Oncogenic HPV: how is it transmitted?
From 60 to 70% of cases or carriers are infected through sexual contact.
All types of coitus play a role, since the virus can be on the mucous membrane of the mouth, vagina or rectum.
At the same time, anal contact reduces local resistance in a man, increasing the risk of infection.
The entry points for an infectious agent are often sites of injury or maceration of the mucous membrane or skin.
Peak infection occurs between 20 and 30 years of age.
Men and women are infected equally often.
Infection through household contact occurs much less frequently.
Here, wound surfaces of the skin or mucous membranes (extensive wounds, scratches, burns) also come first.
A vertical route of infection is also possible.
The fetus can receive the virus from the mother in utero.
Or when passing through the birth canal in cases where there is a clinically developed viral process in the mother.
How is HPV infection treated during pregnancy?
When infected with HPV, pregnancy and childbirth have some specifics.
Thus, in some women with HPV infection, during pregnancy, the manifestations of the disease may increase, such as changes in cervical cells and genital warts.
However, doctors are usually in no hurry to prescribe treatment.
Since the latter can provoke premature birth, in addition, after childbirth, the manifestations of infection may noticeably decrease on their own.
Therefore, it is recommended, if possible, to adhere to expectant management and dynamic monitoring of the pregnant woman.
However, there are situations when genital warts grow noticeably and their number increases.
They merge into giant formations.
Women may experience pain when walking, difficulty defecating and urinating.
During childbirth - traumatization of formations, bleeding, problems with the passage of the fetus through the birth canal, ruptures of the vaginal walls.
In such cases, it is necessary to remove condylomas before delivery.
If the removal of the formations could not be carried out on time, the doctor may decide to deliver the patient by cesarean section.
In routine practice, this measure is not used to prevent fetal infection.
Since there is no reliable data confirming that cesarean section prevents the development of respiratory papillomatosis in children of sick mothers.
If abnormal cell changes were detected during pregnancy, a Pap smear test should be repeated a few weeks after birth.
Often, after childbirth, both genital warts and cellular changes disappear on their own.
Accordingly, treatment of such conditions is not required.
In other situations, certain therapeutic procedures are carried out.
In pregnant women, removal of condylomas can be carried out through cryotherapy, using a carbon dioxide laser, electrocoagulation, or surgitron.
For large, easily traumatic formations, it is recommended to remove them surgically after the first trimester until the 36th week of pregnancy.
The use of drugs such as podophyllin, 5-fluorouracil, as well as the use of intralesional interferon is not allowed during pregnancy.
How does HPV infection occur?
Papillomaviruses can only be transmitted from person to person.
Since some types can persist for a certain time in exfoliating skin cells, they may pose a risk of household contact infection.
This option is typical for the non-oncogenic group; for example, infection with the formation of plantar warts is likely in the presence of microdamages to the skin of the feet.
Low- and high-oncogenic viruses are transmitted sexually, including various types of sexual contact.
Infection of newborn children by sick mothers occurs occasionally.
Interestingly, women with diabetes, when their glucose levels are well controlled, do not have an increased risk of HPV infection.
The incubation period is quite long and can vary from three months to several years.
What else is prescribed with this study?
Antigen for squamous cell carcinoma (SCC) (carcinoma of the cervix, nasopharynx, esophagus, ear and other localizations)
8.14. Ven. blood 1 day
2,300 ₽ Add to cart
HPV 16/18/31/33/35/39/45/51/52/56/58/59 type, DNA (HPV, PCR, genotyping) scraping, count.
19.57. Scraping 1 day
1,710 ₽ Add to cart
HPV 16/18/31/33/35/39/45/51/52/56/58/59/68 type, DNA (Digene-test, PCR, without genotype determination) scraping, count.
19.75. Scraping 10 days
6,470 ₽ Add to cart
HPV type 6/11/42/43/44, DNA (Digene-test, PCR, without genotype determination) scraping, count.
