Skin structure
The skin consists of 3 layers: epidermis, dermis and subcutaneous fat (SAT) (Fig. 1). The epidermis is the thinnest of them and is a stratified keratinizing epithelium. The dermis is the middle layer of the skin. Mainly composed of fibrils of the structural protein collagen. PFA contains fat cells - adipocytes. The thickness of these layers can vary significantly depending on the anatomical location.
Fig.1. Skin structure
Localization options
Squamous cell skin cancer most often presents as a single lesion, much less often as multiple lesions. In the vast majority of cases, the skin of the face (nose, ears, periorbital area) is affected. Favorite localization is the transitions between the mucous membrane and squamous epithelium, which are observed on the red border of the lips, in the perianal region, and on the external genitalia.
In the oral cavity, this type of cancer is often located on the mucous membrane of the palate and tongue. This tumor is characterized by a long asymptomatic course. It gradually turns into a hard nodule or over time acquires the appearance of a peritonsillar abscess.
Squamous cell carcinoma on the lower lip occurs against the background of such precancerous formations as leukoplakia, actinic and abrasive cheilitis. Initially, it appears as tightly fitting scales, under which a small growing compaction forms. Less commonly, the disease begins with erosion, which has a dense base. As the tumor grows, the lip may become deformed or thicken.
For localization of cancer in the vulva area, localization is characteristic of the transitional fold of the labia majora and minora, and the clitoris. The disease has an unfavorable prognosis and is characterized by rapid metastasis. The formation of squamous cell skin cancer of this localization may be preceded by lichen sclerosus, Bowen's disease, and erythroplakia.
Penile skin cancer usually occurs in men over 40 years of age. Its typical location is the posterior surface of the body of the penis, the area of the preputial sac and coronary sulcus. Predisposing factors to the formation of this tumor are chronic inflammatory processes, balanitis with congenital phimosis, and accumulation of smegma. This is why penile cancer almost never occurs in men who have undergone circumcision.
Epidermis
Rice.
2. Epidermis The epidermis is a constantly exfoliating epithelial layer of the skin, which consists mainly of 2 types of cells - keratinocytes and dendritic cells. Melanocytes, Langerhans cells, Merkel cells, and intraepidermal T lymphocytes are present in small quantities in the epidermis. Structurally, the epidermis is divided into 5 layers: basal, spinous, granular, shiny and horny, differing in the position and degree of differentiation of keratinocytes, the main cell population of the epidermis (Fig. 2).
Keratinization. As keratinocytes differentiate and move from the basal layer to the stratum corneum, their keratinization (keratinization) occurs - a process that begins with the phase of keratin synthesis by keratinocytes and ends with their cellular degradation. Keratin serves as a building block for intermediate filaments. Bundles of these filaments, reaching the cytoplasmic membrane, form desmosomes necessary for the formation of strong contacts between neighboring cells. Further, as epithelial differentiation progresses, epidermal cells enter the degradation phase. The nuclei and cytoplasmic organelles are destroyed and disappear, metabolism stops, and cell apoptosis occurs when it is completely keratinized (turns into horny scales).
The basal layer of the epidermis consists of a single row of mitotically active keratinocytes, which divide on average every 24 hours and give rise to new cells in the overlying epidermal layers. They are activated only in special cases, such as when a wound occurs. Next, a new cell, a keratinocyte, is pushed into the spinous layer, where it spends up to 2 weeks, gradually approaching the granular layer. The movement of the cell to the stratum corneum takes another 14 days. Thus, the lifespan of a keratinocyte is about 28 days.
It should be noted that not all cells of the basal layer divide at the same rate as keratinocytes. Epidermal stem cells under normal conditions form a long-lived population with a slow proliferation cycle.
The spinous layer of the epidermis consists of 5-10 layers of keratinocytes, differing in shape, structure and intracellular content, which is determined by the position of the cell. Thus, closer to the basal layer, the cells have a polyhedral shape and a round nucleus, but as the cells approach the granular layer, they become larger, acquire a flatter shape, and lamellar granules appear in them, containing various hydrolytic enzymes in abundance. Cells intensively synthesize keratin filaments, which, gathering into intermediate filaments, remain unconnected on the nuclear side, but participate in the formation of multiple desmosomes on the membrane side, forming connections with neighboring cells. The presence of a large number of desmosomes gives this layer a spiny appearance, for which it received the name “spinous.”
