Forms and complications of nevi
There are melanocytic (containing pigment cells - melanocytes) and non-melanocytic nevi (formed by cells other than melanocytes), which include epidermal nevus, nevus of the sebaceous glands, Becker's nevus and some other benign formations, vascular nevi of the skin.
Melanocytic nevi
There are acquired and congenital melanocytic nevi.
Acquired melanocytic nevi (AMN) are benign skin tumors. As a rule, they do not have a tendency to undergo malignant transformation. Special forms of acquired melanocytic nevi include Spitz nevus, Reed's nevus, spotted nevus (spilus), halonevus (Setton), and blue nevus (Jadassohn-Tiche) lying in the deep layers of the skin.
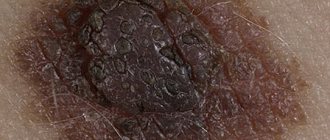
Atypical (dysplastic) nevi (AN) are classified into a separate group. Unlike common acquired melanocytic nevi, atypical melanocytic nevi may have some clinical characteristics of melanoma, such as asymmetry, ill-defined borders, multiple colors, or a size greater than 6 mm. Their main difference from a malignant tumor is stability, absence of changes over time and similar characteristics in one person. Atypical melanocytic nevi have a relatively increased risk of malignant transformation and require careful monitoring.
Congenital melanocytic nevi occur as a developmental defect (hemartoma) and are usually present at birth. Large congenital melanocytic nevi are also associated with an increased (but still low) risk of malignant transformation. Very rarely, they can be associated with a pathological accumulation of melanocytes in the central nervous system (neurocutaneous melanosis). Congenital melanocytic nevi with the expected size in an adult (over the course of life they will increase in proportion to the child’s growth) also require increased attention and medical supervision.
Nevi of Ota and Ito also have a melanocytic structure, but they are not based on excessive cell division, but on their accumulation in the deep layers of the skin.
Melanoma. Nevi (moles). The role of dermatoscopy in the prevention of melanoma development.
In 102 cable. paid appointment with a dermatologist: without an appointment, anonymously, on the day of treatment, on a first-come, first-served basis.
Melanoma is a malignant tumor of melanocytic origin. It belongs to the category of the most aggressive tumors with lympho- and hematogenous metastasis and has an extremely unfavorable prognosis. It can be hidden under the mask of pigmented and pigmented skin formations, which occur in 90% of the population. The most common benign, borderline and malignant skin formations: congenital pigmented nevus, congenital noncellular nevus, borderline nevus, flaming nevus, complex nevus, Spitz nevus, Reed nevus, Miescher nevus, Unna nevus, blue nevus, dysplastic nevus (Clark nevus), nevus sebaceous Jadassohn's glands, lentigo maligna, Dubreuil's melanosis, seborrheic keratosis, actinic keratosis, dermatofibroma, hemangiomas, vascular malformations, intraepidermal hemorrhages, freckles, solar lentigo, ink spot lentigo, Bowen's disease, pigmented form of basal cell skin cancer, primary melanoma, melanoma in situ, nodular melanoma, acral lentiginous melanoma, non-pigmented melanoma, metastatic melanoma, etc.
Among pigmented skin formations, melanocytic nevi occupy a special place; during the diagnosis and observation of which, skin melanoma and pre-melanoma lesions are mainly detected.
Only early detection and surgical excision of the tumor is the only possibility of effective treatment.
The most important factor in the development of melanoma against the background of melanocytic nevus (MN) is: -exposure to human skin of an excessive dose of ultraviolet radiation, leading not only to damage to skin cells, but also to a decrease in their immunity.
-skin phenotype I–II (proneness to sunburn of the skin, red hair, blue eyes, fair skin),
-3 or more episodes of sunburn of the skin during life,
-presence of freckles and lentigo or 3 or more atypical MNs,
-familial cases of melanoma in close relatives. MNs are observed in 3/4 of Caucasians and are benign tumors of the melanogenic system. Only some of them transform into melanoma (melanoma-dangerous MN) or are a marker of an increased risk of its development. Identifying them in order to prevent the development of melanoma is extremely important.
The vast majority of MNs are acquired. They are divided into ordinary and special types (spindle cell or epithelioid nevus (Spitz nevus, juvenile melanoma); nevus of balloon-forming cells; halo nevus (Setton).
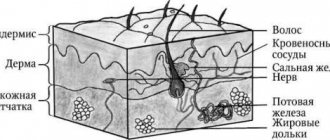
Among common MNs, borderline, complex (epidermodermal) and intradermal forms are distinguished. They arise after the birth of a child and have characteristic dynamics: first, due to the proliferation of nevus cells along the border of the epidermis and dermis, the formation of borderline MN occurs; over time, nevus cells move into the dermis, forming mixed MN; the borderline component may disappear with age, leaving only the dermal (intradermal MN) component.
