Symptoms of blue nevus
Blue nevus can appear in people of any age group, but most often it is first discovered in middle age. It usually does not cause patients any particular discomfort (except for a cosmetic defect when it is localized on the face and is large in size). Blue nevus has the following clinical characteristics:
- intradermal nodule;
- round, spindle-shaped or elliptical shape;
- light gray, dark blue, blue-black or blue color;
- uneven color;
- clear contours;
- smooth, hairless surface;
- the size rarely exceeds a centimeter (although there are blue nevi larger than 3 cm);
- protrudes slightly above the skin or does not rise above it at all;
- the consistency is elastic and dense;
- most often localized on the buttocks and limbs;
- can form on the mucous membranes of the mouth, vagina, and cervix.
Removal of Jadassohn's nevus in young people
T. A. Gaidina (1, 2), A. S. Dvornikov (1), P. A. Skripkina (1), G. B. Arutyunyan (1)
Relevance of removal of Jadasson's nevus in young people
(1) Department of Dermatovenereology, Faculty of Medicine, Russian National Research Medical University named after N. I. Pirogov, Moscow
(2) Rednor Company LLC, Moscow
One of the benign skin formations is seborrheic nevus of Jadassohn (NSJ) - a hamartoma localized primarily on the skin of the face or scalp and is equally common in men and women. Pluripotent primary epithelial cells included in the structure of the NSJ are a favorable environment for the development of both benign and malignant tumors against its background. To exclude neoplastic transformation, it is advisable to remove the NSJ immediately after puberty. If surgical intervention is not possible, patients require constant dynamic monitoring. This paper presents two cases of successful CO2 laser removal of NSJ in young patients.
Key words: seborrheic nevus of Jadassohn, benign skin formations, malignant transformation of nevus, removal with CO2 laser
In 1895, the German dermatovenerologist Joseph Jadassohn first described hamartoma of the sebaceous glands [1]. Nevus of the sebaceous glands of Jadassohn (syn.: Nevus sebaceous Jadassohn, NSJ, nevus of the sebaceous glands, seborrheic nevus) is a congenital organoid nevus, localized primarily on the skin of the face or scalp and is equally common in both sexes (Fig. 1). The development of nevus is caused by proliferation and malformation of the sebaceous glands and is the result of differentiation of pluripotent cells towards mature sebaceous and apocrine structures [2]. Clinically, NSJ is presented as an asymptomatic solitary plaque of a round or linear shape, slightly raised above the skin level, up to 10 cm in size and has small hemispherical papules of pink, yellow or brown color with a smooth or papillomatous surface. NSJ is characterized by age-related features associated with the differentiation of sebaceous and sweat glands [3]. In young children, the nevus is hairless, hardly noticeable and has a smooth or poorly defined papillary surface. During puberty, the NSJ becomes more convex and becomes covered with closely adjacent papules, the color of which varies from light yellow to dark brown. Histological examination of NSJ in older patients can reveal abnormal formation of the epidermis and lobules of mature pilosebaceous follicles, a large number of different epithelial structures (dilated apocrine glands, abortive hair follicles) [4]. In adolescents, there are accumulations of undifferentiated cells resembling foci of basal cell carcinoma [2].
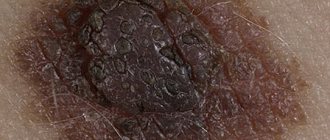
Fig.1
Seborrheic nevus of Jadassohn on the skin of the cheek in a 35-year-old woman.
This paper describes two clinical cases of removal of Jadassohn's sebaceous nevus using a CO2 laser.
Description of clinical cases
Case 1
Patient K., an 18-year-old man, came to the clinic with complaints of a formation localized on the skin of the left half of the bridge of the nose (Fig. 2).
Fig.2
Patient K., 18 years old. Seborrheic nevus of Jadassohn with cutaneous horn on the skin of the dorsum of the nose. Side view
History: the patient had the formation since birth. During puberty, he began to notice its slight growth and scanty discharge of a light yellow color, appearing when pressed. The young man repeatedly tried to independently squeeze out and remove the formation that was annoying him. A year ago, a growth appeared in the center of the formation, which over the past 6 months has increased to 0.5 cm (Fig. 3).
