Are you constantly embarrassed by others and cover your face with your hair in the hope of hiding skin imperfections? With early diagnosis and treatment of acne, your face can become clear and radiant again.
If you want to smile at your reflection in the mirror again, rather than look away in embarrassment, then this article is a must-read.
Acne is defined as a chronic skin disorder in which hair follicles become blocked and/or inflamed. When bacteria attaches to pimples, infection occurs and blackheads form. There are several variants of the disease, and they range from mild to severe. Appears on the face, neck, chest and back area.
Acne itself can cause not only psychological discomfort to its owner, but also lead to scarring of the skin (post-acne).
How papules and pustules appear
The mechanism of pimple formation is very simple. Due to the increased secretion of sebum - sebum - the sebaceous gland duct is blocked. A sebaceous plug is formed, that is, a comedon; they can be open or closed. But if such a comedon is affected by the bacteria P. Acnes, then inflammation occurs; over time, the purulent contents break into the skin, spread, which leads to the formation of other papules, and with more severe inflammation, purulent pustules appear.
There are many reasons for such activity of the sebaceous glands, the most common being hormonal changes during puberty. Nutrition, stress, hygiene habits, and lifestyle also play a role.
Causes of acne
You've probably heard the misconception more than once that acne is the result of poor hygiene. In reality, it is a complex skin condition involving hormonal, dietary and hereditary factors, and for all these reasons and more, acne requires a holistic approach. Treatment largely depends on the severity of the disease. If you have acne, never use alcohol or sulfates in hopes of freeing your skin from the unpleasant disease.
Acne can appear for the following reasons:
- Hormonal imbalance. With increased testosterone production in men and women, intense accumulation of sebum occurs in the glands. This turns out to be a favorable environment for the development of bacteria. Increased testosterone production in women may be associated with ovarian dysfunction. During adolescence (10-18 years), the formation of the endocrine system and puberty occurs. Often at this age, boys and girls experience active production of testosterone, which is what causes acne.
- Disorders of the autonomic nervous system. Frequent stress, lack of sleep, fatigue, increased physical activity, endocrine changes in the body (for example, after childbirth) lead to an imbalance in the work of the sympathetic and parasympathetic parts of the autonomic nervous system. In this case, again, the human sebaceous glands work more intensively.
- Decreased immunity. The skin's natural defenses can be disrupted by bad habits, stress, poor diet, and abuse of ultraviolet rays. As a result, bacteria and fungi multiply, causing acne.
- Hereditary predisposition. If parents have had acne, then there is a high chance that their children will also suffer from this problem. An increased level of testosterone, the level of sensitivity of the sebaceous glands to the effects of sex hormones, a tendency to form defective sebaceous glands, and much more can be inherited.
- Dietary disorder. Floury and sweet foods, as well as sugar, which is found in almost all foods, lead to the development of large amounts of insulin. As a result, the production of male sex hormone increases. And this, as we have already learned above, leads to increased production of sebum. The abundance of unhealthy fats in the body leads to the development of bacteria, which cause acne on the body and face.
- Diseases of the gastrointestinal tract, pathologies of the endocrine system. Acne is often a symptom of internal diseases. For example, diseases of the digestive system lead to the fact that food is not fully absorbed and stagnates. Acne is most often formed due to pathologies such as dysbiosis, constipation, irritable bowel syndrome, acute and chronic gastritis, and stones in the bile ducts.
- Incorrect cosmetic care. This includes failure to comply with personal hygiene rules and the use of low-quality decorative cosmetics. On the contrary, if the skin is constantly subjected to cleansing, it loses its natural protection and the acid-base balance is disturbed. As for low-quality cosmetics: viscous products that contain oils and glycerin are considered especially dangerous. Such cosmetics clog pores and create a microfilm on the surface of the skin that impedes breathing.
Acne
Acne is a disease in which papules, pustules, and comedones appear on the face and body (several follicles are affected at once). The inflammation is widespread, often the pimples are painful to touch, and as soon as one goes away, others appear. If a person has only comedones - white and blackheads, then we are talking about a non-inflammatory type of acne. And if there are papules and pustules, cysts, this is an inflammatory type. Pustules on the face should not be pressed, this will only worsen the situation; the contents may not break out, but subcutaneously.
