We have cured more than 2,000 patients who were considered hopeless. Most of these patients were treated unsuccessfully for a long time (some for 35 years) in leading clinics both in our country and in foreign clinics in Israel, Germany and Switzerland. Moreover, we treated all of them on an outpatient basis - not a day of bed rest was required.
If you have an urgent question or acute pain, you can contact the doctor by phone:
8 Andreev Dmitry Yurievich
Examples of patients with trophic leg ulcers treated in our clinic (photos before and after treatment):
See all patient reviews
Over the past 20 years, we have managed to come a long way - from the creation and use of tissue extracts containing growth factors, to cellular technologies and the development of a series of original wound dressings with recombinant growth factors. In the photographs you can see the patents we received for these developments.
Causes of trophic ulcers on the leg
A trophic ulcer always accompanies another serious disease. Diseases that contribute to the appearance of trophic ulcers:
- advanced stage of varicose veins
- thrombophlebitis
- atherosclerosis
- diabetes
- hypertonic disease
- burns, frostbite
- arsenic or chromium poisoning
- radiation exposure
- diseases of the spinal cord and peripheral nerves
- complicated tuberculosis and syphilis
- blood diseases
- long-term immobility as a result of injury (bedsores)
- complicated skin diseases, including allergic ones
Trophic ulcer - symptoms
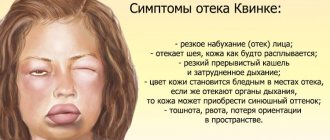
Trophic ulcers do not form spontaneously. Initially, swelling appears, accompanied by severe itching. The skin becomes thinner. Pigmentation or cyanosis appears.
Multiple trophic ulcers on the leg
The appearance of a trophic ulcer is often accompanied by chills and night cramps of the calf muscles. Due to stagnation in the lymphatic vessels, droplets of liquid begin to appear on the glassy surface of the skin. Next, the foci of exfoliated epidermis merge, and an ulcer with ragged, compacted edges is formed, causing severe pain at the slightest touch. As a rule, the ulcer surface is quickly colonized by bacteria, and the bleeding ulcer begins to fester.
Features of different types of ulcers
Venous ulcers
This type of trophic ulcer usually appears on the inner surface of the leg. Venous ulcers occur as a result of impaired blood flow in the lower extremities due to stasis dermatitis.
In this case, the lower part of the leg from the foot to the knee swells greatly, and cramps may occur at night. Then the lower leg begins to itch very much, and a mesh with enlarged veins appears on it. With further damage, red-violet spots and hyperpigmentation appear. The skin becomes denser, acquires shine and smoothness. Small ulcers quickly increase in size, the purulent process first affects the skin, then the Achilles tendon, calf muscle, and periosteum of the tibia. The ulcer first releases serous fluid, and when infected, pus with a nauseating odor.
If this disease is not treated or treated incorrectly, the lymph nodes may be affected and “elephantiasis” may develop (a type of swelling of the legs when the size and shape of the affected limb changes). And in some cases, even death is possible due to blood poisoning - sepsis.
Arterial ulcers
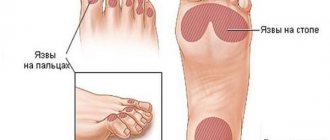
Arterial ulcers are initially, as a rule, small wounds with jagged edges filled with pus. They develop against the background of damage to the main arteries of the legs and form on the sole and outside of the foot, big toe and heel. This type of trophic ulcers occurs due to obliterating atherosclerosis. An arterial ulcer can occur due to hypothermia of the feet, wearing tight shoes, or damage to the skin. This disease most often affects smokers and older people.
Diabetic ulcer (Diabetic foot)
Diabetes mellitus causes various complications, one of which is a trophic ulcer. Although blood circulation in the legs may not be significantly impaired, due to damage to the nerve endings, patients complain of loss of sensation and coldness of the limb. Diabetic ulcers most often occur on the big toe. With further development of the disease, first the remaining toes are affected, and then the entire foot.
A diabetic ulcer is dangerous because it quickly becomes infected. This can lead to gangrene and leg amputation.
Hypertensive ulcers (Martorella)
Quite a rare type of ulcer. Hypertensive ulcers can appear as a result of constant high blood pressure (arterial hypertension), and this can provoke spasm of small vessels. Hypertensive ulcers most often affect women over 40 years of age. The peculiarity of these types of ulcers is the symmetry of the affected areas in the middle part of the legs.
Hypertensive ulcers are very painful and are most susceptible to bacterial infection.
Neurotrophic ulcers
Occurs as a result of injury to the head or spine. A neurotrophic ulcer is located on the side of the heel or sole in the form of a small but deep hole, involving bone, tendon and muscle. The skin around the wound loses sensitivity.
Trophic ulcer with varicose veins
More than 70% of cases of trophic ulcers are caused by severe cases of varicose veins. Even minor damage to the integrity of the skin with varicose veins can lead to the formation of ulcers on the ankles and legs.
Large trophic ulcer on the leg
Trophic ulcers located on the lower leg indicate serious changes in larger venous vessels and the spread of an area with impaired innervation and poor blood supply. A trophic ulcer of the leg usually causes severe pain.