19.76. Scraping 10 days
6,360 ₽ Add to cart
Gynecological smear for flora
16.1. Scraping 2 days
630 ₽ Add to cart
Examination of scrapings from the cervix (Papanicolaou test, Pap test)
14.11. Scraping 3 days
1,450 ₽ Add to cart
Femoflor Screen (Study of the microflora of the urogenital tract in women, 12 indicators), scraping
50.2.2087. Scraping 3 days
2,670 ₽ Add to cart
Femoflor-16 (Study of microflora of the urogenital tract in women, 16 indicators), scraping
27.39. Scraping 3 days
3,110 ₽ Add to cart
How does the infection manifest?
Symptoms of infection are determined by the type of virus and the type of illness it causes.
HPV can be located either outside the cell chromosomes, the so-called. benign form of the disease, and integrated into DNA, the malignant form.
The following development options are typical for human papillomavirus infection:
- latent course - without cell changes, without symptoms;
- the formation of warts, condylomas, papillomas, when the virus affects cells, provoking their growth;
- neoplastic changes (dysplasia) – changes in cellular structure under the influence of a virus;
- carcinoma formation - the appearance of numerous atypical cells characteristic of a cancerous tumor.
An important feature of HPV infection is its ability to self-heal.
In 90% of all episodes of infection, the virus is destroyed by the body within two years.
Clinical manifestations of infection are quite characteristic.
Thus, vulgar warts look like grayish-brown warty nodules, which are usually located on the fingers and the back of the hands.
Flat warts affect the face and hands and usually appear during adolescence.
Plantar warts appear in areas where the skin rubs against shoes and are characteristic thickenings that are painful when pressed.
Genital warts are shaped like a rooster's comb or a cauliflower stalk, have a thin stalk and a wider head.
In women, such formations are usually located at the entrance to the vagina, in the area of the labia and anus. Multiple flat papules, as a manifestation of infection caused by HPV of low oncogenic risk, are called epidermodysplasia verruciformis.
With laryngeal papillomatosis, typical growths are detected in the larynx.
Dome-shaped and flat, smooth, velvety papules on the genitals are a characteristic manifestation of bowenoid papulosis.
The cause of which is predominantly HPV-16 (a representative of the high oncogenic risk group).
Malignancy of such formations is observed in approximately 3% of episodes.
Dysplasia (neoplasia) of the cervix is a process of atypical changes in epithelial cells in the zone of transition of squamous epithelium to columnar epithelium.
This condition is considered precancerous.
Depending on the severity of cell changes, different degrees of dysplasia and cancer itself (squamous cell carcinoma) are distinguished.
Promote the development of dysplasia:
- multiple pregnancies and births before the age of 20;
- early onset of sexual activity;
- promiscuity;
- chronic inflammation of the uterine cervix;
- damage by genital warts;
- smoking, etc.
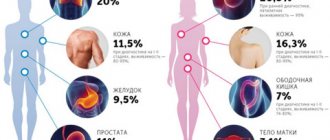
Why is papillomavirus dangerous?
The potential threat in viruses of this type is primarily the risk of growth of tumors of the urinary tract and genitals.
Slightly less commonly, viruses are responsible for tumor growth in the oropharynx area.
The long-term existence of the virus in epithelial cells sooner or later changes their structure and ability to divide uncontrolledly.
Any episode of infection should be diagnosed, monitored and, if possible, treated.
Errors in immune defense can occur at any stage of life.
In addition to external provoking factors, they can be caused by natural hormonal fluctuations.
Therefore, today there is an urgent question about creating artificial protection against papillomaviruses by vaccinating high-risk groups or children.
What is HPV infection?
A specific feature of HPV is its tendency to infect epithelial cells of the skin and mucous membranes.
Several dozen known types of human papillomaviruses are grouped into three groups according to their ability to provoke cancer.
In this case, they distinguish:
- non-oncogenic, examples of which are types 1,2,28, 41, etc., responsible for the appearance of skin warts (plantar, vulgar, etc.);
- with a low risk of developing oncopathology, such as types 6,11, 15, 25, 43, etc., infection with which can manifest itself in the form of anogenital warts (otherwise genital warts) and be accompanied by the development of malignant transformations only in extremely rare cases;
- with high risk, including types 16, 18, 33, 52, etc., infection with which is associated with precancerous/cancerous changes in the cervix, as well as a disease such as bowenoid papulosis.