It is worth saying that papules and pustules can appear not only as part of acne, for example, papular dermatosis with sterile papules is sometimes found, that is, P. Acnes is not detected in them, but acne is still the most common cause. Papular rashes also occur with psoriasis.
Acne treatment methods
If inflamed rosacea appears on your face and you feel a strong tingling sensation, then you should
Seek advice from our trusted specialists! Since even simple acne can develop into a more unpleasant disease - rosacea.
Doctors will be able to provide all the important information on combating pathology and will carry out safe procedures in the shortest possible time. With timely diagnosis and treatment, your face will become clear and radiant again.
For a long time there was no most effective and rapid treatment for the disease. As a rule, an integrated approach is always used. It involves the work of several specialists at once: a dermatologist, a nutritionist, a surgeon. Treatment occurs in several stages:
- prevent the formation of comedones;
- clear clogged ducts;
- stop the proliferation of bacteria;
- reduce sebum secretion;
- cure inflammation on the skin.
Those with this unpleasant disease took antibiotics, used ointments, and followed a diet. This approach did not always help, but could only do harm. In modern cosmetology, a new effective means for treating acne has appeared - light and laser technologies.
How to treat papules and pustules
Now that we have found out what papules and pustules are, the question arises whether they need to be treated. In this case, everything depends on their number and frequency of occurrence. If they are isolated and rarely appear on the face and body, for example, due to hormonal changes during the menstrual cycle, then there is no need to worry. You can simply choose suitable care cosmetics from a cosmetologist and cleanse your face efficiently. But if there are a lot of rashes, they can merge together and form spots; papules and pustules should be treated by a dermatologist.
Treatment of acne, papules and pustules is complex.
Lifestyle adjustments and adherence to doctor's recommendations are required. A non-hormonal ointment is used as a local remedy, which does not cause withdrawal effects in the future. Before treatment, the doctor will prescribe tests for hormones, the content of certain vitamins and a general blood test. This way you can choose an individual treatment plan. June 23, 2020
Author of the article: dermatologist Mak Vladimir Fedorovich
© S.V. KLYUCHAREVA1, A.V. KARPOVA2,3, K.V. NOZDRIN3
1 – Federal State Budgetary Educational Institution of Higher Education “North-Western State Medical University named after. I.I. Mechnikov" of the Ministry of Health of Russia, St. Petersburg, Russia; 2 – Federal State Autonomous Educational Institution of Higher Education “Russian Peoples' Friendship University”, Moscow, Russia; 3 – JSC “Retinoids”, Moscow, Russia.
Summary
The high prevalence of acne throughout the world and in Russia, the impact that this disease has on the quality of life of patients, the role of numerous environmental factors, dietary habits and lifestyle on the course of the disease determine the relevance of increasing the effectiveness of its treatment and the continuous search for affordable, convenient in the use and safety of medicines.
Purpose of the study.
To demonstrate the high effectiveness and safety of a solution containing 0.025% isotretinoin in an alcohol-glycol base in patients with papulopustular acne.
Materials and methods.
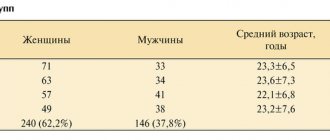
88 patients with papulopustular acne aged from 18 to 47 years were observed. In group 1 (n=48), patients were prescribed an external preparation containing 0.025% isotretinoin 1-2 times a day for 4-6 weeks. Patients of group 2 (n=40) received external therapy with a cream containing 0.1% adapalene, according to the instructions, for a total duration of up to 12 weeks.
Results and conclusion:
After 12 weeks, the number of papules and pustules in patients of group 1 became less than in patients of group 2 (p
Keywords:
acne, papulopustular form, topical isotretinoin, 13-cis-retinoic acid, alcohol-glycol base.
Information about the authors:
Klyuchareva S.V.
— https://orcid.org/0000-0003-0801-6181
Karpova A.V.
