Causes of stomatitis
In children, as in adults, stomatitis can be caused by viruses, fungi, bacteria, allergies and injuries. About six months after birth, the child loses the immunity received from the mother, the protective power of the immune system changes, and the child’s body becomes more susceptible to infections. The oral mucosa in children is more delicate and easier to injure; children also more often “bite” their cheeks after dental treatment due to a temporary loss of sensitivity after anesthesia, which causes traumatic stomatitis.
Children are not always motivated to brush their teeth, so poor hygiene can also cause stomatitis.
With the following diseases, stomatitis is observed in children much more often: chronic tonsillitis, diabetes mellitus, heart defects, chronic hepatitis.
Causes and risk factors
The mucous membrane of the child's oral cavity is often injured. The appearance of ulcers can be caused by temperature effects (hot food and drinks), biting the inner surface of the cheeks or lips; damage by sharp edges of the filling, braces or the tooth’s own tissues in case of chipped enamel. Normally, the immune response allows the pathological process to be quickly eliminated, the mucous membrane heals, and bacteria do not have time to cause severe inflammation and ulceration.
Weakened children's immunity cannot cope with this task, which leads to the development of aphthous stomatitis. A small number of opportunistic bacteria that populate the oral cavity begin to actively multiply. Often the disease occurs against the background or as a result of a severe infection: influenza, ARVI, acute tonsillitis, infectious mononucleosis, etc.
Main risk factors:
- food allergies, allergic reactions to hygiene products, such as toothpaste;
- deficiency of vitamins and microelements due to a strict diet or impaired digestion of food;
- hereditary predisposition;
- foci of infection in the oral cavity: caries, chronic periodontitis, periodontitis, gingivitis;
- frequent respiratory diseases;
- severe systemic diseases: pathologies of the endocrine system, blood vessels, metabolic disorders, etc.
Ask a Question
Classification of HRAS (chronic recurrent aphthous stomatitis)
| CLASSIFICATION | A COMMENT | ||
| classification: | According to the degree of damage to the mucous membrane: | a comment: | 1) Superficial (catarrhal, fibrinous) 2) Deep (ulcerative, necrotic) |
| classification: | According to the clinical course: | a comment: | 1) acute 2) chronic |
All types of stomatitis occur in children, but the most common are: herpetic, candidal and traumatic stomatitis.
Acute herpetic stomatitis
It occurs most often, and mainly affects children from 10 months to 3 years.3 The appearance of rashes is preceded by inflammation of the lymph nodes.
With a mild form
In acute herpetic stomatitis, the temperature rises to 37-37.5°C, the general condition is satisfactory, slight swelling and redness may occur on the gums, then up to six blisters appear, which burst with the formation of painful aphthae surrounded by a red rim.
Afta is a round-shaped erosion. Aphthae may merge together. The rash appears once, and after 1-2 days the erosion gradually heals.
Moderate form
Acute herpetic stomatitis is characterized by deterioration of the child’s well-being, weakness, and headache. The child is capricious, has no appetite, the lymph nodes are enlarged and painful, the temperature rises to 38-39°C, the symptoms resemble ARVI. The oral mucosa is swollen, reddened, rashes appear (bubbles, then erosions) of 10-15 pieces, and often there are rashes on the face. Salivation increases, and gingivitis appears (inflammation of the gums, accompanied by bleeding). The rash may appear several times, i.e. after the old ones heal, new ones appear. Healing of erosions takes up to 4-5 days. Bleeding gums and swollen lymph nodes persist for some time after the erosions have healed.
Severe form
It begins as an acute respiratory viral infection, there is pain in the muscles, joints, tachycardia and bradycardia (increased and slow heartbeat), and nosebleeds may even be observed. In this form, the temperature is high up to 40°C, gingivitis is pronounced, the mucous membrane is bright red, swollen, the child’s lips are dry, the mucous membrane of the eyes is swollen, reddened. The rashes constantly appear again, their number can reach 100. Rashes often appear around the mouth, on the eyelids, on the mucous membranes of the eyes, between the fingers, on the earlobes. Simple gingivitis turns into ulcerative (a more severe form of gum inflammation, with the formation of ulcers), salivation increases, and bad breath appears. Recovery is long and hospitalization is often required.
