Why is HPV genotyping needed?
HPV is a heterogeneous virus.
This means that there are many forms of it.
In fact, this is a whole family of viruses, varying in their level of pathogenicity.
When infected with different types of HPV, the risk of cancer increases to varying degrees and different symptoms occur.
About 40 types of HPV are transmitted sexually.
Fourteen of them are viruses of high oncogenic risk.
Thus, genotyping is used to find out what type of virus persists in the patient.
This is important for assessing oncogenic risk.
Patients with different types of HPV are managed completely differently.
If with low-oncogenic viruses a person can have warts removed and sent home, then detection of highly oncogenic types requires dynamic monitoring.
The role of drug therapy is increasing.
It is important for a person to get rid of carriers of the virus as soon as possible in order to prevent precancerous processes and cancer.
PCR diagnostics of papillomaviruses KVANT 21
Detection of the causative agent of papillomavirus infection (Human Papillomavirus), during which the DNA of viruses in a sample of biomaterial is examined using the polymerase chain reaction method in real time.
In this case, the presence and quantity of HPV is determined:
- low oncogenic risk (types 6, 11, 44);
- high oncogenic risk (16, 18, 26, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, 68, 73, 82 types).
Research method
Polymerase chain reaction (PCR).
Result format:
HPV type; HPV number: Lg copies per 100,000 epithelial cells, Lg copies/sample.
What biomaterial can be used for research?
Urogenital smear, urogenital smear (with prostate secretions), rectal smear, oropharyngeal smear.
How to properly prepare for research?
- Women are advised to take a urogenital smear or urine test before menstruation or 2 days after it ends.
- Men should not urinate for 3 hours before submitting a urogenital smear or urine test.
General information about the study
Human papillomaviruses (HPV) are widespread, infect the epithelium of the skin and mucous membranes and have oncogenic potential. HPV is transmitted through close contact with infected epithelium, so the main routes of infection are sexual and household contact. It is possible to transmit HPV from an infected mother to her fetus. A person can be infected with several types of HPV.
Factors that provoke the development of HPV infection include: early onset of sexual activity, a large number of sexual partners, reduced immunity, the use of oral contraceptives, vitamin deficiencies, sexually transmitted infections, smoking and living in large cities.
The incubation period can last from 2 months to 2-10 years. A latent course of the disease is characteristic, in which there are no clinical manifestations, and colposcopic, cytological and histological examination reveals the norm. In 30% of cases, the virus can be cleared within 6-12 months. Diagnosis of latent HPV infection is carried out only by PCR.
During acute infection, benign formations occur, such as papillomas, warts, and condylomas. In children, papilloma viruses can lead to laryngeal papillomatosis. Damage to trophoblast cells by papilloma viruses is fraught with spontaneous abortion.
The combination of papillomavirus DNA with the cell gene leads to dysplasia/neoplasia (most often in the transition zone of the cervix).
What is the research used for?
- To detect papillomavirus infection of high oncogenic risk.
- To confirm/exclude persistence of a certain type of HPV.
- To assess the degree of carcinogenic risk in women with cervical epithelial dysplasia.
What do the results mean?
Reference values: negative.
Reasons for a positive result
- Infection with papilloma virus.
Reasons for a negative result
- Absence of papillomavirus infection.
- Low levels of HPV in the blood.
Detection of HPV DNA in the test material indicates the presence of papillomavirus infection. If HPV DNA is not detected in the biomaterial under study, then the presence of papillomavirus infection is unlikely.
- from 3 Lg to 5 Lg (HPV/10 5 cells) - clinically significant viral load, dysplasia cannot be excluded, there is a risk of developing dysplasia
- > 5 Lg (HPV/105 cells) - clinically highly significant viral load, high probability of dysplasia
Do HPVs cause cancer in everyone?
Of course, viruses do not cause cancer in every person.
Even those that have a high oncogenic risk.
In 90% of cases, a person becomes infected and recovers on his own within 1-2 years.
Often he has no symptoms at all.
In other cases, condylomas or changes in the epithelium appear.
But pathological foci disappear after the virus is eliminated.
However, in 10% of cases, a chronic persistent infection develops.
She is the one who poses the greatest threat.
HPV most often causes cervical cancer in women.
Other types of malignant tumors, including among men, are very rare.
These include neoplasms:
- skin;
- member;
- anus;
- rectum;
- larynx;
- esophagus;
- Bladder.
Observation is required primarily for women.
In them, the virus causes cervical cancer, and this is the most common cause of death from cancer among patients of reproductive age.