— https://orcid.org/0000-0003-4528-1013
Nozdrin K.V.
— https://orcid.org/0000-0002-2943-3585
Introduction
The high prevalence of acne throughout the world and in Russia, the impact that this disease has on the quality of life of patients, the role of numerous environmental factors, dietary habits and lifestyle on the course of the disease determine the relevance of increasing the effectiveness of its treatment and the continuous search for affordable, convenient in the use of safe medicines [1-4].
According to the American Academy of Dermatology, in the United States alone, more than 50 million people suffer from acne in one form or another, mostly teenagers and young adults, but also adult acne (acne tarda) [1]. The study of the pathogenesis of the disease allows us to identify several key links: hypersecretion of sebum, follicular hyperkeratosis, colonization by Cutibacterium acnes (formerly Propionibacterium acnes), as well as complex inflammatory mechanisms caused by immune reactions [1, 4, 5]. Accordingly, drugs prescribed to patients with acne should reduce excessive sebum secretion, normalize the process of cell keratinization, reduce the concentration of C. acnes and influence the inflammatory process.
The choice of therapy for patients with acne is determined by the clinical form and severity of the disease, skin type, gender, age, concomitant diseases and the effectiveness of previous treatment [1, 6, 7]. Taking into account the clinical picture of the disease, comedonal, papulopustular, nodular and conglobate acne, as well as mild, moderate and severe severity, are distinguished [1, 7]. For comedonal and papulopustular acne of mild to moderate severity, Russian and foreign communities recommend external therapy, mainly with topical retinoids, as monotherapy or in combination with external antibacterial drugs [1, 7, 8].
Topical retinoids are vitamin A derivatives that bind to various nuclear receptors of retinoic acid and have comedolytic, sebostatic, anti-inflammatory and regenerating effects on the skin, normalize the processes of keratinization and epidermal differentiation [8-11]. Currently on the Russian market, retinoids for topical use are represented by a synthetic analogue of retinoic acid (retinoid-like compound) - adapalene, including in combinations with benzoyl peroxide, clindamycin and metronidazole (France, Switzerland, India, Russia), and a biologically active form of vitamin A — isotretinoin (Russia) [12]. Given the prevalence of the disease at a young age, it seems important to have a range of affordable, budget-friendly medications for external therapy containing retinoids, such as Retinoic ointment and Retasol.
Retasol is a solution containing 0.025% isotretinoin in an alcohol-glycol base. Isotretinoin (13-cis-retinoic acid) inhibits the terminal differentiation of sebocytes, hyperproliferation of the epithelium of the sebaceous glands, reduces the production of sebum, normalizes its composition and facilitates its evacuation, reduces the inflammatory reaction around the glands. Ethyl alcohol, which is part of Retasol, has a defatting, antiseptic and additional comedolytic effect, which increases the overall pharmacological effect of the drug [13].
The solution is indicated for adults and adolescents over 12 years of age with papulopustular and comedonal forms of acne. It is also used in the treatment of rosacea (for small amounts of rashes), perioral and seborrheic dermatitis. The solution is applied with a cotton swab to previously cleansed skin (after washing or wiping with an alcohol-free tonic) 2 times a day. Duration of treatment is from 4 to 12 weeks.
The purpose of the study was to demonstrate the high effectiveness and safety of the drug Retasol in patients with papulopustular acne.
Material and methods
We observed 88 patients with papulopustular acne, of which 18 (20.5%) were men and 70 (79.5%) women aged 18 to 47 years. The duration of the disease ranged from several months to 7 years. Distribution by severity of the disease: mild in 33 (37.5%) patients (Fig. 1), moderate in 34 (38.6%) (Fig. 2), severe in 21 (23.9%) (Fig. 3 ). In all patients, the rashes were widespread and localized on the skin of the face, chest and upper back.
Fig 1.
Patient E., 19 years old. The onset of the disease is at the age of 18. Diagnosis: “mild acne” There are single papules and pustules in the facial area. There is a history of treatment with cosmetics, without effect.
Fig 2.