Enteroviral vesicular stomatitis (arm - leg - mouth)
Caused by enteroviruses. It also occurs in adults, but in 95.7% of cases children are affected.6 It is characterized by seasonal occurrence (summer - autumn) and group incidence.4 It is observed mainly in children under 10 years of age. Vesicular stomatitis is contagious, so it is recommended to use separate utensils and hygiene products. Characteristics for this disease: temperature 37.5-38, weakness, headache, muscle pain, rash on the palms, soles, as well as blisters on the hard palate and pharynx, which then turn into erosions that are almost not painful.
Course of herpetic sore throat
The diagnosis of herpetic sore throat can be made by an otolaryngologist, therapist or pediatrician after examining the patient and clarifying his complaints. To monitor changes characteristic of a viral infection, the doctor may prescribe a general blood test, and to confirm enteroviral sore throat, a specialist may prescribe a pharyngeal smear and a blood test for specific antibodies. The pathogen can also be detected in stool or inflammatory fluid that is released from vesicles1,4.
Manifestations of herpetic sore throat can go away on their own in less than 10 days. But in any case, at the first symptoms of the disease, you should definitely consult a doctor. You cannot self-medicate2,3.
In some cases, herpetic sore throat can cause complications from the nervous system. In this case, 1 appears:
- severe spasm of the neck muscles, due to which the child cannot bend his head;
- weakness of the muscles of the limbs;
- disturbance of consciousness.
A severe complication of herpetic sore throat is damage to the soft membranes of the brain, brain and spinal cord1,3.
Newborns are at highest risk of developing complications, so they need careful treatment and care3. It is important to maintain hydration and give your child enough fluids1.
Up to contents
Acute pseudomembranous candidal stomatitis (thrush)
Acute pseudomembranous candidal stomatitis (thrush) occurs:
- Light shape
- Medium-heavy forms
- Severe form
The main symptom of the disease is a white or yellow coating.
With a mild form
The plaque is located in islands, most often on the tongue and cheeks. Children are restless, sleep poorly, and suck the breast sluggishly. Older children may complain of a burning sensation. The plaque is easily removed; underneath there is a bright red mucous membrane. The disease lasts no longer than 7 days.5
Moderate form
The plaque is located on the cheeks, tongue, hard palate, and mucous membranes of the lips. Under the plaque, erosions form, which sometimes bleed. The plaque is more difficult to remove. Lymph nodes are sometimes enlarged and painful. The duration of the disease is 10-15 days, there are relapses.
Moderate form
The plaque is dirty gray, almost cannot be removed, and is located on the tongue, cheeks, soft palate, tonsils, pharynx, and mucous membranes of the lips. Cheilitis appears in the corners of the mouth - inflammation of the lips. The oral mucosa is dry and inflamed. The child’s health is impaired, the child refuses to eat, and the temperature rises. Lesions in the genital area, neck folds, and between the fingers are also common. The disease is long-term, with frequent relapses.
Forms of the disease
According to the ICD, aphthous stomatitis is assigned code K12.0. There are two forms of the disease - acute and chronic. The second is characterized by frequent relapses and may be a consequence of inadequate or untimely treatment of acute inflammation.
An acute disease is characterized by severe symptoms. It begins quickly, severe pain occurs at the site of mucosal damage, and the child may refuse to eat. In some cases, body temperature rises, weakness and lethargy occur.
The chronic form is characterized by a sluggish course; the child’s general well-being does not suffer. The disease can recur up to several times a year.
Bacterial stomatitis in children
Necrotizing ulcerative stomatitis is more common in weakened children and is caused by fusobacteria and spirochetes. May be a sign of periodontal disease (progressive destruction of periodontal tissue). It is characterized by the appearance of painful ulcers, weakness, gingivitis (inflammation of the gums), enlarged and painful lymph nodes, difficulty eating, speaking, and bad breath.
Often, erosions in traumatic stomatitis can become infected through dirty hands, toys and other objects, then bacterial stomatitis develops, so it is important to pay attention to antiseptic treatment.
