Histological examination (a superficial smear is taken if there is bleeding or cracks, provided that the tumor is removed immediately after the diagnostic results);
- Epiluminescent microscopy (examination of a mole using a special apparatus to determine its structure);
- CT (image recording, data processing, comparison with standards).
Classification and signs of nevi
In total, up to 15 types of nevi are distinguished, differing from each other in location, size, intensity of staining, shape and ability to malignant degeneration. Let's talk about the most common of them.
Borderline pigmented nevus
It is a flat spot on the skin measuring up to 5 mm. The color ranges from light brown to dark and can be found on any part of the body, even on the palms and soles. Hair does not grow on the surface of this type of nevus. Usually this is a single education. The appearance of new spots around it, a change in the color of the border nevus, or ulceration may indicate the onset of malignancy and requires urgent consultation with an oncologist.
Pigmented complex nevus
Based on localization, this nevus is located in two layers of skin - the epidermis and dermis, which is why it is called complex. Outwardly it looks like a regular mole, the surface is smooth, rises above the skin, dimensions up to 1 cm. Colored differently: from light to almost black.
Intradermal nevus
It has, unlike a complex one, a bumpy surface with many cracks. You can find it on the neck or head. Sometimes it can be on a thin stalk (like a hanging mole).
Blue nevus
It is very dangerous in terms of the development of melanoma. It is a dense nodule measuring up to 1 cm with a smooth surface of a black-blue hue. Frequent locations are the back of the hands and feet, buttocks, and lumbar region. Blue nevus grows extremely slowly, reaching up to 3 cm in diameter. When located on traumatic parts of the body, it is capable of malignancy.
Basal nevus
In other words, this is an ordinary flesh-colored mole of small size, with almost no melanin. Perhaps this is the most common type of nevus, which has no tendency to malignant degeneration.
Warty nevus
It resembles a papilloma with a bumpy surface and is located on the scalp or neck.
Giant nevus
This is a very large pigmented nevus (more than 20 cm). Sometimes such a benign formation occupies part of a limb or face. Giant nevi must be removed due to the high risk of malignancy (up to 40% of cases, this type of nevus degenerates into melanoma).
All other types of pigmented nevi (nevus of Ota, Ita, Becker and others) are not so common. Of particular note is the existence of ocular nevus. This is a small spot on the iris or retina that is detected during an ophthalmological examination.
Congenital malformations of the skin and subcutaneous fat
Congenital malformations of the skin and subcutaneous fat in children have various forms of manifestation.
One of them is nevus. This is a neoplasm that appears as a result of a high concentration of nevocytes in a certain area of the skin. Normally, skin color is formed by melanocytes distributed in equal density. However, pathology may develop, due to which melanocytes degenerate into nevocytes, which, through their accumulation, form a pigmented nevus in a child. It can occur during pregnancy or appear shortly after birth.
To one degree or another, the following factors can lead to the development of pathology:
- gene breakdown;
- the presence of a genitourinary infection in the mother during pregnancy;
- heredity;
- the impact of negative external factors on the mother’s body during pregnancy;
- incorrect diet of the mother during pregnancy, the predominance of artificial colors, preservatives, and flavors;
- long-term use of hormonal contraceptives before pregnancy.
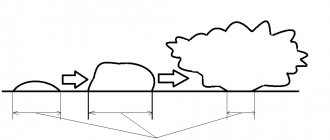
Initially, pigmented nevus in children is defined as a benign formation. However, it may have melanocytic activity, which means it can grow. As the child ages, not only the spots may grow, but also the appearance of new ones, as well as their degeneration into malignant tumors. A skin tumor - melanoma - is aggressive, as it quickly progresses and metastasizes to nearby organs and tissues.
Pigmented nevus is detected in approximately 1% of children.
Boys and girls are equally susceptible to the appearance of spots on the skin. A nevus can look different: a medium or large-sized nodule, a spot colored differently from the main skin tone, a wart. Localization is also varied: limbs, torso, head. In most cases, nevus occurs on the child's head, neck, chest or upper back.
The size of the formations varies from several mm to several cm. In approximately 5%, the number of nevi is so large that they occupy a significant proportion of the skin surface. Normally, when palpated, they can be both soft and nodular, but without pain.
diagnosis of pigmented nevus
- Finding out the history of the disease and visual examination of the pigment spot allows you to obtain up to 50% of the information.
- Dermatoscopy is performed in most developed clinics. The essence of the study is to view the nevus under a fluorescent microscope. Using this method, you can evaluate the surface of the nevus, the presence of microcracks, the color of individual parts, the condition of nearby skin, signs of inflammation, and more.
- Computer diagnostics of pigment spots is an expensive procedure and is not carried out everywhere. With its help, the diagnosis of one or another type of nevus is made with up to 90% confidence.