Education mechanism
As a result of exposure to the causative factor, the pressure in the venous capillaries of the upper extremities increases, and they begin to change their shape and direction. They become crimped and thinned. Their permeability increases, fibrin and blood clots are deposited between the venous vessels. This leads to hypoxia (low oxygen saturation of the blood vessels). The level of blood circulation decreases sharply, causing ischemia (circulatory failure). A prolonged absence of normal blood circulation provokes the development of necrotic processes. Plaques of various shapes form on the hands, which over time either dry out and turn into a dry form of necrosis or begin to quickly increase, reaching large sizes.
Trophic ulcer, stages or course options
The size of the trophic ulcer directly depends on the lack of blood supply and the duration of the pathological process. Usually the ulcerative surface occupies no more than 35 cm2. If left untreated, it can cover the entire lower leg and reach 100 cm2. Treatment methods for trophic ulcers must be correct, competent and qualified: no poultices or tinctures!
Stages of appearance of a trophic ulcer
The initial stage (small bleeding ulcer) is complicated by the addition of a bacterial and fungal infection. Purulent contents with an unpleasant odor begin to separate from the ulcer. The longer the process, the deeper the layers are subject to inflammation and rotting. The ulcerative lesion spreads to the calf muscles, involving the ankle joint in the inflammatory process. In advanced cases, the development of pyoderma, phlegmon and sepsis is possible.
It is worth distinguishing between venous and arterial trophic ulcers. The former occur in patients of any age, while arterial ulcers are a disease that occurs exclusively in old age, caused by atherosclerosis of the artery walls.
Trophic ulcer, diagnosis
When diagnosing a trophic ulcer and identifying the causes of its occurrence, the following laboratory tests are used:
- determination of blood sugar levels
- Wasserman reaction
- cytological analysis
- bacteriological examination
The doctor also prescribes a number of necessary studies:
- Ultrasound examination of the vessels of the lower extremities
- angiography (x-ray examination of blood vessels with a contrast agent)
- rheovasography
- infrared thermography
- spiral computed tomography
Diagnosis of a trophic ulcer is a key stage in proper treatment
To select an effective treatment, consultation with a phlebologist surgeon specializing in vascular diseases of the lower extremities is necessary.
Classification of the most common trophic ulcers of the lower extremities
• Ulcers due to chronic venous insufficiency of the lower extremities due to varicose and post-thrombotic diseases. • Ulcers caused by obliterating atherosclerosis of the arteries of the lower extremities. • Diabetic trophic ulcers. • Ulcers due to obliterating endarteritis. • Hypertensive trophic ulcers (Martorell syndrome).
• Ulcers due to congenital malformations of the vessels of the lower extremities: - with Klippel-Trenaunay syndrome - with Parkes-Weber-Rubashov syndrome • Ulcers due to lymphedema - due to primary lymphedema - due to secondary lymphedema • Ulcers due to pyoderma gangrenosum
This is the most famous and common type of ulcer. Occurs in severe venous insufficiency at advanced stages of varicose and post-thrombotic disease.
Clinical symptoms of this type of ulcer are swelling, sclerosis of the skin and subcutaneous tissue, then hyperpigmentation and white atrophy of the skin preceding ulceration.
The pathogenesis of venous (varicose and postthrombotic) ulcers is similar. They are caused by increased venous pressure due to damage to the saphenous veins in the case of varicose veins or deep veins in post-thrombotic disease.
Postthrombotic disease (PTD) occurs due to the destruction of deep vein valves after phlebothrombosis and develops in more than half of patients who have undergone proximal thrombosis and in about a quarter of patients after deep vein thrombosis of the leg. Unlike varicose veins, patients with PTB may not have visible saphenous varices.
Since about 90% of all blood flows through the deep veins of the legs, and only 10% through the saphenous veins, the severity of these ulcers differs. Varicose ulcers (ulcers with varicose veins) are much smaller than with post-thrombotic ones, and are almost always localized in the lower third of the leg and in the ankle regions. With postthrombotic disease, ulcers can reach gigantic sizes, becoming circular. They can extend to the deep fascia, and exudation from them can exceed 1.5 liters per day. Thus, in the photograph below of patient A., 66 years old, you can see a galosh filled with wound secretion that accumulated during half an hour of walking.
Why is a trophic ulcer dangerous? - Wikipedia warns!
The main point in the treatment of trophic ulcers is to identify the underlying disease that caused the ulcerative skin defect. This approach will ensure effective treatment of ulcers and prevention of relapses. The danger of trophic ulcers lies in the fact that, in the absence of proper treatment, damaged cells are capable of malignant degeneration and the appearance of squamous cell carcinoma, and in rare cases, skin sarcoma. Therefore, even if the trophic ulcer has gone away, treatment after surgery should continue.
Causes
The main reason for the development of such defects is not only vascular diseases. Often, trophic ulcers occur against the background of neoplasms localized in the axillary, subclavian and mediastinal lymph nodes. In addition, injuries of various types (stabbed, cut, chopped, bitten), infectious and inflammatory diseases (chickenpox, helminthic infestations), pathologies of the immune system, systemic connective tissue diseases (lupus erythematosus, vasculitis), sepsis cause aggravation of the skin syndrome and the development ulcerative defects on the hands.