Traumatic stomatitis in children
A specific form of traumatic stomatitis in children is Bednar's aphthae . This is a traumatic erosion of the oral mucosa. In children, unlike adults, the mucosal epithelium consists not of four layers, but of two, so it is easily injured. The cause may be early teething, a rough nipple from the mother, or a long nipple on the bottle. Erosion is most often located in the middle of the palate or opposite the cutting edge of the teeth. The child begins to refuse food, cries, and sleeps poorly.
Traumatic stomatitis also occurs in children when wearing braces. Erosions have uneven edges, are painful, and are usually located on the mucous membrane of the cheeks and lips, less often on the tongue.
Features of treatment
To diagnose a disease, only a visual examination is often sufficient, but in some cases laboratory diagnostics are required to determine the causative agent of the inflammatory process and the sensitivity of bacteria to antibiotics. Treatment should be carried out by a dentist, and the treatment regimen is developed individually, taking into account test results, the age and well-being of the child, the causes of the disease, the area of mucosal lesions and other conditions.
If the question of how to treat aphthous stomatitis in children is decided individually, then recommendations regarding eating behavior and hygiene are general for all cases. Such recommendations include the following:
- avoidance of too hot or cold drinks and foods;
- following a hypoallergenic diet;
- refusal of food that irritates the mucous membrane. This list includes fatty, salty and spicy foods, marinades, solid foods;
- adding pureed and soft foods to the menu. This includes cream soups, porridges, pre-boiled meat;
- drinking enough liquid;
- careful adherence to oral hygiene: using brushes with soft bristles, rinsing the mouth after each meal.
Local drug treatment consists of the use of such agents as:
- rinses or irrigation solutions (for children who do not yet know how to rinse their mouths) with an antiseptic effect;
- ointments and gels that stimulate the restoration of mucous membranes;
- drugs for pain relief and burning sensation.
It is important to test the product before use: apply a small amount to the crook of your elbow. If there is no redness, burning, or rash, we can say there is no allergy - the product can be used for treatment.
In some cases, systemic drug therapy is indicated. Your doctor may prescribe antihistamines to combat the allergic reaction and relieve swelling. In order to increase the resistance of the child's body, immunomodulators may be recommended. The decision on the need for antibacterial therapy is made in the case of an extremely severe course of the disease, a persistent increase in body temperature, and identification of a bacterial pathogen in a smear.
Elevated body temperature and pain are indications for symptomatic therapy. The doctor may recommend non-steroidal anti-inflammatory drugs in a dosage and form appropriate to the age of the young patient. Sometimes it is advisable to use suppositories if taking the medicine in the form of a tablet or syrup causes pain or anxiety.
Treatment of infants additionally includes disinfection of toys and teethers that the baby may put in his mouth. A nursing mother should pay attention to breast hygiene: thoroughly wash her breasts after feeding using warm water and special products.
Sometimes it is advisable to use folk remedies. Thus, rinsing the mouth with chamomile can soothe inflamed mucous membranes and speed up the healing process. However, it is important to remember that such prescriptions can only complement the main course of treatment. Don't forget to consult your doctor about the possibility of using them. Some herbs are strong allergens, so it is important to ensure that you are not hypersensitive to them.
Warming, the use of honey and alcohol tinctures are prohibited, as all this can lead to a worsening of the condition and lead to serious complications. It is better not to self-medicate, but to show the child to a qualified specialist.
Treatment of aphthous stomatitis in children usually takes no more than 7–12 days. It all depends on the state of the child’s immune system, the severity of inflammation, the number and depth of ulcers.
Drug-induced stomatitis
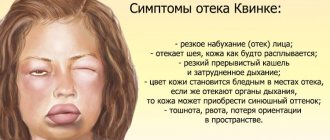
Occurs when there is an allergy to a drug. Often, allergies can occur to antibacterial, antimicrobial drugs, vaccines, iodine. The mucous membrane is red, swollen, the lips and tongue also often swell, blisters appear, which burst, leaving erosion. The gums are inflamed and bleed when touched. General manifestations are possible, such as urticaria, nausea, vomiting. In severe cases, anaphylactic shock occurs (an emergency condition manifested by decreased blood pressure, shortness of breath, fainting, suffocation), Quincke's edema (an atypical reaction of the body, manifested by rapid and severe swelling)
Both conditions are extremely dangerous and require immediate action and calling an ambulance!