Patient K., 27 years old. The onset of the disease was at the age of 22. Diagnosis: “moderate acne.” The disease recurred monthly; there was a history of diseases of the gastrointestinal tract and ENT organs. In the facial area there are single papules, multiple pustules and atrophic scars.
Patients are divided into two groups so that the ratio of degrees of disease severity in each group is the same. In group 1 (n=48), patients were prescribed external Retasol 1-2 times a day for 4-6 weeks. As the rashes regressed and the oiliness of the skin decreased, patients were prescribed Retinoic ointment 0.1% for external use 1-2 times a day for a total duration of up to 6-8 weeks. In the future, to maintain the effect, it was recommended to use Retinoic ointment 0.05% once a day for a total duration of up to 6 months.
Patients of group 2 (n=40) received external therapy with a cream containing 0.1% adapalene, according to the instructions, for a total duration of up to 12 weeks.
Exclusion criteria: a history of allergic reactions to the components of the drugs, contraindications for use, the general serious condition of the patient due to somatic pathology, which does not allow the patient to comply with the necessary regimen, lack of willingness to cooperate on the part of the patient, inability to comply with the conditions of the protocol.
In order to prevent possible side effects, patients were advised to check drug tolerance on a separate area of the skin (neck), avoid sun exposure, and not use sulfonamides and phenothiazine derivatives during treatment.
The effectiveness and tolerability of therapy were assessed once a month for 12 weeks, which included assessment of clinical examination data and subjective feelings (complaints) of patients, photography, counting the number of inflammatory elements (papules and pustules), assessment of the dermatological quality of life index (DIQL scale), global assessment of therapeutic effect (GOTE) using a ranking method in points (3 points - excellent result, 2 - good, 1 - satisfactory, 0 - unsatisfactory). Long-term results were assessed 12 months from the start of treatment.
Statistical processing of the data was performed using application packages Statistica 10. To determine the dynamics of the number of inflammatory elements, a rank analysis of variance was carried out according to Friedman, and the rate of decrease (increase) in the number of inflammatory elements as a percentage of the initial level was calculated based on group average values.
The study was approved by the local ethics committee.
Fig 3.
Patient A., 24 years old. The onset of the disease was at the age of 17. Diagnosis: “moderate acne.” The process on the skin in the form of closed comedones was long-term, but the exacerbation occurred relatively acutely; within six months, papules and pustules appeared on the face, painful conglobates formed in the bridge of the nose and forehead, which persisted for 3 months. There is a history of diseases of the endocrine system and menstrual irregularities. In the facial area there are single papules and multiple pustules, in the frontal part there are dense infiltrates.
results
The initially formed groups of patients were homogeneous in terms of the severity of the inflammatory process (rpapules = 0.65; rpustules = 0.88). After 12 weeks, the number of papules and pustules in group 1 became smaller compared to group 2 (p
Fig 4.
Reducing the number of papules during treatment.
Fig 5.
Reducing the number of pustules during treatment.
As can be seen from table.
1, already at the end of the first month of treatment, significant positive dynamics were noted: a decrease in papules by 29.7 and 25% and pustules by 46.7 and 35% in groups 1 and 2, respectively. After 12 weeks, a decrease in papules by 80 and 60% and pustules by 93.3 and 76.7% was observed. Table 1.
Estimation of the number of inflammatory elements
| Treatment day | Group 1 (n=48) | Group 2 (n=40) | ||||||
| Papules | Pustules | Papules | Pustules | |||||
| abs. | % | abs. | % | abs. | % | abs. | % | |
| 0th (before treatment) | 960 | 100 | 720 | 100 | 800 | 100 | 600 | 100 |
| 30th | 675 | 70,3 | 384 | 53,3 | 600 | 75,0 | 390 | 65,0 |
| 60th | 480 | 50,0 | 192 | 26,7 | 480 | 60,0 | 240 | 40,0 |
| 90th (12 weeks) | 192 | 20,0 | 48 | 6,7 | 320 | 40,0 | 140 | 23,3 |
| 360th | 30 | 3,1 | 0 | 0 | 162 | 20,3 | 7 | 1,2 |
Fig 6.
Histogram of the median number of inflammatory elements.
Table 2.