- A nevus biopsy is performed as a last resort and according to strict indications. It is better to carry out a targeted biopsy of an already removed formation followed by histological examination. This type of diagnosis is the most accurate.
Signs of malignancy
Not all moles on the human body have the risk of transformation into melanoma; in most cases, malignancy does not occur. However, those people who have many nevi on their bodies and have had cases of cancer among their immediate relatives need to be attentive to the condition of their tumors.
Any changes that occur with the growth can indicate the beginning of the process of malignancy. It may change color, size, shape, outline, the edges may become blurred, black or red dots may appear on the surface, and white areoles may appear around the tumor. In addition, the mole may bleed, hurt, itch, and the skin around it may become thick and inflamed. If at least one of these factors is observed, you should consult a dermatologist or oncologist for advice.
The risk of melanoma increases if a person often sunbathes a lot on the beach or in a solarium, lives in an area with poor ecology or close to radiation. Also, any frequent damage to the nevus, be it physical, chemical or other, can accelerate the process of malignancy. For this reason, it is not recommended to take any specific action to remove a mole without consulting a specialist.
Complications of nevi
The most common complications of all types of pigmented nevi are degeneration into melanoma and infection. Malignization is typical mainly for giant and blue nevi, as well as for borderline pigmented nevi.
Signs of malignant degeneration of nevus:
- horizontal or vertical growth;
- ulceration and bleeding;
- the appearance of irregular shapes and changes in shape;
- change in color of the nevus;
- the appearance of burning, itching, pain;
- dropouts (daughter spots next to the main one).
The occurrence of at least one of the above symptoms is a reason to immediately consult a doctor.
What to do? Should I delete or not?
Fortunately, I was not able to find practical recommendations in which the mere presence of an atypical nevus on a person’s skin would be considered a direct indication for its removal.
On the other hand, the presence of single or multiple, atypical [7] and dysplastic [3] nevi on a person’s skin equally increases the risk of developing melanoma on the skin as a whole.
Thus, in my opinion, the most logical tactic seems to be not prophylactic removal of atypical nevi, but increasing the frequency of preventive self-examinations and examinations by an oncologist.
Treatment and prevention of nevi
All types of nevi are subject to mandatory periodic monitoring. Melanoma-dangerous nevi (giant, blue, borderline) must be removed, including healthy skin up to 5-10 mm in diameter, followed by plastic surgery (if necessary). After removal, a histological examination is required to determine the likelihood of melanoma!
Small nevi up to 1 cm are removed by laser or cryodestruction only when located in traumatic areas (belt, under the breasts in women, neck).
Prevention of all pigmented nevi consists of monitoring their growth and condition and timely taking measures to remove them.
Make an appointment by phone or.
general characteristics
Intradermal moles form on the surface of the skin and initially look like elastic palipules or nodules, which usually change their shape and size over time. They can be flat or convex, small (diameter up to 6 mm) or large (diameter more than 1 cm). Each person can have a large number of moles on their body, which in most cases manifest themselves during adolescence or after about 40 years. For some, the number of tumors is in the dozens, for others it can reach more than a hundred.
Typically, intradermal skin nevi form in the neck, armpits, under the mammary glands in women, or in the intimate area. Less commonly, they can be found on the scalp, face, back, stomach, arms or legs. In this case, moles can be located singly or in entire clusters. Distinctive features of growths of this type are:
- homogeneous shade that does not change over time;
- clearly defined edges;
- soft, painless surface;
- absence of inflammation and other negative processes.
Intradermal melanocytic nevus transforms into melanoma in only 16% of cases.
Prevention of melanoma
To avoid skin cancer, you should follow some rules:
- do not be in the open sun, especially from 10 to 16-17 hours;
- do not visit the solarium;
- wear wide-brimmed hats in the summer heat and, if possible, wear clothes made of light materials that cover the places where there are nevi;
- Do not injure the area of the pigment spot, do not irritate it with chemicals.
Do not forget: the use of ointments, creams and sprays against UV radiation does not provide one hundred percent protection against the appearance of melanoma! Take care of yourself, and if a problem occurs, contact your doctor immediately.
Therapist of the highest category, cardiologist, gastroenterologist. Menzhevitskaya Tatyana Ivanovna
Treatment method
Today, you can get rid of pigmented nevi in various ways. Medicine offers several options:
- surgical intervention: the formation is excised using a scalpel, while the doctor captures healthy areas of skin and tissue. Sutures are placed at the intervention site, and after they are removed, unfortunately, a scar remains on the skin;
- laser: using a directed laser beam, the formation is removed in a few minutes, leaving a barely noticeable white spot on the skin;
- cryodestruction: the technique is based on exposing the pigment spot to critically low temperatures. There are no cicatricial formations or unaesthetic scars left on the skin;
- radio knife: a minimally invasive, painless method of removal, after which there will be no scars on the skin.
After any of the listed options for removing formations, histology of the removed tissue is required to determine their benignity/malignancy.