Trophic ulcer - treatment in Moscow
Do you have a trophic ulcer? Treatment in Moscow or in any other city is quite lengthy and involves a whole range of measures to ensure that the trophic ulcer disappears. Conservative treatment, the same as drug treatment, is aimed at reducing the symptoms of the underlying disease that caused a violation of tissue trophism, treating the ulcerative lesion itself and fighting secondary infection.
Excellent results in laser treatment of trophic ulcers
Depending on the stage, the trophic ulcer is removed in different ways. Treatment (Moscow offers many methods) depends on the stage of development of the trophic ulcer and is carried out in the following areas:
- local treatment;
- elastic compression;
- drug treatment;
- hemosorption - removal of toxic tissue breakdown products from the blood;
- physiotherapy;
- autoirradiation of blood with laser or ultraviolet rays;
- surgical intervention if indicated;
- visiting sanatoriums.
What to do if you have deep trophic ulcers of the lower extremities? What to do if a large trophic ulcer, treatment (photo, results you have already assessed) which you have not carried out, increases?
View all patents
Venous ulcers | Ulcers in atherosclerosis | Diabetic trophic ulcers | Ulcers due to obliterating endarteritis | Ulcers in hypertension | Ulcers due to congenital vascular malformations | Ulcers due to lymphedema | Pyoderma gangrenosum | Hydrostatic ulcers | Ulcers due to malignant skin tumors
There are different definitions of the concept of “trophic ulcer,” but its main criteria are, firstly, damage to the skin over the entire thickness, that is, the absence of sources for epithelization at the bottom of the ulcer and, secondly, the low healing rate. Trophic ulcers of the lower extremities are a common pathology. They affect about 1% of the total adult population, and among elderly people (over 65 years old) this figure increases to 5%. Currently, in developed countries, the incidence of ulcers is increasing, which is associated with the aging of the population and the spread of risk factors for atherosclerosis obliterans, such as smoking, diabetes and obesity. Few people know that the diagnosis “Trophic ulcer” does not exist. A trophic ulcer is not a diagnosis, but a CONSEQUENCE of advanced diseases, of which there are more than a hundred. And they are treated differently. Trophic leg ulcers account for 3 pathologies in 95% of cases:
1. Venous insufficiency of the lower extremities due to varicose and post-thrombotic diseases: approximately 55% of all ulcers; 2. Obliterating atherosclerosis of the arteries of the lower extremities: approximately 15% of all ulcers; 3. Diabetes mellitus: approximately 20% of all ulcers; Combinations of the above reasons: approximately 10% of all ulcers.
The remaining diseases, of which there are more than a hundred, lead to ulcers, which occur in approximately 5% of cases. But it is precisely these 5% of cases that cause the greatest difficulties in diagnosis and treatment.
Trophic ulcer - treatment at home
The attending physician decides about the possibility of treating the disease at home. With the prescribed set of medications, the patient can do dressings at home, while regularly visiting the doctor. It is desirable, of course, that this doctor be a good specialist in the treatment of trophic ulcers. There are few such doctors in Moscow.
Leading specialist of our center for the treatment of trophic ulcers Malakhov A.M.
Our leading surgeon-phlebologist Alexey Mikhailovich Malakhov deals with this problem.
Treatment of ulcers
Treatment of trophic ulcers should be carried out using complex methods: it is necessary not only to eliminate the local manifestation of the process, but also to fight the cause of the disease. For this purpose, surgical and medicinal methods are used. When microbial infection develops, detoxification therapy is carried out, which removes decay products of microbial cells and improves the patient’s condition. Great importance is attached to normalizing the work and rest regime and wearing special compression garments. Reviews about the treatment of trophic ulcers indicate the effectiveness of physiotherapeutic procedures.
In the multifunctional clinic "MedicCity" you will be able to offer full-fledged treatment using modern, unique equipment. So start your treatment now. After all, not only your health, the degree of your recovery, but also your life depends on how quickly you see a doctor!
Trophic ulcer - treatment without surgery
If the cause of the ulcer is not venous pathology, then conservative measures are sufficient. A portable laser device is a great help in home treatment of the initial stages of ulcerative skin lesions up to 50 cm2 in size. A laser injected into a vein helps reduce blood viscosity, significantly reduces the risk of blood clots, and increases blood flow in problem areas. In addition, the laser beam effectively reduces pain and trophic ulcers. Laser treatment (reviews below) in combination with conservative treatment allows you to avoid surgical intervention.
Laser therapy is carried out in courses of 10-15 procedures. With the correct individual selection of treatment parameters, this treatment method does not cause complications, patients note good tolerability of the procedures, and the trophic ulcer is quickly eliminated. Laser treatment, the price of which is not too high, is very popular.
Venous trophic ulcers. Basic principles of treatment.
Definition. A trophic ulcer of venous etiology is a defect of the skin and underlying tissues of the leg, resulting from a chronic disorder of venous outflow and not healing within six weeks.
Epidemiology
Venous ulcers are found in 1-3% of the adult population of Russia. The total number of patients with a history or currently suffering from venous ulcers of the lower extremities of venous etiology reaches 6% of the population. These data need to be clarified through targeted epidemiological studies.
Etiology and pathogenesis
The main nosological causes of the development of venous trophic ulcers are varicose and post-thrombotic disease, less often - congenital arteriovenous malformations.