The granular layer of the epidermis is composed of still living keratinocytes, distinguished by their flattened shape and a large number of keratohyalin granules. The latter are responsible for the synthesis and modification of proteins involved in keratinization. The granular layer is the most keratogenic layer of the epidermis. In addition to keratohyalin granules, keratinocytes of this layer contain large quantities of lysosomal granules. Their enzymes break down cellular organelles during the transition of the keratinocyte to the phase of terminal differentiation and subsequent apoptosis. The thickness of the granular layer can vary; its value, proportional to the thickness of the overlying stratum corneum, is maximum in the skin of the palms and soles of the feet.
The shiny layer of the epidermis (so named for its special shine when viewing skin preparations on a light microscope) is thin, consists of flat keratinocytes, in which the nuclei and organelles are completely destroyed. The cells are filled with eleidin, an intermediate form of keratin. It is well developed only in some parts of the body - on the palms and soles.
The stratum corneum of the epidermis is composed of corneocytes (dead, terminally differentiated keratinocytes) with a high protein content. The cells are surrounded by a waterproof lipid matrix, the components of which contain compounds necessary for exfoliation of the stratum corneum (Fig. 3). The physical and biochemical properties of cells in the stratum corneum vary depending on the position of the cell within the layer, directing the exfoliation process outward. For example, cells in the middle layers of the stratum corneum have stronger water-binding properties due to the high concentration of free amino acids in their cytoplasm.
Rice. 3. Schematic representation of the stratum corneum with the underlying granular layer of the epidermis.
Regulation of proliferation and differentiation of epidermal keratinocytes. Being a continuously renewing tissue, the epidermis contains a relatively constant number of cells and regulates all interactions and contacts between them: adhesion between keratinocytes, interaction between keratinocytes and migrating cells, adhesion with the basement membrane and underlying dermis, the process of terminal differentiation into corneocytes. The main mechanism for regulating homeostasis in the epidermis is supported by a number of signaling molecules - hormones, growth factors and cytokines. In addition, epidermal morphogenesis and differentiation are partially regulated by the underlying dermis, which plays a critical role in maintaining postnatal skin structure and function.
Treatment of hyperkeratosis
If symptoms of hyperkeratosis occur, you should consult a dermatologist. For an experienced, qualified specialist, it is not difficult to diagnose the presence of hyperkeratosis. Only in isolated cases, to clarify the nature of the formations, a biopsy of suspicious areas of the skin is required.
To effectively eliminate the problem of hyperkeratosis, especially affecting the skin of the face, complex therapy is required. It is also necessary to prescribe treatment for the disease that provoked its development, if one has been detected. To do this, the patient may need to consult not only a dermatologist, but also an endocrinologist or other specialist.
As part of the treatment of hyperkeratosis itself, drug therapy and cosmetic procedures are prescribed. The first is the use of retinoids, vitamin C, and sometimes topical corticosteroids. For faster skin restoration and elimination of cosmetic imperfections, the following is recommended:
- paraffin therapy;
- mild chemical peels;
- UV therapy;
- mesotherapy.
The use of scrubs and other mechanical exfoliation products is not indicated for hyperkeratosis. This will only worsen the situation and can lead to skin infection. But it is always recommended to apply emollients to the skin, which moisturize and soften the skin. They contain natural lipids or natural oils that nourish dry skin and saturate it with the substances it needs. As a result, it is possible to restore the skin’s natural protection and restore its natural smoothness.
In case of seborrheic hyperkeratosis, accompanied by the formation of growths, they can be removed using electrocoagulation, laser or cryodestruction.
Unfortunately, hyperkeratoses often accompany chronic diseases, which cannot be completely eliminated. Recovery can only be achieved in situations where thickening and peeling of the skin is caused by mechanical factors or treatable diseases, such as mycosis. In other cases, when dryness and thickening of the skin are caused by chronic dermatological or other pathologies, it is only possible to reduce the frequency of their exacerbations and the severity of the course, that is, to achieve a stable and long-term remission. But this requires the correct selection of treatment tactics, constant skin care, and often diet.