Borderline MN manifests itself as a uniformly pigmented (from light brown to dark brown) spot with a diameter of 1–5 mm, round or oval in shape with a smooth surface and clear boundaries, located on any part of the skin and existing until approximately 35 years of age.
Mixed MN is a pigmented papule, sometimes with papillomatosis, rarely reaching 1 cm in diameter.
Intradermal MN is characterized by a dome-shaped or papillomatous papule, which may be blackberry-shaped, stalked, or mollusc-shaped with a broad base; its surface is covered with hair, its diameter rarely exceeds 1 cm, and its color varies from light brown to black. Rarely, depigmented MN with a whitish pink-red color is found.
Conventional MNs grow in proportion to the growth of the human body; after birth, their number increases, reaching a maximum during puberty, and after 50 years it gradually decreases, and by 7–9 decades of life they usually disappear.
Melanoma-dangerous MNs include congenital nevi and dysplastic nevi (DN).
But there is convincing evidence that melanoma can develop both in the tissue of intradermal MN and directly underneath it. Considering this possibility of melanoma developing against the background of intradermal MN, and also due to the difficulty of clinically distinguishing borderline and mixed MN from DN, in order to avoid malignancy, when For ordinary MNs, constant friction of clothing and contact with irritating substances should be avoided; mechanical hair removal from their surface is unacceptable.
Congenital MN are benign pigmented tumors consisting of nevus cells. They occur in 1% of Caucasian children, are detected at birth or during the first year of a child’s life and come in different sizes: from tiny to gigantic. Any of them can develop melanoma.
Dysplastic nevus - (synonyms: Clark's nevus, atypical nevus) - an acquired pigmented neoplasm. It occurs in 5% of the population [8] (including 30-50% of patients with sporadic and all patients with familial melanoma) and occurs in clinically unresponsive patients. affected skin or in the setting of complex or (rarely) borderline MN.
DNs appear later than acquired MNs—shortly before the onset of puberty or throughout life until old age. Their development is promoted by insolation. They are not characterized by spontaneous involution.
Although in the vast majority of cases acquired MN do not require treatment, it is still undertaken in some conditions.
A melanocytic nevus can be surgically removed if there is a rapid change in the element, an atypical clinical picture, suspicious for melanoma, for cosmetic reasons, or repeated injury to the element.
A melanocytic nevus must be immediately removed if at least one of 7 signs of a sudden (within one or several months) change is present:
- increasing the area and height of the element;
- increasing the intensity of pigmentation, especially if it is uneven;
- signs of local regression;
- the appearance of a pigment corolla around the MN, the appearance of satellite elements;
- inflammatory reaction in the MN;
- itching;
- erosion and bleeding.
Removal of MN must be complete and performed surgically with mandatory histological examination. After partial removal, the MN repigments and recurs, forming pseudomelanoma. Other methods of removal (electrocoagulation, cryodestruction, dermabrasion, laser) for pigmented formations of the skin and mucous membranes should not be carried out, since they do not provide documentary verification of the diagnosis.
Prevention of melanoma consists of early and active detection of pre-melanoma lesions (primarily DN and lentigo maligna), with constant dynamic monitoring of macroscopic changes in these spots. Patients with DN should be informed about the signs of transformation of these MNs into melanoma and independently regularly monitor the nature of individual elements.
Dermoscopy (dermoscopy, epiluminescent microscopy) is a non-invasive, accessible, painless, fast (It takes about 3 minutes to study one pigmented skin formation using dermatoscopy) diagnostic method for the early detection of melanoma and differential diagnosis of other pigmented skin tumors. The method of epiluminescence microscopy of the skin consists of applying mineral oil to the surface of a pigmented neoplasm in order to better penetrate light through the surface layers of the epidermis and study the object using a dermatoscope with a magnification of 10-40 times or more.
The use of dermatoscopy is effective for the early diagnosis of primary skin melanoma at an early (pre-invasive) stage of growth. Dermoscopy increases diagnostic accuracy by 5 to 30% compared to conventional clinical examination, depending on the type of skin lesion and the experience of the physician.
Symptoms of nevi
Nevi look like spots or nodules on the skin. Some of them are barely noticeable, others have a rich brown (melanocytic or pigmented) or red (vascular nevi) color.
As a rule, nevi do not cause any discomfort and are not felt.
Nevi can change their appearance and increase throughout life. It is important to correctly assess these changes; such manifestations can not only be a variant of the norm, but also serve as one of the signs of malignant skin formations.