Analysis of the strength of the influence of the used therapy method on the quality of life of patients in the comparison groups according to the results of DIQ before and after treatment and GOTE (M±p1)
| Chapter | Points max | Comparison groups | Significance of differences when comparing groups | ||||||
| Group 1 (n=48) | Group 2 (n=40) | pdo | pafter | ||||||
| before | after | p | before | after | p | ||||
| 1. Symptoms and sensations | 5 | 2,3±1,2 | 1,1±0,4 | 2,3±1,3 | 1,6±1,1 | 1,0 | 0,0096 | ||
| 2. Daily activities | 3 | 2,1±0,8 | 1,2±0,5 | 1,8±0,7 | 1,2±0,4 | 0,060 | 0,90 | ||
| 3. Rest (leisure) | 3 | 1,6±0,6 | 0,8±0,5 | 1,5±0,6 | 1,3±0,5 | 0,67 | |||
| 4. Work and study | 3 | 1,4±0,6 | 0,7±0,5 | 1,4±0,6 | 0,8±0,5 | 0,84 | 0,47 | ||
| 5. Interpersonal relationships | 5 | 3,2±1,1 | 1,2±0,6 | 3,2±1,1 | 2,5±1,3 | 0,89 | |||
| Sum of points | — | 10,4±3,3 | 5,0±2,2 | 10,1±3,3 | 7,4±2,9 | 0,68 | |||
| 6. Treatment effectiveness - GOTE | 3 | 2,2±0,8 | 3,0±0,2 | 2,0±0,7 | 2,2±0,5 | 0,0034 | 0,16 | 0,0000 | |
Note: p is the significance of the Student's test for related samples when comparing indicators before and after treatment in each group; pbefore is the significance of Student’s test for independent groups when comparing indicators in groups 1 and 2 before treatment, pafter is after treatment.
Observation of long-term results 12 months after the start of treatment demonstrated the high effectiveness of the therapy with the transition to long-term clinical remission: there was a decrease in papules by 96.9 and 79.7% and pustules by 100 and 98.8% in the 1st and 2nd groups respectively. In group 1, regression of rashes persisted in 97% of patients, in group 2 - in 77% (see Fig. 4-9).
Analysis of examination data and patient complaints made it possible to assess the tolerability of therapy in both groups. It should be noted that the external use of retinoids is always accompanied by dermatological reactions (irritant dermatitis), which do not require specific therapy and in most cases go away on their own after correcting the dosage regimen and using moisturizing cosmetic products. The parameters assessed (symptoms and complaints) included a burning sensation (tingling), itching, flushing, swelling and dryness of the skin.
Fig 7.
Patient E., 19 years old. 1 month after therapy with Retasol 2 times a day. The effectiveness of treatment was 90%.
During a visit 1 month after the start of treatment, an increase in burning sensation was noted by 6.2 and 7.5% of patients in groups 1 and 2, respectively, an increase in skin dryness - 22.9 and 32.5%, an increase in itching - 4 ,1 and 10%, increased swelling - 2.1 and 2.5%. At the same time, a decrease in hyperemia was observed in 25.1 and 27.5% of patients in groups 1 and 2, respectively.
At the end of the 12-week course of treatment, side effects in the form of burning sensation, itching, swelling were insignificant, respectively 4.1; 10.4; 4.1% in group 1 and 5.0; 17.5; 5.0% in the 2nd. Dry skin at the end of treatment persisted in 8.2 and 12.5% of patients in groups 1 and 2, respectively, which demonstrates better tolerability in group 1.
An analysis of the strength of the influence of the treatment methods used on the quality of life of patients in groups according to the results of DIQ before and after treatment and GOTE (M±p) is presented in table. 2. When assessing the global therapeutic effect (GOTE), reliable positive results were obtained: already on the 30th day of treatment in group 1, half of the patients noted the good effectiveness of the drug - 2.1 points, and after 90 days, almost all rated the therapeutic effectiveness at 2 .9 points, versus 1.9 and 2.1 points in the 2nd group.