Drug therapy
First of all, vitamin A, also called retinol, and vitamin C are prescribed internally and externally. Normally, a person receives the necessary vitamins from food, but today rarely anyone can boast of a balanced diet.
Vitamin A, in addition to regulating cell growth, is necessary to maintain visual acuity, hair and nail growth, and also performs a number of other functions. For hyperkeratosis, vitamin A in the form of synthetic derivatives called retinoids is used for general and local therapy.
Some of the brightest representatives of this kind of drugs are Roaccutane, in which isotretinoin is the active ingredient, and Neotigazon, containing acitretin. These compounds are derivatives of retinoic acid. In the case of the development of follicular hyperkeratosis, the use of topical retinoids, in particular adapalene, is indicated.
If hyperkeratosis, especially follicular hyperkeratosis, is accompanied by an inflammatory process, topical corticosteroids are prescribed, for example, drugs based on hydrocortisone, prednisolone, fluacinolone, clobetasol. Most modern drugs in this group are available in several dosage forms: emulsions, creams, ointments. Moreover, the effectiveness of treatment largely depends on the correctness of its choice. Additionally, corticosteroids help accelerate the exfoliation of dead cells.
Paraffin therapy
Paraffin therapy is a cosmetic procedure in which special cosmetic molten paraffin is applied with a brush to a previously cleaned face or other areas of the body affected by hyperkeratosis. The procedure takes on average 20-60 minutes and promotes:
- gentle removal of dead cells;
- cleansing pores of impurities;
- activation of microcirculation;
- moisturizing the skin;
- reducing inflammation.
Peelings
For hyperkeratosis, chemical peelings are indicated, in particular using acids such as:
- salicylic;
- glycolic;
- dairy;
- lemon;
- apple;
- tartaric.
All of them have a good exfoliating effect, and also additionally open pores and moisturize the skin. As a result, it is possible to effectively solve the problem of excessive dryness and flaking of the skin, as well as improve its tone and texture, restoring velvety.
UV therapy
Ultraviolet irradiation helps eliminate the manifestations of hyperkeratosis by suppressing pathogenic microorganisms, including fungi, activating blood circulation and metabolism, suppressing the inflammatory process, and providing a regenerative and desensitizing effect.
Mesotherapy
Mesotherapy is a well-known cosmetic procedure, which consists of introducing into the skin the substances necessary for its proper functioning using numerous injections or using hardware. As a result, it is possible not only to saturate the tissues with vitamins, but also to achieve effective hydration, which helps reduce the manifestations of hyperkeratosis and improve the condition of the skin in general.
Thus, hyperkeratosis is a very common disorder, although it does not affect the face as often as, for example, the feet, elbows, skin of the legs and back. However, with excessive dryness and thickening of the facial skin, even in the form of small papules, a serious aesthetic disadvantage occurs. But with a timely visit to a dermatologist and the start of complex therapy, including the use of modern cosmetic procedures, it is possible to significantly improve the condition of the skin of the face and other parts of the body or even completely eliminate the signs of hyperkeratosis.
5 4 votes
Article rating
Dermis
The dermis is a complex, loose connective tissue consisting of individual fibers, cells, a network of blood vessels and nerve endings, as well as epidermal outgrowths surrounding the hair follicles and sebaceous glands. The cellular elements of the dermis are represented by fibroblasts, macrophages and mast cells. Lymphocytes, leukocytes, and other cells are capable of migrating into the dermis in response to various stimuli.
The dermis, making up the main volume of the skin, performs primarily trophic and supporting functions, providing the skin with such mechanical properties as plasticity, elasticity and strength, which it needs to protect the internal organs of the body from mechanical damage. The dermis also retains water, participates in thermoregulation and contains mechanoreceptors. Finally, its interaction with the epidermis supports the normal functioning of these layers of skin.
In the dermis there is no such directed and structured process of cell differentiation as in the epidermis, however, it also exhibits a clear structural organization of elements depending on the depth of their occurrence. Both the cells and the extracellular matrix of the dermis also undergo constant renewal and remodeling.