Most often during this period only breast cancer occurs.
But they die from it less often.
The insidiousness of the disease is that it is detected late, and the effectiveness of treatment is low already from stage 2.
However, cervical cancer is common only in countries with poor medical standards.
This is a completely controllable disease.
Cancer does not develop out of the blue.
There are many ways to prevent it.
To do this, it is possible to identify HPV in time, carry out genotyping, and establish surveillance if a virus of high oncogenic risk is detected.
Already at this stage, drug treatment often allows you to get rid of the infection and prevent precancerous processes.
If precancerous diseases are identified, they can be cured.
And for all this, a woman has not even years – decades.
But if she never goes to the gynecologist and does not get tested, then cervical cancer appears and develops.
Although this happens slowly, there is no chance of identifying the disease in time.
Because there are no symptoms until the moment when the pathology becomes incurable.
Manifestations of HPV infection
In most situations, when infected with HPV in general and, in particular, HPV 16, women, as well as men, have no symptoms.
Sometimes a sign of infection can be warts and condylomas (in the case of the presence of a virus from the low-oncogenic/non-oncogenic group).
With HPV 16 infection, women may experience precancerous changes on the cervix.
This is revealed during a gynecological examination.
Or preventative, or when the patient consulted a doctor for another reason, for example, with complaints of unusual discharge.
The main diseases caused by HPV 16 are bowenoid papulosis and dysplasia of varying degrees.
With bowenoid papulosis, dense brownish, reddish or flesh-colored papules appear in the labia, pubis, inguinal and perianal areas.
They merge into large warty surfaces up to 2 cm in diameter.
The disease is characterized by a chronic, long-term course.
Malignancy develops in 3% of episodes (degenerates into squamous cell carcinoma), although self-healing is more often diagnosed.
Cervical dysplasia is a precancerous change and requires serious consideration.
Since this pathology may not be diagnosed in a timely manner due to its asymptomatic course, most countries in the world have adopted cervical cancer screening programs.
There are several classification approaches for dysplasia and cervical cancer.
They are based on the results of morphological/cytological studies (studies of cell changes).
According to the International Classification of Diseases, 10th revision, there are:
- mild dysplasia - minor proliferation and changes in epithelial cells, often a similar condition is detected during inflammatory processes in the uterine cervix and is eliminated after appropriate anti-inflammatory therapy
- moderate dysplasia - changes affect the entire lower layer of the epithelium
- severe dysplasia - the entire length of the epithelium is affected, the cell structure is noticeably changed
- cervical cancer (otherwise known as squamous cell carcinoma) – detected during colposcopic examination, confirmed cytologically and histologically
Moderate and severe dysplasia in most episodes is caused by exposure to the virus.
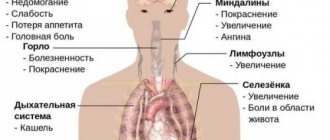
Signs of cervical cancer are detected only in the last stages and include:
- bleeding between menstrual periods, irregular, after sexual intercourse
- unpleasant smell of discharge
- vaginal discomfort
- pain in the pelvic area, back, legs
- weight loss
- fatigue, lack of appetite
- unilateral swelling of the legs
As the disease progresses, the severity of symptoms may increase noticeably.
HPV genotyping: what does this analysis provide?
This is the process of determining the type of virus.
It is based on determining a section of DNA, that is, the genotype of the pathogen.
Research objectives:
- determination of oncogenic types of virus;
- establishing the degree of oncogenic risk for a particular patient (the virus is determined in combination with other research methods);
- determination of therapeutic tactics.
As a result of the test, the doctor receives the following information:
- whether the virus that persists in the human body is highly oncogenic;
- what type of virus it is (even within the group of oncogenic HPVs there are viruses that, to a greater or lesser extent, increase the likelihood of cancer);
- in what concentration it is contained (if there are few viruses, it is likely that the body will soon get rid of them on its own).
HPV HCR genotyping
HCR stands for high carcinogenic risk.
Thus, this study differs in that only highly oncogenic viruses are detected.
For example, you will not receive a conclusion: 6, 11 or another type with low oncogenicity has been detected.
Testing may not be carried out on them.
Situations when typing specifically for BCR viruses is required:
- reduced immunity (including due to HIV);
- “bad” results of oncocytology analysis;
- clinical signs of cervical dysplasia.
That is, the analysis is done when the risk of cancer in a particular patient is assessed as high.
It may not matter whether other viruses are present among those that almost never cause cancer.