Fig.3
The same patient. Seborrheic nevus of Jadassohn with cutaneous horn on the skin of the dorsum of the nose. Front view
Status localis: the skin of the face is of normal color, in the T-shaped zone there is excessive sebum secretion, closed comedones. On the skin of the left half of the dorsum of the nose there are papules merging into an oblong-oval plaque measuring 0.5 × 0.8 cm, light pink in color, having a lobular structure and slightly rising above the skin level. In the center of the formation there is a cylindrical outgrowth 0.1 × 0.1 cm at the base and 0.5 cm in height. At the top of the outgrowth there are dense layered horny masses. On palpation, the formation is soft and painless. Histological examination: papillomatous epidermal hyperplasia and hyperplasia of the sebaceous glands were revealed. Clinical diagnosis: D23.3, seborrheic nevus of Jadassohn, cutaneous horn. Taking into account the localization and small size of the formation, a decision was made to remove the formation with a CO2 laser under local anesthesia. Examination 2 weeks after removal showed the formation of a normotrophic scar (Fig. 4)
Fig.4
The same patient. Formation of a normotrophic scar after removal of Jadassohn's nevus with a CO2 laser
Case 2
Patient A., a 30-year-old woman, came to the clinic for the aesthetic correction of a formation on the skin of her forehead (Fig. 5). History: the patient had the formation since birth. During puberty, the formation slightly increased in volume, became more protruding above the surface of the skin and acquired a darker color. Over the past ten years, the patient has not noted any changes.
Fig.5
Patient A., 30 years old. Seborrheic nevus of Jadassohn on the forehead.
Status localis: facial skin of normal color. On the skin of the forehead there are papules that merge into an oblong-oval plaque measuring 1.7 × 1.1 cm, light brown in color with a bumpy surface. The formation is characterized by a lobular structure and rises slightly above the skin level. On palpation it is soft and painless. Histological examination: subepithelial proliferation of the sebaceous glands was revealed (Fig. 6).
Fig.6
Skin fragment with subepithelial proliferation of sebaceous glands. Staining: hematoxylin-eosin; magnification x40.
Clinical diagnosis: D23.3, seborrheic nevus of Jadassohn. The patient underwent removal of the formation with a CO2 laser under local anesthesia. Examination 2 weeks after removal showed the formation of a normotrophic scar (Fig. 7).
Fig.7
Patient A., 30 years old. Formation of a normotrophic scar after removal of Jadassohn's nevus on the forehead skin using a CO2 laser
Discussion of clinical cases
There are differing opinions regarding the timing and advisability of NSJ removal. Before puberty, the NSJ is usually not noticeable. After puberty, secondary benign neoplasms develop in the NSJ with a frequency of 10–30% [5]. The literature describes various benign tumors that develop in the NSJ, of which trichoblastoma and syringocystadenoma are the most common [6]. This transformation of the NSJ brings additional discomfort to patients and requires aesthetic correction. The development of cutaneous horn due to NSJ is a rare phenomenon [7, 8]. There are no exact statistics on the incidence of malignant transformation of NSJ. The rarity of malignant transformation is noted by domestic researchers [2] and some foreign sources [9]. Other authors indicate malignant transformation in 22% of cases [10], most of which are described in patients over 50 years of age [11, 12]. It has been proven that the risk of malignant transformation increases with age [11]. Cases of the development of multiple neoplasms within the same NSJ in people over 50 years of age have been described [13]. The typical localization of NSJ on the skin of the face and scalp is also one of the risk factors for degeneration into a malignant tumor type. The cellular structure of NSJ (pluripotent primary epithelial cells) serves as a favorable environment for the development of malignant neoplasms against its background [2, 4]. Considering that the risk of malignant transformation exists, and the presence of the nevus itself is accompanied by aesthetic problems in patients, the authors consider it advisable to remove the NSJ in patients after puberty. The choice of removal method in young patients is quite wide: curettage, cauterization, cryotherapy, photodynamic therapy, laser ablation, surgical excision. The experience of successful use of a CO2 laser with a good cosmetic effect has been described in children [14]. This method is characterized by high efficiency, less damage to normal tissues and good cosmetic effect. In patients over 50 years of age, removal should be performed by radical surgery. If it is impossible to do this for any reason, constant dynamic monitoring is indicated.
CONCLUSIONS
The presented clinical cases demonstrate a good cosmetic effect after removal of NSJ with a CO2 laser. This method can be recommended as the method of choice for removing NSJs up to 2–3 cm2 in size in young people.
Literature
1. Lantis S, Leyden J, Heaton C. Nevus sebaceous Jadassohn. Arch Dermatol 1968, 98:117–23.
2. Molochkov V. A., Mardi Sh. On the development of basal cell carcinoma against the background of Jadassohn’s nevus of the sebaceous glands. Almanac of Clinical Medicine. 2007; 15:232–5.
3. Simi C, Rajalakshmi T, Correa M. Clinicopathologic analysis of 21 cases of nevus sebaceus: A retrospective study. Indian J Dermatol Venereol Leprol. 2008; 74 (6): 625–7.