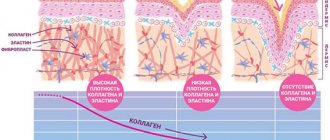
The extracellular matrix (ECM) of the dermis, or intercellular substance, which consists of various proteins (mainly collagen, elastin), glycosaminoglycans, the most famous of which is hyaluronic acid, and proteoglycans (fibronectin, laminin, decorin, versican, fibrillin). All these substances are secreted by dermal fibroblasts. The ECM is not a random accumulation of all components, but a complexly organized network, the composition and architectonics of which determine such biomechanical properties of the skin as rigidity, extensibility and elasticity. Epidermal keratinocytes, which are closely connected to each other, are attached to the ECM proteins. They form a dense protective layer of the skin. The structure of the ECM is also capable of exerting a regulatory effect on the cells immersed in it. Regulation can be either direct or indirect. In the first case, ECM proteins and glycosaminoglycans directly interact with cell receptors and initiate specific signal transduction pathways in them. Indirect regulation is carried out through the action of cytokines and growth factors retained in the cells of the ECM network and released at a certain moment to interact with cell receptors. The ECM structural network is subject to remodeling by enzymes from the matrix metalloproteinase (MMP) family. In particular, MMP-1 and MMP-13 initiate the degradation of collagen types I and III. The density of the ECM network of the dermis is uneven - in the papillary layer it is looser, in the reticular layer it is much denser, both due to the closer arrangement of the fibers of structural proteins and due to the increase in the diameter of these fibers.
Collagen is one of the main components of the ECM of the dermis. Synthesized by fibroblasts. The process of its biosynthesis is complex and multi-stage, as a result of which the fibroblast secretes procollagen into the extracellular space, consisting of three polypeptide α-chains folded into one triple helix. Procollagen monomers are then enzymatically assembled into extended fibrillar structures of various types. In total, there are at least 15 types of collagen in the skin; in the dermis, types I, III and V of this protein are most abundant: 88, 10 and 2%, respectively. Type IV collagen is localized in the basement membrane zone, and type VII collagen, secreted by keratinocytes, plays the role of an adapter protein for attaching ECM fibrils to the basement membrane (Fig. 4). Fibers of structural collagens of types I, III and V serve as a framework to which other ECM proteins are attached, in particular collagens of types XII and XIV. It is believed that these minor collagens, as well as small proteoglycans (decorin, fibromodulin and lumican), regulate the formation of structural collagen fibers, their diameter and the density of the formed network. The interaction of oligomeric and polymeric collagen complexes with other proteins, ECM polysaccharides, various growth factors and cytokines leads to the formation of a special network with certain biological activity, stability and biophysical characteristics important for the normal functioning of the skin. In the papillary layer of the dermis, collagen fibers are located loosely and more freely, while its reticular layer contains larger strands of collagen fibers.
Rice. 4. Schematic representation of skin layers and distribution of different types of collagens.
Collagen is constantly renewed, degrading under the action of proteolytic enzymes collagenases and being replaced by newly synthesized fibers. This protein makes up 70% of the skin's dry weight. It is the collagen fibers that “withstand the blow” under mechanical influence on it.
Elastin forms another network of fibers in the dermis, giving the skin such qualities as firmness and elasticity. Compared to collagen, elastin fibers are less rigid and curl around collagen fibers. It is with elastin fibers that proteins such as fibulins and fibrillins bind, to which, in turn, latent TGF-β-binding protein (LTBP) binds. Dissociation of this complex results in the release and activation of TGF-β, the most potent of all growth factors. It controls the expression, deposition and distribution of collagens and other matrix proteins in the skin. Thus, the intact network of elastin fibers serves as a depot for TGF-β.
Hyaluronic acid (HA) is a linear polysaccharide consisting of repeating dimers of D-glucuronic acid and N-acetylglucosamine. The number of dimers in the polymer varies, which leads to the formation of HA molecules of different molecular weights and lengths - 1x105-107 Da (2-25 μm), which, accordingly, have different biological effects.