Stages of changes in nevi
Melanocytic nevi , both acquired and congenital, are characterized by staged changes throughout life. The classic path of development includes 3 stages, which differ in the depth of the formation:
- a simple nevus or borderline nevus is a superficial flat brown spot;
- a complex or combined nevus is located deeper and looks like a brown spot or raised formation on the skin;
- An intradermal nevus is a light-colored, raised formation located deep in the skin.
Treatment of nevi
In most cases, no treatment is required, only observation is required, since nevi are benign formations. If a malignant nature is suspected and formations with a high risk of malignant transformation are identified, surgical excision is performed. It is possible to remove the nevus at the request of the patient for aesthetic reasons or because of discomfort (for example, when localized in areas of frequent trauma by clothing).
Features of the treatment method
Surgical excision of the nevus is optimal. This method allows for radical removal with a scalpel followed by suturing of the wound surface. In some cases, when nevi protrude above the surface of the skin, a radio knife, electric knife or laser knife can be used. In all cases of surgical treatment of melanocytic nevi, it is necessary to conduct a histological examination of the removed tissue.
Treatment
Treatment of nevi is indicated only in cases where there are signs of transition to a malignant formation. However, in cases where there is a high probability of injury to the mole, its removal is recommended. To select the appropriate method, the size of the tumor is taken into account, as well as its condition and the presence of signs of malignancy. Among the most commonly used treatment methods are:
- Destruction using a laser or electrocoagulator - excision under the influence of high temperatures or a laser. With the electrocoagulation method, the vessels are cauterized during the procedure, so the risk of bleeding is eliminated. The laser affects the deep layers of the skin, but healthy areas are not affected. This method is recommended for removing small moles.
- Chemical destruction - based on the destructive action of chemicals. It should be taken into account that incomplete removal of a mole threatens the development of a malignant process. Therefore, the most effective method is still surgery.
How are nevi treated in the Rassvet blade?
The doctor will examine the patient's skin completely to eliminate the risk of missing melanoma or other skin cancer. Suspicious formations are further studied using a device that allows you to examine the skin with 10 times magnification - a dermatoscope. The patient's chart describes nevi that require observation. The doctor will suggest surgical removal of suspicious nevi, followed by histological examination of the removed material (sent to an expert laboratory). Removal of nevi for aesthetic reasons can be performed at the request of the patient.
Recommendations of a dermatologist for patients with nevi:
- avoid excessive ultraviolet irradiation of the skin (tanning, sunbathing, solariums, ultraviolet drying of manicure and pedicure coatings); when staying outdoors for a long time, use a broad-spectrum photoprotective cream with SPF 30 or higher, clothing that covers the skin, a hat and glasses with an ultraviolet filter;
- try not to injure nevi when shaving, combing, changing clothes;
- undergo an annual preventive examination of nevi with a doctor;
- independently examine nevi according to the ABCDE rule;
- if there are a large number of nevi (50-100 or more), especially in combination with the presence of risk factors (sunburn, visits to a solarium, melanoma and skin cancer previously identified or in close relatives, the presence of atypical nevi), undergo a digital skin mapping procedure.
Author:
Kuzmina Tatyana Sergeevna dermatologist, Ph.D.
How nevi are removed
A nevus is removed when it becomes a cosmetic problem or is cancerous. The removal method is selected based on cosmetic indications or oncological indications.
Cosmetic
If cosmetic problems arise, the nevi are removed:
- Surgical intervention;
- Method based on liquid nitrogen;
- Using electric currents;
- Using laser surgery;
- Radiosurgical method.
Surgical intervention
It is well suited for removing large nevi. A disadvantage may be the presence of postoperative marks.
Adenoma
A liquid nitrogen
Also called cryodestruction. With it, the tissue is destroyed by cold. The nevus turns into a dry scab, under which new tissue then grows. The removal site is automatically protected from infections. This is how moles that are flush with the skin are removed. If the pathological tissues are not completely destroyed, then the procedure must be performed again.
Electricity
The method is also called electrocoagulation; it affects the tissue with high-frequency currents around the site of removal. Next, the material is sent for histology. The wound heals under the crust, forming a small scar.
Laser removal
Moles are removed with laser on parts of the body that are most often exposed, on the face. The laser acts precisely on the area, leaving a small removal diameter and preserving the tissue around the nevus. The crust protects the wound from infection.
Radiosurgery
The method is non-contact. In this case, tissues are excised with a special radio knife under radio wave exposure. It is often used in cosmetology. It is possible to remove both benign and malignant tissues. Simultaneously with removal, it has a disinfecting and hemostatic effect. There are no scars left after this operation.
Oncological indications
If there is a suspicion or it is definitely established that the nevus has degenerated into melanoma, then within the healthy tissues they are completely excised and examined for histology.