HPV genotyping: quantitative analysis
It is not enough for a doctor to know only the type of virus.
Information about its quantity is also needed.
The unit of measurement is the amount of DNA in 100 thousand epithelial cells.
There should be less than 10 to the 5th power.
If this threshold is reached or exceeded, this concentration of virus is considered clinically significant.
Oncogenic viruses in such quantities provoke intraepithelial neoplasia.
And then cancer develops against its background.
Why does a doctor need to know the amount of virus:
- to understand whether he is dangerous;
- give a prognosis for the further development of the infection;
- evaluate the effectiveness of treatment;
- plan further management of the patient (including the observation method, when periodic examinations and tests are carried out).
The analysis is carried out for 10-14 highly oncogenic types.
To determine quantitative indicators, real-time PCR is performed.
It makes it possible to differentiate clinically significant concentrations of the virus from resolving or transient forms of infection.
Who is recommended for HPV genotyping?
In our country, typing is prescribed not for preventive purposes, as in the West, but for medical reasons.
Many women do not get screened.
Therefore, the incidence of cervical cancer and mortality from it in the country remains high.
Typically, women come to the doctor if they have warts on the genitals or have received abnormal results from a cytological examination of a cervical smear.
But most international organizations recommend testing for HPV even without any symptoms or preliminary research.
That is, carry it out to everyone without exception.
According to FIGO recommendations, HPV testing is carried out once every 5 years until the age of 65 years.
WHO recommends testing at least once for all women aged 30-49 years.
The need for HPV testing is also provided for by Russian Ministry of Health Order 572n dated November 1, 2012.
Direct genotyping (determining the exact type of HPV) is not mandatory.
But if possible, it is recommended to carry out typing for at least types 16 and 18 as the most dangerous among all existing ones.
The use of alternative studies is also permitted.
The Digene test is widely used.
It is based on the hybridization of DNA sections with RNA probes.
They are subsequently captured by antibodies with a fluorescent label.
If the results are positive, quantitative indicators are given.
There are also tests based on the detection of HPV RNA.
In particular, the Aptima test is capable of detecting 14 highly oncogenic types with partial genotyping.
How dangerous is the papilloma virus?
Years of WHO research have found a link between this virus and cancer. Therefore, in medicine, strains (varieties of the virus) of a non-oncogenic and oncogenic nature are distinguished. This means that the infection can be either harmless or pose a serious threat to health.
Here is a partial list of malignant tumors caused by HPV:
- cervical cancer;
- cancer of the external genitalia;
- rectal cancer;
- cancer of the larynx and pharynx.
Therefore, you should not postpone a visit to the doctor if rashes, warts and other neoplasms are found on the mucous membranes, genital area and skin.
What to do if dangerous types of HPV are identified?
The risk of detecting dangerous types of HPV in an individual person is low.
In most people, no variant of this virus is detected at all.
If the patient is infected, then with a high probability it is a harmless type of HPV.
Low-oncogenic varieties are much more common.
If you are unlucky and have been diagnosed with highly oncogenic HPV, you need to look at its quantity.
If it is small, no treatment is required.
Most likely, your body has already begun to get rid of the virus, and soon it will no longer be detected.
It's worse if its concentration is high.
In this case, the following is necessary:
- additional tests;
- treatment;
- dynamic observation.
A smear is taken from the patient for oncocytology.
Most often, this study is carried out not after HPV genotyping, but simultaneously with this test.
Based on the results of these two tests, a decision can be made about the need for colposcopy.
It is needed to identify areas of altered epithelium (precancerous processes).
In turn, the results of colposcopy (examination of the cervix) may require a biopsy.
This is a procedure in which a piece of tissue is taken and sent for histological examination.
Based on its results, both a malignant tumor and a precancerous process of stages 1-3 can be diagnosed.
Stage 1 is reversible, while stages 2-3 require cauterization to prevent cancer.
But precancerous processes develop very slowly.
If antiviral treatment is carried out in time, the virus disappears from the body and the cervical epithelium is restored.
Patients must be monitored.
They are tested every six months to assess whether the concentration of the virus is increasing or decreasing.
To eliminate it, antiviral and immunomodulating drugs are used.
Treatment of HPV infection
Which doctor treats HPV 16 in women?
Treatment of HPV infection can be carried out by a gynecologist, oncologist, infectious disease specialist, or venereologist.
It is important to understand that accidental detection of the virus in the absence of clinical changes is not an indication for therapy.