Assessment of patients’ quality of life indicators based on the results of treatment demonstrated a significantly greater severity of the positive effect of therapy in group 1 compared to group 2, the data are presented in table. 3.
Figure 8.
Patient K., 27 years old. 1 month after therapy with Retasol 2 times a day. The effectiveness of treatment was 80%.
Figure 9.
Patient A., 24 years old.
1 month after therapy with the drug Retasol 2 times a day. The effectiveness of treatment was 80% (papules and pustules resolved, the size of infiltrates decreased). Table 3.
Assessment of quality of life indicators of patients based on treatment results, Me (Q1; Q3)
| Index | 1st group | 2nd group |
| Symptoms and sensations: | ||
| before treatment | 2 (1; 3) | 2 (1; 3) |
| after treatment | 1 (1; 1) | 1 (1; 2) |
| Daily Activities: | ||
| before treatment | 2 (2; 3) | 2 (1; 2) |
| after treatment | 1 (1; 1) | 1 (1; 1) |
| Rest (leisure): | ||
| before treatment | 2 (1; 2) | 1 (1; 2) |
| after treatment | 1 (0; 1) | 1 (1; 1) |
| Work and study: | ||
| before treatment | 1 (1; 2) | 1 (1; 2) |
| after treatment | 1 (0; 1) | 1 (0; 1) |
| Interpersonal relationships: | ||
| before treatment | 3 (3; 4) | 3 (3; 4) |
| after treatment | 1 (1; 1) | 2 (1; 3) |
| Treatment effectiveness: | ||
| on the 30th day | 2 (2; 3) | 2 (2; 2) |
| on the 90th day | 3 (3; 3) | 2 (2; 2) |
The greatest statistical dispersion is observed in the indicators “symptoms and sensations” in both the 1st and 2nd groups. At the same time, there was a more pronounced dynamics of improvement in indicators of the quality of life of patients in the 1st group compared to the 2nd, primarily in such a parameter as interpersonal relationships (decrease from 3 (3; 4) to 1 (1; 1) points ), as well as a significant increase in the “treatment effectiveness” indicator from 2 (2; 3) to 3 (3; 3) points.
After completion of the course of treatment, an analysis of the quality of life of patients demonstrated a decrease in all parameters in both groups: according to the sum of points in group 1 before treatment, the indicator was 10.4 points, after 90 days - 5 points, which allowed patients to significantly improve interpersonal relationships and increase efficiency work and study. In group 2, these indicators were 10.1 and 6.1 points, respectively. Thus, the DIQL in group 1 improved by 52%, and in group 2 by 40%, which indicates a positive impact of therapy on the quality of life of patients. At the same time, in group 1 the indicators were higher by 12%.
Conclusion
The results obtained during the study demonstrate the high effectiveness and tolerability of the drug Retasol in the treatment of papulopustular acne. Side effects such as itching, burning, swelling, hyperemia and dry skin were minor and less pronounced than in group 2.
Persistent, long-term clinical remission and a significant increase in the quality of life of patients allows us to recommend this drug as an affordable, budget-friendly, highly effective remedy for the treatment of acne as monotherapy or combination therapy together with Retinoic ointment according to the scheme: externally Retasol 1-2 times a day for 4 —6 weeks, then externally Retinoic ointment 0.1% 1-2 times a day for a total duration of up to 6-8 weeks, then externally Retinoic ointment 0.05% once a day for up to 6 months to maintain the effect.
Literature
- Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, Bowe WP, Graber EM, Harper JC, Kang S, Keri JE, Leyden JJ, Reynolds RV, Silverberg NB, Stein Gold LF, Tollefson MM, Weiss JS, Dolan NC, Sagan AA, Stern M, Boyer KM, Bhushan R. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945-973.e33. Epub 2016 Feb 17. Erratum in: J Am Acad Dermatol. 2020;82(6):1576. PMID: 26897386.
- Kucharska A, Szmurło A, Sińska B. Significance of diet in treated and untreated acne vulgaris. Postepy Dermatol Alergol. 2016;33(2):81-86. Epub 2016 May 16. PMID: 27279815; PMCID: PMC4884775.