Among the pathogenetic mechanisms, dynamic venous hypertension, venous edema and microcirculatory disorders with the development of microangiopathy, as well as molecular cellular mechanisms (macrophage reactions, activation of metalloproteinases, etc.), play a key role. Valvular insufficiency of perforating veins is an important, but not the only factor leading to the development of trophic skin disorders. This is evidenced by venous ulcers that develop in the absence of low venovenous discharge.
Classification
Closed trophic ulcers are classified as C5, open ulcers are classified as C6 clinical classes according to the CEAP classification.
Additionally, classifications describing the depth of the ulcer and its area can be used.
According to depth they are distinguished:
- I degree – superficial ulcer (erosion) within the dermis;
- II degree – ulcer reaching the subcutaneous tissue;
- III degree - an ulcer that penetrates into the fascia or subfascial structures (muscles, tendons, ligaments, bones), into the cavity of the articular capsule or joint.
By area they are distinguished:
- small, up to 5 cm2 in area;
- medium – from 5 to 20 cm2;
- extensive (giant) - over 50 cm2.
Features of clinical diagnosis
- Clinical examination with a thorough assessment of complaints and medical history.
- Identification of comorbid diseases affecting the course of trophic ulcers (diabetes mellitus, metabolic disorders, obesity, atherosclerosis, etc.).
- Assessment of vascular status with mandatory determination of pulsation in the arteries of the foot.
- Assessment of local status : in the vast majority of cases, venous ulcers are located on the inner surface of the lower third of the leg, less often they involve other surfaces of the leg or are circular in nature. A venous ulcer is a chronic wound, which is characterized by a combination of signs of all three phases of the wound process. However, from the point of view of choosing tactics for local treatment of a trophic ulcer, it is necessary to assess what phenomena prevail at the moment. The first phase of the wound process (inflammation) is characterized by the presence of necrosis and purulent discharge. Against this background, individual areas of the ulcer may be covered with fibrin, as well as flaccid and pale granulations. The edges of the ulcer and the surrounding tissue are compacted. The second phase of the wound process is characterized by the presence of bright granulation tissue. Active epithelization and scar formation are characteristic of phase III.
- Determination of the state of the peri-ulceral zone , which is characterized by the presence of hyperpigmentation, induration, lipodermosclerosis, and less commonly the phenomena of eczema and dermatitis.
Instrumental diagnostics
- Doppler ultrasound with ankle-brachial index measurement. A decrease in this indicator below 0.8 or an increase above 1.5 indicates the presence of serious concomitant arterial pathology.
- Ultrasound angioscanning when planning surgical intervention.
- X-ray contrast angiography or CT for suspected arteriovenous malformation.
Treatment of venous trophic ulcers
Treatment tactics
Treatment of trophic ulcers of venous etiology can be divided into two stages. The first stage involves closing the trophic ulcer using conservative measures. The second includes measures aimed at preventing relapse. This algorithm is successfully applied in 2/3 of patients. The indication for surgery for an active trophic ulcer is the ineffectiveness of adequate conservative treatment. In turn, the clear clinical effect of rational conservative treatment for 6 weeks allows us to recommend its continuation until the ulcer is completely closed.
Stage 1: closure of the trophic ulcer
Lifestyle correction.
- Diet. Limiting foods that contribute to fluid retention in the body (pickles, spicy seasonings, etc.). Preference should be given to vegetables and fruits high in vitamin C and bioflavonoids. It is advisable to expand the diet to include fish and poultry to ensure that the body receives easily digestible proteins. Attention must be paid to the prevention of constipation, which can increase venous hypervolemia of the lower extremities.
- Mode. Patients with venous trophic ulcers should not stand or sit for long periods of time. If the patient’s professional activity does not allow one to exclude prolonged static loads or exposure to high or low temperatures, it is necessary to be released from work until the trophic ulcer is completely closed or examined by the VTEK. During the night, the patient is recommended to keep his legs in an elevated position (15–20 cm above the level of the body).
Pharmacotherapy.
Antibacterial drugs . Indications for antibacterial therapy are signs of acute infectious inflammation of the soft tissues surrounding the trophic ulcer, or a high degree of bacterial contamination of 107 or more microbial bodies per gram of tissue. Ideally, culture is required to identify the microbial flora and determine its sensitivity to a specific antibiotic. It is also possible to prescribe drugs empirically, taking into account the most likely strains of microorganisms growing in venous trophic ulcers. Protected penicillins (ampiox, amoxiclav) can be first-line drugs. The use of 1-2nd generation cephalosporins (cephalexin, cefaclor, cefuroxime), as well as tetracyclines (doxycycline) is less preferable due to their isolated gram-positive spectrum of action. If high activity of Pseudomonas aeruginosa is suspected, carbenicillin, ticarcillin, azlocillin or piperacillin are used.
The persistent course of the microbial inflammatory process in the conditions of complex treatment of a trophic ulcer serves as an indication for microbiological culture with subsequent correction of the ongoing antibacterial therapy. Isolation of multiresistant strains determines the need for parenteral use of reserve group antibiotics (vancomycin, 3rd-4th generation cephalosporins, carbapenems) until the symptoms of acute cellulitis are completely resolved (on average 7-10 days). The presence of fungal flora in a trophic ulcer is an indication for the administration of fluconazole at a dose of 50–100 mg per day.
