An indicator of good health has always been the condition of the skin and mucous membranes. The condition of our skin is influenced by both aggressive environmental factors and internal processes in the body.
Our skin immediately signals a problem with irritation, rashes, comedones and other cosmetic defects. Proper and regular skin care will help prevent their occurrence.
One of the common cosmetic problems of clogged pores is comedones or acne. Acne is caused by the skin secreting sebum, which clogs the pores or hair follicle, which can eventually cause a cyst.
Why retinol?
Retinoids are a group of drugs based on vitamin A, represented by retinol and its derivatives.
The Global Alliance of Dermatologists and Cosmetologists, based on many years of research, clinical observations and treatment of patients with problem skin, has come to the conclusion that
Retinoids are the N1 substance in acne therapy.
Russian experts classify retinoids as first-line drugs for the treatment of problem skin with acne.
The term “1st line” means that they are recognized as the most effective and it is worth starting therapy with their prescription.
One of the main goals of acne treatment is not just to stop the process and get rid of acne, it is important to prevent the appearance of scarring. After all, getting rid of scars is almost impossible!
For a detailed understanding of the reasons for which the Global Alliance of Dermatologists and Cosmetologists made this conclusion, let’s begin the analysis by listing the points where retinol works for acne.
Comedones - what are they?
Comedones are signs of acne or acne - derived from the Latin language from acne comedonica. They are deep subcutaneous rashes - black and white dots that appear on the skin due to clogged pores.
Comedones on the face are a common problem for oily and combination skin types. Against the backdrop of excessive work of the sebaceous glands, blockage of pores and sebaceous ducts occurs - excess sebum mixes with dead skin cells, remnants of makeup and external impurities, forming a sebaceous plug.
Important(!): without timely care, an inflammatory element may occur at the site of the comedone: the sebaceous plug creates an ideal environment for the proliferation of acne bacteria, which provoke inflammation.
How does retinol work for acne?
Points of application of retinol and its derivatives for acne:
FOLLICULAR HYPERKERATOSIS
Retinoids, like AHA acids, are able to break the bonds between keratinocytes, stimulating their exfoliation, inhibit the excessive proliferation of the ductal epithelium, thereby cleanse the pores on the face and eliminate their blockage.
CLOSED COMEDONS
Through the hair follicle, retinoids are able to penetrate right up to the ducts of the sebaceous glands, where they also stimulate exfoliation and elimination of accumulated sebum, which stretches the sebaceous glands, turning them into retention cysts.
Result : a large number of dead cells do not accumulate in the ducts and their removal to the outside improves, which removes the blockage of the duct - sebum accumulated in the gland comes to the surface of the skin.
INFLAMMATION
Retinoids are antioxidants that further reduce the production of proinflammatory cytokines and other inflammatory factors (eg, IL-1β, TNF-α, and nitric oxide NO).
Important : inflammation is recognized as a key factor provoking the severity of the acne process, and, therefore, the main starting point for acne therapy.
PATIENT
Retinoids indirectly inhibit the proliferation of P. acne bacteria, preventing the formation of antibiotic resistance in bacteria that form skin microbiologists.
IMMUNE FUNCTION OF THE SKIN
Retinoids block important inflammatory pathways such as AP-1, as well as leukocyte migration and toll-like receptors. In addition, retinoic acid (one of the forms of retinol, formed inside the skin during the transformation of retinol) affects Langerhans cells - skin macrophages, increasing their readiness for phagocytosis and migration to the site of inflammation.
PREVENTION OF POST-ACNE
According to clinical observations, early use of retinoids to correct acne minimizes the risk of scarring.
Also, topical retinoids reduce the risk and clinical manifestation of post-acne hyperpigmentation. The higher the dose of topical retinoids, the greater the preventive effect.
The main causes of acne and comedones:
- improper skin care: neglect of hygiene rules, insufficient cleansing of the skin, use of cosmetics that are not suitable for your skin type;
- mechanical damage to the skin: chemical peeling, exfoliation, self-squeezing pimples;
- excessive production of sebum;
- consuming large amounts of sugar and fats;
- preference in the diet for dairy products;
- allergic reactions.