- Cooper AJ, Harris VR. Modern management of acne. Med J Aust. 2017;206(1):41-45. PMID: 28076744.
- Li X, He C, Chen Z, Zhou C, Gan Y, Jia Y. A review of the role of sebum in the mechanism of acne pathogenesis. J Cosmet Dermatol. 2017;16(2):168-173. Epub 2022 May 29. PMID: 28556292.
- Platsidaki E, Dessinioti C. Recent advances in understanding Propionibacterium acnes (Cutibacterium acnes) in acne. F1000Res. 2018;7:F1000 Faculty Rev-1953. PMID: 30613388; PMCID: PMC6305227.
- Gollnick HP, Bettoli V, Lambert J, Araviiskaia E, Binic I, Dessinioti C, Galadari I, Ganceviciene R, Ilter N, Kaegi M, Kemeny L, López-Estebaranz JL, Massa A, Oprica C, Sinclair W, Szepietowski JC, Dréno B. A consensus-based practical and daily guide for the treatment of acne patients. J Eur Acad Dermatol Venereol. 2016;30(9):1480-1490. Epub 2016 May 14. PMID: 27177989.
- Federal clinical guidelines. Dermatovenereology 2015: Skin diseases. Sexually transmitted infections. 5th ed., revised. and additional M.: Business Express; 2016;9-27.Federal'nye klinicheskie rekomendatsii. Dermatovenerologiya 2015: Boleznikozhi. Infektsii, peredavaemye polovym putem. 5th izd., pererab. i dop. M.: Delovoi ekspress; 2016;9-27. (In Russ.).
- Nast A, Dréno B, Bettoli V, Bukvic Mokos Z, Degitz K, Dressler C, Finlay AY, Haedersdal M, Lambert J, Layton A, Lomholt HB, López-Estebaranz JL, Ochsendorf F, Oprica C, Rosumeck S, Simonart T , Werner RN, Gollnick H. European evidence-based (S3) guideline for the treatment of acne - update 2016 - short version. J Eur Acad Dermatol Venereol. 2016; 30(8):1261-1268. PMID: 27514932.
- Kolli SS, Pecone D, Pona A, Cline A, Feldman SR. Topical Retinoids in Acne Vulgaris: A Systematic Review. Am J Clin Dermatol. 2019;20(3):345-365. PMID: 30674002.
- Latter G, Grice JE, Mohammed Y, Roberts MS, Benson HAE. Targeted Topical Delivery of Retinoids in the Management of Acne Vulgaris: Current Formulations and Novel Delivery Systems. Pharmaceutics. 2019;11(10):490. PMID: 31554188; PMCID: PMC6835300.
- Yeh L, Bonati LM, Silverberg NB. Topical retinoids for acne. Semin Cutan Med Surg. 2016;35(2):50-56. PMID: 27416308.
- https://grls.rosminzdrav.ru
- Burylina OM, Karpova AV. Kosmetologiya. Klinicheskoye rukovodstvo. M. 2019;83, 114-115.
Seal
Acne treatment time frame
Treatment of chronic deviation depends on the severity of the course. Duration is determined by the characteristics of the patient. Advanced cases require complex treatment for months or years. It is necessary to take medications made with isotretinoin, followed by the use of external components. After the end of the therapeutic method, a rehabilitation period begins, social adaptation, and organization of proper care. Preventing the development of new pathology and activation of inflammatory processes.
Symptoms
Structurally, the nodules are bandless formations of various colors. They can be red, gray, brown. Some papules have a noticeable bubble on the surface; they are called serous. Red formations are usually inflammatory in nature.
The size of a single growth can vary: from the head of a pin to the size of a nail. Large papules are called plaques.
In addition to the external defect, papules can cause physical discomfort, causing itching, inflammation, burning sensation and irritation of the skin. When pressed, the formations turn pale.
The appearance of unpleasant growths on the skin always makes you want to get rid of them as quickly as possible. But not all patients seek help from a doctor, and many self-medicate. Such therapy not only does not eliminate the defect in appearance, but can serve as a favorable condition for the further spread of infection.
In addition, papules can be symptoms of serious diseases that require immediate treatment.