Phlebotropic drugs. RCTs and meta-analysis results show that MOFF (1000 mg per day) in combination with compression therapy accelerates the healing of venous trophic ulcers with an area of up to 10 cm² in up to 6 months. For other FLPs, there is no reliable data regarding their effectiveness in venous ulcers.
Local treatment of venous trophic ulcers.
Local therapy is a key stage in the treatment of trophic ulcers of venous etiology. The choice of specific therapeutic agents depends on the characteristics of the wound process, the condition of the tissues surrounding the trophic ulcer, and the limb as a whole.
Toilet trophic ulcer. When treating a trophic ulcer, jet washing of its surface with a sterile saline solution heated to 37°C can be considered optimal. The use of concentrated antiseptics (povidone iodine, hydrogen peroxide, miramistin, sodium hypochloride, etc.) traditionally used for acute wounds should be avoided. In conditions of trophic ulcers, they not only destroy microorganisms, but also have a cytotoxic effect, damaging granulation tissue. High-pressure lavage, including vortex therapy, is undesirable, as it promotes the penetration of microorganisms into the tissue and damages the microvasculature. Surgical debridement or debridement is performed when there is a large amount of necrotic tissue and fibrin. At the same time, during the procedure one should not strive to expose the bottom of the trophic ulcer.
Wound coverings. Local physicochemical conditions have a significant influence on the normal course of reparative processes in the area of the ulcer. On the one hand, excess humidity causes the death of epithelial cells. On the other hand, lack of moisture leads to drying out and slows down the epithelization process. Severe disturbances in the gas composition and acidity of the environment also adversely affect the functional cellular activity, and in certain cases create conditions for the activation of pathogenic microflora. It has been proven that a moist environment is necessary for wound self-cleaning, proliferation and migration of epithelial cells. With a sufficient amount of fluid in the extracellular matrix, looser fibrous tissue is formed with the subsequent formation of a less rough, but more durable scar.
The greatest prospects in the treatment of trophic ulcers of venous etiology are associated with the use of new generation wound coverings. The main objectives of such dressings are:
- irreversibly remove detritus, microbial particles and excess exudate;
- protect from mechanical influences, chemical irritation and
secondary infection;
- keep the ulcer surface moist,
preventing it from drying out and forming a dry scab;
- help increase the reparative resources of local tissues;
- maintain microcirculation and oxygenation of the edges of the ulcer;
- have a beneficial effect on the surrounding skin, protect it from maceration,
allergies and dermatitis;
- stay on the wound and be removed painlessly and atraumatically;
- retain their properties when combined with elastic compression in
over a long period of time (a day or more);
- be easy to use and comfortable for the patient.
The so-called interactive dressings have all of the above properties to the greatest extent (Table 8). These are bandages of complex pathogenetically targeted action, capable of creating and maintaining in the pathological focus for a long period of time an optimal wound environment for healing with a balanced level of humidity and sorption of wound exudate and, as a result, ensuring timely cleansing and normalization of reparative and regenerative processes in the wound. Interactive dressings, as a rule, have low adhesion to the wound surface and are able to maintain a constant gas composition and pH level of tissues.
Table 8. Modern dressings used for the treatment of venous trophic ulcers.
| Groups of dressings | Wound process phase | Degree exudation | Functional properties |
| Super-absorbing titels | 1 — 2 | Wounds with moderate or severe exudation | Absorb liquid, promote rapid wound cleansing, stimulate proliferation processes, and have low adhesion. Protects against recurrent and secondary infection. Pairs well with elastic compression. |
| Sponge- thin bandages | Vapor permeable. Actively absorb liquid, maintaining a balanced, moist environment. Clean the ulcer surface from fibrin. Stimulate granulation, protect the skin from maceration. Hydrophilic sponges protected by a hydroactive gel layer allow for local treatment from the moment of cleansing to complete epithelization of the ulcer. Pairs well with elastic compression. | ||
| Algi- natural headbands | Irreversibly binds fluid, maintaining a balanced moist environment and promoting wound cleansing, drainage and hemostasis. Stimulates the growth and development of granulation tissue. Do not interfere with microcirculation and oxygenation of the edges of the ulcer. Require additional use of secondary dressing and fixation means. | ||
| Hydro- gels | 2 — 3 | Minimal exudation wounds | They create and maintain a moist environment for a long time and are transparent. Moderately absorb and clean, reduce pain, non-adhesive. |
| Hydro- colloids | 2 | Wounds with small or medium exudation | Vapor permeable. Partially permeable to air. Absorb liquid, stimulate granulation and epithelization, protect against secondary infection. |
| Atraumatic mesh dressings | All phases | Well permeable, easily modeled on wounds of complex configuration. They do not stick to the wound, protect granulations, but require the additional use of a secondary dressing and fixation means. |
The choice of one or another dressing requires mandatory consideration of the phase of the wound process and the degree of exudation. Thus, dressings, the use of which is rational in the inflammation phase, due to the structure of their material, are capable of inactivating wound exudate, promoting the irreversible elimination of microorganisms, toxins and tissue detritus, while stimulating the process of rejection of necrotic tissue. In turn, coatings used in the treatment of “clean” healing ulcers maintain the necessary humidity and aeration, reliably protect against mechanical damage and secondary contamination, and stimulate reparative processes.