HA is a highly hydrophilic substance that affects the movement and distribution of water in the dermal matrix. Thanks to this property, our skin, normally and in youth, has high turgor and resistance to mechanical pressure.
HA easily forms secondary hydrogen bonds both within one molecule and between neighboring molecules. In the first case, they ensure the formation of relatively rigid spiral structures. In the second, association with other HA molecules and nonspecific interaction with cell membranes occurs, which leads to the formation of a network of polysaccharide polymers with fibroblasts included in it. Shorter molecules of proteoglycans (versican, lumican, decorin, etc.) “sit” on a long HA molecule, like on a thread, forming aggregates of enormous sizes. Extended in all directions, they create a scaffold, contributing to the stabilization of the ECM protein network and fixing fibroblasts in a specific matrix environment. Taken together, all these properties of HA endow the matrix with certain chemical characteristics - viscosity, density of “cells” and stability. However, the ECM network is a dynamic structure that depends on the state of the organism. For example, under conditions of inflammation, HA aggregates with proteoglycans dissociate, and the formation of new aggregates between newly synthesized HA molecules (renewed every 3 days) and proteoglycans is blocked. This leads to a change in the spatial structure of the matrix: the size of its cells increases, the distribution of all fibers changes, the structure becomes looser, the cells change their shape and functional activity. All this affects the condition of the skin, leading to a decrease in its tone.
In addition to regulating water balance and stabilizing the ECM, HA plays an important regulatory role in maintaining epidermal and dermal homeostasis. HA actively regulates dynamic processes in the epidermis, including keratinocyte proliferation and differentiation, oxidative stress and inflammatory response, maintenance of the epidermal barrier and wound healing. In the dermis, HA also regulates fibroblast activity and collagen synthesis. By remodeling the matrix, HA controls the functioning of cells in the matrix, influencing their availability to various growth factors and changing their functional activity. Cell migration and the immune response in tissue depend on the action of GC. Thus, changes in the distribution, organization, molecular weight and metabolism of GCs have significant physiological consequences.
Fibroblasts are the main type of cellular elements of the dermis. It is these cells that are responsible for the production of HA, collagen, elastin, fibronectin and many other intercellular matrix proteins necessary for the formation of connective tissue. Fibroblasts in different layers of the dermis differ both morphologically and functionally. Not only the amount of collagen they synthesize depends on the depth of their location in the dermis, but also the ratio of the types of this collagen, for example types I and III, as well as the synthesis of collagenase: fibroblasts in the deeper layers of the dermis produce less of it. In general, fibroblasts are very plastic cells, capable of changing their functions and physiological response and even differentiating into another cell type depending on the stimulus received. The role of the latter can be played by signaling molecules synthesized by neighboring cells and the restructuring of the surrounding ECM.
Causes and risk factors
Currently, several factors have been identified that may predispose to the development of squamous cell carcinoma. These include:
- Age. The disease almost never occurs in young people. The majority of patients are elderly people over 65 years of age.
- Light skin color and presence of freckles.
- Increased insolation. The conclusion about the influence of this factor was made due to the fact that this form of malignant tumor always appears on open areas of the body that are constantly exposed to sunlight. In addition, squamous cell skin cancer can occur at the site of severe sunburn.
- Mutation of the TP53 gene, which is responsible for suppressing tumor growth.
- The presence of precancerous formations and other pathological conditions of the skin (scar atrophy, radiation damage, tuberculous lupus, occupational diseases, lichen planus, etc.).
- The effect of carcinogens on the skin (arsenic, paraffin, kerosene, coal tar, etc.), which leads to inflammation and atrophy. As a result, the formation of focal proliferations occurs, which over time can degenerate into a malignant formation.
- Prolonged mechanical irritation or damage to the skin.
- The patient is immunosuppressed.
- Infection with human papillomavirus. The role of some of its types in the occurrence of skin cancer of the penis, anus, and vulva has been proven.
- There is scientific evidence of the development of this tumor in patients with psoriasis after receiving courses of PUVA therapy and photochemotherapy, as well as in patients after radiation therapy.
Determining the cause of squamous cell skin cancer is critical to assessing the risk of recurrence and metastatic spread. Thus, a malignant tumor that developed at the site of skin lesions by actinic keratosis metastasizes only in 0.5% of cases. At the same time, cancer that occurs on the scar has a much higher risk of spreading - up to 30%.