Prevention of stomatitis in children
In children's groups, infections spread especially quickly. Therefore, if a child is infected with the herpes virus, he needs to stay at home until he recovers. Children who have been in contact with sick people should use antiviral ointments for 5 days.
If a pregnant woman has herpes or candidiasis, she should treat it before giving birth. If you have the herpes virus during the period of illness, you should use separate utensils, do not kiss children, and wear a mask.
Kindergartens and other preschool institutions must be cleaned and objects, including toys, must be treated with disinfectants.
To avoid allergic reactions, you should seek help from an allergist to identify existing allergies.
It is worth preventing a decrease in immunity; hardening works especially well in childhood. It is worth limiting your intake of fast carbohydrates, because... they create a favorable environment for the development of candidiasis. An important point is the proper nutrition of the child; regular intake of vitamins, especially vitamin C, is essential.
Tantum® Propolis
For children over 14 years of age , you can use Tantum® Propolis lozenges; they contain a lot of vitamin C, which will strengthen the immune system, and propolis has an anti-inflammatory effect, preventing the occurrence of infections.7
Find out more
Prevention of Bednar's aft is preparing the breasts for feeding, using special creams to soften the skin, prevent cracks, and it is also worth choosing the right bottle. In case of injury due to braces, you need to use orthodontic wax; here it is important to prevent the wounds from becoming infected, so it is better to treat them with antiseptic solutions and sprays.
Tantum® Verde spray will relieve pain at the site of injury and its antiseptic effect will prevent infection.8,9
Diagnosis and treatment of oral lesions in newborns
Infants often develop lesions in the oral cavity, which cause discomfort for themselves and cause anxiety for their parents. The most common disorders and diseases include congenital and neonatal teeth, various oral mucous cysts in newborns, ankyloglossia and congenital epulis of the newborn. In this article we will look at the features of diagnosis and treatment of this type of disorder and try to give readers an idea of the correct methods of treating and counseling young patients and their parents.
During their practice, doctors encounter various cases of oral lesions in newborns: from physiological characteristics associated with the development of the child to cancerous tumors. Awareness of such disorders plays an important role in correct diagnosis, counseling and treatment planning. The purpose of this article is to inform healthcare professionals about the diagnosis and treatment of the most common oral disorders in newborns.
Congenital and neonatal teeth
The eruption of the first baby tooth occurs approximately six months after the baby is born. But some babies reach this age already having congenital (the baby is born with them) or neonatal (erupted during the first month of life) teeth in their mouths.
Almost all congenital teeth (about 90%) erupt in the incisor area of the lower jaw. As a rule, they have the correct shape, but may be characterized by discoloration and an uneven surface. Their typical distinguishing feature already during the development period is increased mobility due to the absence or short length of roots. Most of the congenital teeth are subsequently included in the row of twenty primary teeth, but about 10% of them turn out to be supernumerary. Congenital teeth are rare: one case in two to three thousand births of healthy children, and, as a rule, this deviation is random. But in some cases, the appearance of congenital teeth can be a symptom of certain syndromes, malformations and gingival tumors.
If the congenital tooth turns out to be supernumerary and is not included in the row of baby teeth (this can be determined using an x-ray) or interferes with breastfeeding, it is recommended to remove it. Excessively mobile teeth should also be removed to prevent possible aspiration. In addition, congenital teeth can cause traumatic ulceration of the ventral surface of the tongue (Rigi-Fede syndrome), but this disorder is not an indication for tooth extraction and is cured by smoothing the rough cutting edge of the congenital tooth.
Newborn cysts
To refer to oral mucous cysts in newborns, many terms are used that replace each other, causing some confusion. But, based on the different histogenesis of the lesions, all of them can be divided into two categories: palatal and gingival.