Atraumaticity and safety are the most important properties of modern interactive dressings. Non-traumatic means that the coating can be easily removed due to the low degree of adhesion to the wound surface. Safety means the absence of mechanical and chemical irritation, as well as hypoallergenicity. An additional advantage is their modeling ability, which allows closing a wound defect of any shape in various parts of the body. Many wound dressings are self-adhesive or have an additional self-adhesive edge treated with a hypoallergenic adhesive. Such dressings should only be used in patients with normal skin sensitivity in the absence of dermatitis and/or eczema. Modern interactive dressings are produced in ready-made sterile packaging, with markings that ensure ease of use.
Superabsorbents are capable of absorbing and irreversibly sorbing wound discharge. They are a multilayer pad that contains as an active substance a granular polyacrylate superabsorbent that has a high degree of affinity for wound fluid proteins. The saline solution, which soaks the wound covering continuously for 24 hours, is released into the wound and replaced by exudate, providing wound dialysis and microbial decontamination. Moisturizing necrosis helps to soften it, make it easier to reject and clean the wound. Currently, further improvement of the “washing-absorption” mechanism, reducing adhesive properties and creating conditions for complete irreversible inactivation of absorbed microflora through the introduction of the antiseptic polyhexamethylene biguanide (PHMB) into the absorption element makes it possible to increase the intervals between dressings to 72 hours without the threat of re-infection of the ulcer.
Alginates are produced from seaweed. They are based on the calcium salt of alginate acid, as well as polymer chains of mannuronic and hyaluronic acids. Alginate dressings are placed in the wound dry. Upon contact with blood and wound secretions, due to the swelling of the fibers, they turn into a hygroscopic non-adhesive gel that fills the wound. In this case, microorganisms and toxins are reliably bound in the gel structure. As a result, wounds are quickly cleansed and a microclimate favorable for healing is created. A prerequisite for the use of calcium alginate-based dressings is the presence of fluid in the wound. The dressing is used in all phases of the wound process with moderate and severe exudation up to complete epithelization. Calcium alginate has hemostatic properties and can be used to treat deep and/or bleeding ulcers. Contraindications to the use of calcium alginate-based dressings are dry necrotic scab and the presence in the wound of elements that are not a source of granulation tissue growth (abundance of open tendons, joint capsules, periosteum, etc.).
Sponge dressings consist of synthetic spongy materials, the therapeutic effect of which is based on the effect of vertical capillarity and low adhesion. They are able to create a balanced environment on the wound surface, stimulate the growth of granulation tissue and isolate the ulcer from secondary infection. Used in the treatment of trophic ulcers with abundant exudation in the first and second phases of the wound process. The advantage is that the structure of the material allows them to be combined with elastic compression without reducing the sorption properties of the wound covering. The indication for changing the dressing is its complete saturation with exudate, manifested by leakage of liquid or deformation of the outer layer of the coating.
Currently, hydrophilic sponge dressings protected by a hydroactive atraumatic coating have been developed and introduced into the domestic market. A mesh atraumatic hydrogel coating with an initial 35% moisture content, which is the contact layer of the dressing, can significantly reduce the adhesion of the sponge to the wound surface and effectively moisturize even a dry ulcerative surface. The prolonged release of fluid with such a dressing allows you to ensure the necessary balance of moisture and sorption from the moment the ulcer is cleansed of detritus until its complete epithelialization. The bandage also does not lose its properties if elastic compression is used and can remain on the wound for an average of 3-5 days.
Hydrocolloids are used in the 2nd phase of the wound process. Upon contact with wound exudate, the colloidal component swells and turns into a gel. The main advantages of these coatings include good fixation to the wound surface, high atraumaticity, and easy modeling of the shape of both the limb and the ulcerative defect. The disadvantage of hydrocolloids is their opacity, which makes it difficult to visually monitor the condition of the wound defect. The saturation of hydrocolloids and loss of sorption activity is indicated by the deformation of the bandage in the form of a bubble and a change in its color. When changing the dressing (on average every 2-3 days), the remainder is removed from the wound surface with a damp swab. Low sorption capacity, as well as insufficient permeability to gases and water, limits the use of hydrocolloids in severe exudative processes.
Hydrogel dressings are a ready-made sorption gel fixed on a transparent semi-permeable membrane containing up to 60% water and possessing moderate sorption activity. The gel maintains a constant shape and keeps the wound moist while absorbing excess secretions. These coatings are used to rehydrate dry necrotic scab or stimulate epithelization of granulating ulcerative defects. Hydrogel-based dressings do not stick to the wound, which makes them highly atraumatic. The outer surface of the coating is impermeable to microorganisms and water and at the same time transparent. The last factor makes it possible to visually monitor and record the condition of a trophic ulcer without removing the bandage. The indication for changing the coating is its cloudiness and loss of transparency.