Only if highly oncogenic viruses (HPV 16) are detected in women, the doctor decides what to do next.
Is it necessary to undergo diagnostic examinations and examinations more frequently or to prescribe additional studies?
Only a specialist can determine whether it is necessary to treat HPV 16 in women, taking into account the presence/absence of changes induced by the virus.
In a situation with HPV, it is important to trust your health only to highly professional specialists who are familiar with international protocols for managing the infection.
This is especially important when infected with HPV 16, which provokes malignant pathologies in women (reviews on the Internet or from friends will help you decide on an institution and a doctor).
Today, in women, treatment for HPV 16 is based on the removal of atypically changed epithelium.
It should be understood that if women have an infection, there are currently no drugs that destroy the virus itself.
Any international treatment regimen for HPV 16 does not include any antiviral agents.
At the same time, specific treatment for HPV 16 is carried out, in which it is recommended that women take drugs with immunomodulatory and antiviral activity.
It is believed that such drugs mobilize the immune system to fight the virus.
Such products have not been sufficiently tested for effectiveness in clinical trials.
Accordingly, there is no reliable data on the cure rate.
Despite this, many patients note a significant improvement in their well-being after using them.
Immunocorrective therapy for HPV 16 in women includes:
- with human recombinant interferon or its inducers, suppositories (Viferon, Genferon), Isoprinosine, Cycloferon, etc.
- with an immunostimulating effect - Lykopid, Polyoxidonium, etc.
- B vitamins, omega acids and dietary supplements
Often, before prescribing a drug treatment regimen, an analysis of the immune status (immunogram) is recommended.
With determination of indicators of the activity of monocytes, neutrophils, lymphocyte function, levels of immunoglobulins, CD16+, CD8+, CD4+ and others.
Unfortunately, for many drugs, data on the safety of use, complications and relapses after use have not been obtained.
Therefore, it is recommended to refrain from using them for people with:
- autoimmune diseases
- malignant formations (for cervical cancer can be prescribed only after completion of surgical treatment)
- allergic reactions
- bronchial asthma, etc.
As for the generally accepted approach to the management of HPV infection in the international medical community, the following points are positioned here:
- There is no medicine to remove the virus from the body, but the likelihood of self-healing is very high, especially at a young age
- If there are no changes in cellular structures and a virus from a high oncogenic risk group is identified, more frequent and careful monitoring of the patient is carried out
- If changes caused by the activity of the virus are detected, therapy is carried out aimed at eliminating pathological changes
For bowenoid papulosis caused by HPV type 16, tumors are removed using the following methods:
- Mohs excision
- laser therapy
- cryodestruction
- electrocoagulation
- local application of ointments with cytostatics (5-fluorourocil, prospidin, fluorofur)
- intralesional administration of interferon
- oral administration of Neotigazon capsules
Precancerous conditions and the first stages of cervical cancer are highly treatable.
The changed cells are removed using cryotherapy.
For dysplasia, organ-preserving operations are performed: conization of the cervix with a scalpel, electrosurgically, laser with preliminary canal curettage.
For localized forms of the tumor, surgical treatment is carried out, for a widespread process - radiation and chemotherapy.
Taking into account the fact that eliminating the result of virus activity does not remove the infectious agent itself.
The risk of recurrence of pathological changes remains, which, in turn, requires further monitoring of the patient.
In addition, the possibility of HPV reinfection cannot be excluded.
After implementing any treatment option, follow-up tests are recommended.
Since there is a possibility of spontaneous elimination of the virus within 2 years from the moment of infection.
A separate problem is presented by persons with HPV against the background of HIV infection.
It has been proven that the risk of developing cancer in such women is higher, as is the risk of HPV infection itself.
Although primary HPV infection was detected more often, which is associated with the greater prevalence of this virus.
Moreover, the worse the patient’s immune status, the higher the likelihood of her developing HPV-induced cancer.
Therefore, people with HIV status are recommended to undergo HPV testing more frequently.
Treatment is carried out using the same methods as for those uninfected with HIV, with additional specific therapy aimed at suppressing the activity of the immunodeficiency virus.
Is it possible to do HPV without genotyping?
Of course, such an analysis can be done.
It is also quite informative.
HPV genotyping costs are higher, and such costs are not always necessary.
In any case, as a result of the test, the type will be determined or not, the doctor will find out whether the HCV papillomavirus is present in the body.
If it is present, and if it is present in high concentrations, in any case the patient must:
- treatment;
- dynamic observation.
And this is necessary, regardless of the specific type of virus detected.