Palatal cyst of a newborn
The palatal plates are bilateral rudimentary processes that join along the midline of the oral cavity in the eighth week of fetal development to form the hard palate. They also fuse with the nasal septum, resulting in complete separation of the oral and nasal cavities. In this case, the connective epithelial lining between the plates is destroyed under the action of enzymes, providing the possibility of fusion of the connective tissue. Neonatal palatal cysts, or Epstein's pearls, form from epithelial inclusions along the fusion line of the palatine plates. This disorder is characterized by high prevalence and is observed in 65%-85% of newborns. Cysts are small (1-3 mm) yellow-white bumps along the palatal suture, especially often located at the junction of the hard and soft palate. Histological examination reveals that these cysts are filled with keratin. No special treatment is required, since the cysts atrophy and disappear soon after their contents are removed.
Gingival cysts of newborns
Gingival cysts develop from the dental lamina (ectodermal ligament), which serves as the basis for the formation of primary and permanent teeth. Its remains can proliferate to form small cysts and subsequently cause the development of various odontogenic tumors and cysts. Depending on the location of formation, cysts that appear on the gums of newborns are called Bohn's nodes (present on the buccal and lingual surfaces of the alveolar ridges) or gingival cysts (formed on the process of the alveolar ridge).
Neonatal gingival cysts have a high prevalence: for example, Taiwanese infants screened within three days of birth had a 79 percent prevalence of the disorder.
Typically cysts look like small whitish lesions of constant size. Those that form on the anterior ridge of the lower jaw can be mistaken for congenital teeth. No separate treatment is required as cysts often rupture due to secondary trauma or friction.
Ankyloglossia
The term “ankyloglossia” (tongue-tied) describes the clinical situations of fusion of the tongue with the floor of the oral cavity or insufficient length of the frenulum of the tongue, limiting its mobility. Ankyloglossia can occur in representatives of various age groups, but is most often observed in newborns. According to research, the frequency of this disorder in newborns ranges from 1.7% to 10.7%, in adults – from 0.1% to 2.1%. Based on this, it can be assumed that some milder forms of ankyloglossia resolve with age.
Ankyloglossia of an infant can cause difficulty in breastfeeding and even cause pain in the nipple area for its mother or wet nurse. The preferred treatment for this disorder in newborns is simple frenectomy, where the frenulum is cut off at its thinnest point with small scissors. The procedure can be performed under superficial anesthesia, which ensures minimal discomfort and reduces the likelihood of bleeding. But bleeding is not necessary. Thus, according to the results of a study involving 215 newborns who underwent frenectomy without anesthesia, 38% of children had no bleeding, and 52% had only a few drops of blood. In 80% of cases, nutrition improved within 24 hours after the start of the procedure.
Congenital epulis of the newborn
This disease is a rare tumor of unknown histogenesis. As a rule, the lesion forms on the alveolar ridge of newborns. The course of the disease is as follows: the tumor does not increase in size from the moment of birth, sometimes it can decrease over time, which indicates a reactive rather than a neoplastic etiology. Most often, this tumor is found in the frontal part of the alveolar ridge of the upper jaw and has the appearance of a round attached formation, usually less than 2 cm in diameter (but sometimes larger ones are found), with a smooth lobulated surface. These types of tumors are more common in girls, which may indicate the influence of hormones, although estrogen and progesterone receptors have not been identified. In 10% of cases, multiple lesions may occur, confirming the need for a thorough oral examination.
As a result of histological studies of congenital epulis, large granular cells with small nuclei were identified. Unlike granular cell tumors, staining with the S100 protein antigen in congenital epulis gives a negative result. Other markers of neurogenic origin also showed negative results, confirming a nonspecific mesenchymal origin of the tumor. Surgical removal is recommended for the treatment of congenital epulis, especially if there is difficulty breathing or feeding problems, or if there is a need for histological confirmation of the diagnosis. For smaller tumors, a wait-and-see approach is acceptable, since cases of spontaneous regression of the tumor are known. There were no cases of relapse, even with incomplete removal of the tumor, or malignant degeneration.
Authors:
Van Heerden, Van Zyl