Atraumatic mesh dressings are made on the basis of a neutral hypoallergenic hydrophobic ointment mass or Peruvian balsam. They have an antiseptic effect and stimulate tissue repair. The advantage of atraumatic mesh dressings is the ability not to stick to the wound and not to interfere with the outflow of excess wound fluid. Along with being atraumatic, this factor protects the coatings from drying out and prevents the formation of scar contractures. Silver-containing atraumatic dressings have a more significant antimicrobial effect. Upon contact with the wound surface, there is a slow, uniform release of active silver particles, which have a wide spectrum of antimicrobial activity. The service life of such a dressing, subject to moderate exudation, is 7 days. Atraumatic dressings are used to cover donor sites during autodermoplasty of trophic ulcers.
Additional methods of local treatment of venous trophic ulcers. Additional methods of local therapeutic effects on the area of a trophic ulcer include laser irradiation, vacuum treatment of the wound, its biological sanitation and treatment in a controlled abacterial environment.
Laser radiation. The use of laser radiation is rational in the first phase of the wound process. When treating an infected wound, its surface layers are evaporated to form a thin-walled, sterile scab. These processes are accompanied by a significant decrease in the degree of microbial contamination of the ulcer. The greatest therapeutic effect of laser radiation was obtained when affecting trophic ulcers of a small area.
Vacuum treatment of trophic ulcers . Vacuuming is one of the methods of sanitation of chronic wounds, which can also be applied to trophic ulcers of venous etiology. The main pathogenetic aspects of vacuuming are the removal of weakly fixed non-viable tissues, a significant reduction in the degree of bacterial contamination of tissues and stimulation of reparative processes. Improving stationary and mobile devices that provide prolonged vacuum exposure, equipping them with a dialogue program and an emergency warning system, makes it possible to solve the problem of treating chronic wounds at a completely new level.
Biological rehabilitation of trophic ulcers . Currently, there is renewed interest in the method of cleansing purulent-necrotic ulcers using green fly larvae (Larval therapy). Specially grown larvae, when placed in a wound, have a cleansing effect through the release of powerful proteases. Under their influence, devitalized tissues undergo necrolysis, become amorphous and are absorbed by the larvae. The main problem of biological sanitation of trophic ulcers is the ambiguous ethical and aesthetic perception of the method by doctors and patients.
Treatment of trophic ulcers in a controlled abacterial environment. The method of bandage-free treatment of extensive purulent wounds in a controlled abacterial environment is based on the principle of gnotobiological isolation. The area of ulcerative defects is isolated from the external environment in a transparent plastic chamber and a stream of sterile air is constantly supplied to it, creating an optimal environment for wound healing. The disadvantage of the method is its cumbersomeness, the possibility of performing it only in a hospital setting, as well as a significant reduction in the quality of life of the patient who is forced to observe strict bed rest for a long time.
Compression therapy is a necessary component of the treatment of venous trophic ulcers and the prevention of their recurrence. In case of an open ulcer with symptoms of venous edema, cellulite and exudation, preference is given to multilayer bandages formed from bandages of limited extensibility. To prevent relapse, medical compression stockings are usually used.
Algorithm for local treatment of venous trophic ulcers
Ist phase of the wound process. A large amount of necrotic masses and fibrin is an indication for the use of wound dressings from the superabsorbent group in combination with a multilayer compression bandage. The dressing is changed daily. For high or moderate exudation, it is recommended to use sponge, alginate or atraumatic dressings with antiseptic properties in combination with secondary sorption dressings. The antibacterial properties of drainage and sorption dressings can be enhanced by the additional use of atraumatic silver-containing coatings. Wound coverings and compression bandages are applied for at least 24 hours. If the swelling subsides quickly, then the bandage is changed daily, regardless of the type of interactive bandage.
II phase of the wound process. For high or moderate exudation, sponge dressings are used. If the skin surrounding the ulcer is hypersensitive, sponge dressings with a fixing contour should be avoided. At low and medium levels of exudation, in the second phase of the wound process, hydrophilic sponges protected by a hydroactive gel layer or hydroactive occlusive dressings are used, which best stimulate the healing of a chronic wound. Only with a minimal level of exudation in the second phase of the wound process can one abandon the use of wound occlusion in favor of atraumatic dressings, which can be considered as the treatment of choice in the treatment of chronic wounds in conditions of moderate or low exudation with sensitive skin surrounding the ulcer. For normal skin sensitivity, the preferred local treatment option in the second phase is hydrocolloid dressings, which best stimulate the formation of granulations.
In conditions of an actively granulating trophic ulcer, both in the presence of edema and in its absence, compression therapy can be carried out using a multilayer bandage, including special bandages impregnated with zinc oxide and glycerin.
III phase of the wound process. During the epithelialization stage, the algorithm for local therapeutic effects on venous ulcers is somewhat simplified due to a significant reduction in the severity of exudative processes. For normal skin, it is possible to continue treatment with sponge dressings with a hydroactive layer, as well as local application of thin-layer hydrocolloid and hydrogel dressings. For sensitive skin, the optimal treatment option is hydrogel coatings without a fixing contour or hydroactive atraumatic dressings. As a rule, at this stage of the pathological process, swelling of the limb is insignificant, which makes it possible to widely use medical compression hosiery. If swelling of the limb persists, multi-day compression bandages are used.
Surgery
Obtaining a clear clinical effect from conservative therapy for 6 weeks, consisting in reducing the area and depth of the trophic ulcer, improving the trophism of surrounding tissues, eliminating edema and pain, allows us to recommend its continuation until the complete closure of the trophic ulcer. With an active trophic ulcer, the indication for surgery is the ineffectiveness of adequate conservative treatment.