There are two types of acne: closed and open:
- Closed comedones are white, small, located under the skin in the form of nodules, and tend to become inflamed, forming pimples.
- Open comedones are black rashes located on the surface at the base of the hair follicle and rarely become inflamed.
What retinoids to use for acne
Having understood how retinol works for acne, the question arises: what form of retinol is best to use to treat acne?
To answer this question, you need to understand:
- When treating acne, the goal is not to activate fibroblasts and basal keratinocytes to stimulate cellular renewal and synthesis of the dermal matrix.
- With acne, skin barriers are often compromised. Therefore, the requirement for the selected Retinoid is to minimize aggression and eliminate irritating effects that could provoke the client’s desire to refuse therapy.
Irritation from retinol
Conclusion
At the beginning of therapy, give preference to atraumatic forms of Retinoids without affecting RAR receptors (fibroblasts and basal keratinocytes). Pure retinol and retinol acetate are excluded from acne therapy, especially in the initial stages of treatment.
Comedones (blackheads) - symptoms and treatment
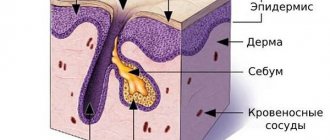
The formation of comedones is based on disruption of the normal functioning of the sebaceous glands. They are located in the deep layers of the skin, at the root of the hair.
The sebaceous glands produce their own secretion - sebum, or sebum. Moving up the pilosebaceous duct, it creates a protective barrier on the skin, gives it elasticity, maintains a normal pH level, and helps retain moisture.
The cells that produce sebum are constantly renewed: they shift towards the mouth of the sebaceous gland, gradually accumulate secretion and are destroyed. The keratinocytes that line the exit duct of the follicle are also constantly renewed and exfoliated.
When the function of the sebaceous glands is disrupted, the following happens:
- The sebaceous glands begin to produce too much sebum. It turns into a thick sticky mass that completely fills the duct.
- The formation of keratinocytes intensifies, and there are more cells. They get stuck in thick sebum and clog the outlet duct of the sebaceous gland.
When the lumen of the canal is completely filled, the contents of the pilosebaceous duct begin to press on the walls of the canal. The mouth of the duct expands, eventually forming a comedon. In such an environment, opportunistic flora is activated over time. She begins to absorb excess sebum, which is a nutrient medium for her. As a result, the pilosebaceous follicle becomes inflamed and acne develops [3].
Heredity, hormonal disorders and nutrition
A genetic predisposition to comedones may be associated with one of four characteristics:
- large sebaceous gland;
- hypersensitivity of sebaceous gland receptors to sex hormones - androgens;
- hyperandrogenism - high levels of androgens;
- increased activity of the enzyme 5-alphareductase with normal levels of sex hormones.
The last feature is associated with the transition of androgen to dihydrotestosterone - DHT. This transition occurs under the influence of the enzyme 5-alphareductase.
DHT controls the activity of the sebaceous glands and the process of keratinization. This hormone binds to androgen receptors in a “lock and key” manner, where the “key” is the hormone and the “lock” is the androgen receptor. But “opening the lock” can only be done with the help of another hormone—insulin or insulin-like growth factor—IGF-1 [3].
Insulin and glucose themselves are necessary for the body. Their level increases after eating any food. But with excessive amounts of sweets, refined and other foods, the concentration of insulin and glucose becomes greater. Moreover, the level of glucose in the blood increases first, and then insulin. And then everything develops according to the same scenario, leading to the active production of sebum and the formation of comedones.
Insulin levels also increase when eating whole milk products. Insulin binds to androgen receptors and increases DHT levels. This hormone, in turn, binds to the receptors of the sebaceous glands and stimulates the production of sebum.
Therefore, people who are genetically prone to increased sebum secretion should be especially careful and control the consumption of sweets, dairy and refined products.