4. Alessi E, Sala F. Nevus sebaceus. A clinicopathologic study of its evolution. Am J Dermatopathol. 1986; 8 (1): 27–31.
5. Liu Y, Valdebran M, Chen J, Elbendary A, Wu F, Xu M. Nevus sebaceous of Jadassohn with eight secondary tumors of follicular, sebaceous, and sweat gland differentiation. Am J Dermatopathol. 2016; 38(11):861–6.
6. Jaqueti G, Requena L, Sánchez Yus E. Trichoblastoma is the most common neoplasm developed in nevus sebaceus of Jadassohn. A clinicopathologic study of a series of 155 cases. Am J Dermatopathol. 2000; 22 (2): 108–18.
7. Pointdujour-Lim R, Marous MR, Satija CE, Douglass AM, Eagle RC, Shields CL. Cutaneous Horn of the Eyelid in 13 Cases. Ophthalmic Plastic and Reconstructive Surgery. 2017; 33 (4): 233–6.
8. Arvas L, Livaoglu M, Karacal N, Sozen E, Kara B. Giant cutaneous horn with naevus sebaceous. J Plast Reconstr Aesthet Surg. 2007; 60 (11): 1268–9.
9. Kamyab-Hesari K, Seirafi H, Jahan S, Aghzadeh N, Hejazi P, Azizpour A, et al. Nevus sebaceus: A clinicopathological study of 168 cases and review of the literature. Int J Dermatol. 2016; 55 (2): 193–200.
10. Westfried M, Mikhail GR. Multifocal Basal-Cell Carcinomas in a Nevus Sebaceus of Jadassohn. J Dermatol Surg Oncol. 1981; 7 (5): 420–2.
11. Idriss MH, Elston DM. Secondary neoplasms associated with nevus sebaceus of Jadassohn: A study of 707 cases. J Am Academ Dermatol. 2014; 70 (2): 332–7.
12. Jardim MML, Souza BC, Fraga RC. Rare desmoplastic trichilemmoma associated with sebaceous nevus. Anais Brasileiros de Dermatogia. 2017; 92(6):836–7.
13. Liu Y, Valdebran M, Chen J, Elberdary A, Wu F, Xu M. Nevus Sebaceous of Jadassohn wiht Eight Secondary Tumors of Follicular, Sebaceous, and Sweat Gland Differentiation. Am J Dermatopathol. 2016; 38(11):861–6.
14. Ashinoff R. Linear Nevus Sebaceus of Jadassohn Treated with the Carbon Dioxide Laser. Pediatric Dermatol. 1993; 10(2):189–91.
RUSSIA NEWSLETTER | 3, 2022 | VESTNIKRGMU.RU
Diagnosis of blue nevus
In most cases, one visual examination by a dermatologist is sufficient to accurately verify the diagnosis. In unclear and controversial clinical cases, the following examination is recommended:
- dermatoscopy (under magnification, the boundaries, depth and structure of pigment formation are studied more carefully);
- siascopy (assessment of the structure and distribution of melanin);
- ultrasonography of the nevus (to exclude infiltrative growth of a malignant nevus);
- histological examination of biopsy specimens (rarely) or surgical material (detects characteristic accumulations of melanocytes in the deep layers of the dermis; with a simple blue nevus, the cells are rich in melanin, and with a cellular nevus, islands of large cells with a small amount of pigment are observed);
- determination of tumor markers SU100 and TA90 (to exclude the development of melanoma).
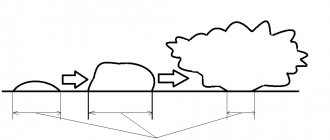
Stages of development
Nevus of the sebaceous glands of Jadassohn has a lobular structure, consists of cells of the sebaceous glands, grows from the middle and upper layers of the epidermis. Refers to harmartomas that arise as a result of pathologies of intrauterine development. The tissues are formed by the same cells as those of a healthy person, but differ in their dislocation and differentiation. Additionally, expansion of apocrine sweat glands and hair follicles is observed.
There are 3 stages of nevus development classified:
- At an early stage, hypoplasia of the follicles and sebaceous glands is noted.
- The mature stage is characterized by hyperpigmentation of the growth, superficial papillomatosis, and hyperplasia of the sebaceous glands.
- Stage of development of a benign or malignant tumor.
Treatment of blue nevus
As a rule, doctors choose a wait-and-see approach. Patients only need to visit a dermatologist or oncologist regularly for examination. Removal of a blue nevus is necessary only if localization is unsuccessful, causing permanent injury to the formation, and if a number of alarming signs appear:
- a significant increase in its value;
- color change;
- blurred contours;
- the appearance of itching or pain.
To remove a blue nevus use:
- electrocoagulation
- cryodestruction;
- laser;
- radio wave method;
- traditional surgical excision (the nevus is removed along with 5–8 mm of intact skin surrounding it and subcutaneous fat).