Book a consultation 24 hours a day
+7+7+78
Subcutaneous fat
Subcutaneous fat, or hypodermis, is the lowest layer of skin, located under the dermis. It consists of fat lobules separated from each other by connective tissue septa containing collagen and penetrated by large vessels. The main cells of fat lobules are adipocytes, the number of which varies in different areas of the body. Currently, PFA is considered not only as an energy depot, but also as an endocrine organ, the adipocytes of which are involved in the production of a number of hormones (leptin, adiponectin, resistin), cytokines and mediators that affect metabolism, insulin sensitivity, reproductive and immune functional activity. systems
Classification
There are several principles for classifying squamous cell skin cancer. According to the histological structure, there are 4 types of this neoplasm, and according to TNM staging - 4 stages, each of which reflects the prevalence of the process in the body.
According to histological classification, the following options are distinguished:
- The spindle cell type has a poor prognosis due to its rapid invasive growth as well as its tendency to metastasize and recur.
- Acantholytic type. Appears on skin affected by actinic keratosis.
- Verrucous squamous cell skin cancer is accompanied by symptoms of severe hyperkeratosis, which is clinically manifested by the formation of a horny growth (skin horn).
- The lymphoepithelial type consists of poorly differentiated cells. It is believed that this neoplasm is a tumor of the skin appendages, and not true squamous cell carcinoma.
The stage of development of this type of cancer is determined by the size of the primary tumor, the degree of invasion into the underlying tissue and the presence of distant metastases. The first stage corresponds to a formation less than 2 cm in size, the second and third - larger tumors with spread to nearby tissues, and the fourth - a lesion of any size with the presence of metastatic lesions.
Forecast
When squamous cell skin cancer measuring less than 2 cm is detected and adequate treatment is provided, the 5-year survival rate reaches 90%. If the tumor is larger and there is growth into the tissue, then this figure is reduced to 50%.
Tumors located on the skin of the periorbital region, external auditory canal, and nasolabial fold have a particularly unfavorable prognosis. With this localization, the tumor can grow into muscles and bones and can cause bleeding due to vascular damage, complicated by infections.
Diagnostic methods
Since the direct dependence of the effectiveness of the treatment on the stage of the malignant neoplasm at which it was discovered has long been proven, there are two levels of diagnosis of squamous cell skin cancer: early and late.
An early diagnosis is considered to be made at stages I-II. In this case, complete recovery of the patient is possible, provided that the correct treatment tactics are chosen. Late detection means diagnosis at stages III and IV. The prognosis is usually unfavorable due to the complexity or impossibility of surgical treatment.
The “gold standard” for diagnosing squamous cell skin cancer is a biopsy followed by histological examination. The immunohistochemical method is considered especially informative. Since the tumor is external and it is not difficult to obtain biomaterial for histology, the tumor is verified in 99% of cases.
The dermatoscopy method is also widely used. In this case, the presence of central keratin plugs, dilated and branched vessels on the surface speaks in favor of skin cancer.
For any form of squamous cell carcinoma, along with a thorough history and physical examination, a specialist must evaluate the condition of the lymph nodes. If the presence of metastatic foci is suspected, the main diagnostic method is fine-needle aspiration. It is also possible to prescribe additional imaging methods (ultrasound, radiography, CT, angiography) to identify regional and distant metastases.
Prevention
The main measure for preventing squamous cell skin cancer is the timely detection and treatment of precancerous conditions. In this regard, young people are recommended to be examined by a dermatologist every 3 years, and people over 40 years old - every year. If you detect any changes in the skin, you should also contact a specialist.
Foci of chronic inflammation on the skin must undergo adequate sanitation. You should also avoid repeated damage to the same skin area (rubbing, compression by tight clothing and shoes, injury during monotonous manual work).
It is important to maintain a sun regime and use a cream with a sunscreen component, and avoid visiting a solarium. When working with chemical reagents that are sources of occupational hazard, it is necessary to use personal skin protection.
Book a consultation 24 hours a day
+7+7+78