Improper skin care
Skin prone to the development of comedonal acne needs proper care.
Soap, harsh scrubs and alcohol products with surfactants only injure the skin, leading to the appearance of new comedones. These products disrupt the skin's pH, its protective barrier, causing it to become overdried. The body will try to restore the skin barrier by increasing sebum production and the formation of keratinocytes. But this will only worsen the skin condition.
People prone to the formation of comedones are also not recommended to use oils, thick creams or massage the skin. Thick creams and oils can further clog the pilosebaceous duct, and increased kneading, rubbing and pressure on the skin can lead to an exacerbation of the disease.
Stress
Stressful situations are a trigger factor for comedonal acne [4][5]. This is due to the production of neurotransmitters, in particular substance P. This substance transmits a signal, triggers the process of inflammation, dilates blood vessels and increases capillary permeability.
The sebaceous glands are hypersensitive to substance P. Therefore, neurotransmitters bind to the cells of the sebaceous glands and stimulate their activity. As a result, sebum formation increases [7].
Localization of comedones
Most often, comedones on the face are found in people with oily and combination skin with a tendency to acne. The more sebum is secreted, the higher the risk of clogging pores and forming a sebaceous plug.
Black comedones can also occur in people with dry and normal skin types. Subcutaneous whiteheads are the most common signs of acne due to increased oily skin.
Such imperfections are predominantly localized in the T-zone of the face - on the forehead, but on the nose and chin - areas of the greatest accumulation of sebaceous glands. Often comedones appear on the back, shoulders or chest - the sebaceous glands in these areas are also active, and the pores are enlarged.
Types of comedones
In dermatology, there are two types of comedones, depending on the depth of their formation:
- Open comedones
are the usual blackheads - superficial blockage of pores with sebum mixed with external impurities and makeup residues. Open comedones acquire their characteristic dark color due to the oxidative reaction of the sebaceous plug and oxygen. - Closed comedones
are white subcutaneous nodules that look like pimples without purulent contents. They arise against the background of an imbalance of sebum regulation: when excess sebum, mixed with toxins and the keratinized layer of cells, blocks the deep sebaceous ducts and the mouths of the hair follicles, accumulates in the pores and creates a kind of compaction or cyst - a subcutaneous sebaceous plug.
What causes comedones: the main reasons
Alexander Prokofiev, a dermatovenerologist, expert of the La Roche-Posay brand, talks about the possible causes of comedones:
- Incorrectly selected care, for example, some compositions of cosmetics can clog pores, excessive frequent esfoliation with scrubs and peels can disrupt the hydrolipid mantle of the epidermis, to which the skin will react with increased sebum secretion.
- Insufficient or excessive cleansing of the skin: in the first case, residues of pollution and decorative cosmetics clog pores and cause inflammation. In the second, the skin barrier is damaged, dries out, peels off - the keratinized layer of cells mixes with sebum and creates a sebaceous plug in the pores.
- Some diseases, for example gastrointestinal disorders, as well as hormonal changes in the body can trigger rashes.
- Touching your face with your hands stimulates the sebaceous glands, which increases the risk of comedones and other imperfections.
- Synthetic clothing does not allow the skin to breathe; the skin reacts with increased sebum and sweating, which also causes clogged pores in the back, shoulders, neck, and chest.
- Poor nutrition and non-compliance with the drinking regime negatively affect the condition of the epidermis: insufficient drinking regime affects the face with dryness, flaking, unbalanced nutrition and bad habits disrupt the functioning of the sebaceous glands.
- Some cosmetics may contain ingredients that clog pores. If your skin is prone to imperfections, choose cosmetics labeled “non-comedogenic” and “for oily problem skin.”
In what cases should you consult a doctor for treatment?
If there are no visible results from home care in combination with cosmetic procedures, you should consult a dermatologist. After an in-person examination and based on test results, the doctor will select individual drug treatment using, for example, hormonal drugs or antibiotics.