Causes of formation of nevus of the sebaceous glands
The etiology of the disease is not fully understood. Moles usually appear in children in infancy or the first few years of life, becoming larger as the child grows older, and their structure changes. The pathology is diagnosed equally often in both sexes. The hereditary factor plays an important role; if the patient’s close relatives suffered from similar ailments, then there is a high probability of a nevus of the sebaceous glands appearing in the baby.
Active growth and malignancy of the node can be provoked by congenital hyperplasia of glandular tissue, concomitant chronic diseases of the gastrointestinal tract, hormonal disorders, the presence of rosacea on the skin, and constant trauma to the growth.
There are several histological variants of seborrheic keratosis
There are acanthotic, hyperkeratotic and adenoid types. Despite certain differences, they all indicate a predominant localization of changes in the epidermal parts of the skin. Associated with acanthosis, hyperkeratosis and hyperpigmentation of keratocytes. Since these formations do not resolve on their own, they require removal. In cosmetically significant locations (open areas of the body), as well as in places of greatest trauma.
Treatment can be carried out in several ways: superficial electrical destruction, cryosurgical method, curettage or using a scalpel. However, none of the presented methods specifically combats hyperpigmentation. Using these techniques, it is only possible to remove the epidermal layers containing pigment. Thus leading to scarring on the surface of the skin. Laser treatment of benign pigmented tumors.
Why is it better to perform surgical excision of a nevus at the Swiss University Hospital?
- We employ specialists with extensive experience, including doctors of the highest category, professors, associate professors, and candidates of medical sciences. If necessary, doctors of narrow specializations are involved in treatment: oncologists, plastic surgery specialists, etc.
- Every year, more than 5,000 patients with various pathologies, including skin diseases, consult our specialists.
- The clinic offers almost all existing modern methods of treating skin diseases in accordance with the traditions of leading European clinics. Each specialist knows more than 100 types of operations within his specialization.
- More than 120 operations are performed in our clinic annually; we guarantee excellent quality and strict adherence to medical technologies.
Probability of malignancy
Seborrheic nevus most often degenerates into basal cell carcinoma. This is a malignant tumor that can grow into surrounding tissues and recur even after complete removal. Malignancy can be triggered by exposure to ultraviolet rays, hormonal changes in the body, and frequent trauma to the node.
In some patients, the simultaneous presence of benign and cancerous tumors is detected. It is worth noting that when moles become malignant, the disease progresses slowly, and metastasis occurs very rarely.
Sebaceous nevus can also develop into the following types of skin cancer:
- hydradenoma;
- apocrine cystadenoma;
- apocrine gland carcinoma;
- keratoacanthoma;
- squamous cell carcinoma.
Cancerous nevi are removed using the classical method, laser or cryodestruction. The prognosis for treatment is favorable, most patients recover. Complications occur less frequently, metastases form, and tumor relapses occur.
Nevus of the sebaceous and apocrine glands of Jadassohn is a congenital skin disease. The size of the growth increases as the child grows older, and the structure of pathological tissues changes. With the onset of puberty, the risk of the tumor degenerating into a malignant form increases, so doctors recommend treating diseases before puberty.
If there was no histology...
Calmly remember whether the doctor performed any additional research methods. Dermatoscopy? Scraping or puncture?
If yes, with a probability of about 95%, everything is fine and this is really a relapse of the nevus, and not melanoma. It requires nothing more than observation and, most likely, will not grow or change.
If there were no other examinations or histology, it seems to me advisable to excise the relapse with mandatory histological examination.
Yes, this is not easy or pleasant, but only such a step can confirm the absence or presence of melanoma.
If a mole, which was removed without histology, not only appears again, but has grown to its previous size, you need to go to an oncologist URGENTLY.
Is nevus recurrence dangerous?
In answering this question, the key point is the histological examination of the removed mole. If it was carried out and the benign quality of the formation was confirmed, a relapse is not dangerous to health.
If the removal was without histology, there is a possibility that the mole was malignant, i.e. melanoma. In this situation, the health risk increases in proportion to the lost time. The tumor remaining in the skin can begin to grow rapidly and metastasize.
In order not to create panic, I will emphasize: the likelihood of a situation with melanoma not being completely removed is not very high. However, it exists.
Seborrheic keratosis
Seborrheic keratosis (seborrheic wart, senile wart, seborrheic nevus of Unna, submersible papilloma) is classified as a benign tumor.
A fairly common disease that occurs mainly in the second half of a person’s life. The most common location is open areas of the skin exposed to sunlight, as well as areas of the body injured by clothing. Laser treatment of benign pigmented tumors. Clinically, seborrheic warts are large hyperpigmented foci of hyperkeratosis, more than 1.5 cm in diameter. With radial growth, with a warty surface, covered with dry horny masses.