All types of surgical interventions performed in patients with trophic ulcers can be divided into two groups. In the first case, the task of the surgical treatment is to eliminate pathological regional venous hypervolemia, in the second - plastic closure of the trophic ulcer.
Operations on the superficial venous system
For varicose veins with high venovenous discharge, a crossectomy is performed followed by stripping of the great saphenous vein on the thigh. Extended phlebectomy on the lower leg, which is fraught with purulent-necrotic complications, should be avoided. In high-risk patients, as well as as a means of eliminating residual varicose veins, phlebosclerosing treatment, laser and radiofrequency coagulation are used.
Interventions on perforating veins
To eliminate horizontal reflux, endoscopic dissection of perforating veins is used, as well as their scleroobliteration or thermal coagulation under ultrasound control.
Deep vein interventions
Surgical interventions on the deep venous system (plasty of venous valves, shunt operations) in patients with trophic ulcers are performed in an extremely limited group of patients in case of failure of all other treatment methods.
Skin grafting
A large area of trophic ulcer sometimes requires surgical repair of the tissue defect. For this purpose, autodermoplasty with a split skin flap is used, both as an independent method and in combination with intervention on the saphenous and perforating veins.
As a rule, the anterolateral surface of the thigh is used as a donor area. A skin flap with a thickness of 0.5 – 0.8 mm is collected using a mechanical, or less commonly, a manual dermatome. After application of donor skin over the entire area of the trophic ulcer, the wound surface is covered with a non-adhesive bandage and a compression bandage is applied for 3 to 5 days. In order to close the donor area, it is most rational to use atraumatic mesh bandages.
Trophic ulcer - laser treatment (EVLO, EVLK)
A more radical method of treating trophic ulcers is surgery using laser coagulation (Endovasal laser coagulation). We have been using the EVLT technique for many years. This treatment method consists of “burning out” the vein, which is located in the area of the trophic ulcer. The results are very good: the ulcers heal almost before our eyes. Scarring occurs over several weeks. At the same time, patients do not fall out of their normal routine of life.
Treatment of trophic ulcers with laser in
Laser treatment of trophic ulcers in Moscow has a number of advantages:
- low morbidity - the phlebologist does not make additional incisions in the ulcerated area;
- the ability to avoid long-term conservative treatment before surgery;
- high efficiency - scarring of the ulcer goes away quite quickly;
- positive cosmetic effect - low tissue trauma eliminates the formation of rough scars when the trophic ulcer disappears. Laser treatment, the cost of which can be discussed upon admission, will help you.
Examples of patients with diabetic ulcers treated in our clinic
Patient Lukyanov V.N., 75 years old.
Diagnosis: Diabetes mellitus type II. Diabetic foot syndrome, mixed form. Upon admission: Phlegmon of the right foot, in bone tissue cultures - abundant growth of Pseudomonas aeruginosa, St. aureus, Enterococcus faecalis. This patient literally ran to us from the purulent surgery department of one of the clinics in our city, where his foot was going to be amputated. His troubles began with inflammation and then phlegmon of the fourth toe of his right foot. He was hospitalized at this purulent surgery department, where he underwent amputation of the fourth finger. Then, during a month of hospitalization, due to the progression of purulent inflammation, his third and second fingers were amputated. Despite this, the infectious process spread to the foot and the patient developed phlegmon of the foot. They began to prepare him for amputation.
Upon admission to our clinic, the patient had severe pain, severe hyperemia and tenderness of the sole, exposed bones were visible in the wound, and there was a purulent discharge with a disgusting odor. We immediately performed bone culture. It contains abundant growth of Pseudomonas aeruginosa (Pseudomonas aeruginosa), St. aureus (Staphylococcus aureus), Enterococcus faecalis (fecal enterococcus).
For treatment in this case, we used a portable vacuum-flushing system that we developed. In it, the beneficial effect of negative pressure on wounds is enhanced by the effect of antiseptics used for washing. In addition, in the case of ischemic ulcers, overdrying of the wound surface is avoided. These systems have proven themselves well for the treatment of severe purulent wounds. In this case, the patient, as you can see in the picture, is mobile - treatment is carried out on an outpatient basis:
After the first dressings, the pain in the wound and the unpleasant odor almost completely disappeared, the pain decreased and the hyperemia on the sole was limited. Soon the ulcer significantly decreased in size, was filled with granulation tissue, and the culture results were negative. The patient underwent branded autodermoplasty:
All treatment took place on an outpatient basis. In the pictures below you can see the right foot of this patient at the time of admission to our Center and at discharge:
The following photographs show the foot of a 66-year-old patient before and after treatment in our clinic. She has an ischemic form of diabetic foot syndrome. The exposed bones of the left foot are visible.
Patient M., 66 years old. Diagnosis: Diabetes mellitus type II. Diabetic foot, ischemic form. Obliterating atherosclerosis. Occlusion of the arteries of the left leg
It all started with an ulcer of the first finger, after which, despite inpatient treatment in one of the leading clinics in St. Petersburg, several amputations followed, as a result of which necrosis spread to the foot. And at the time of admission to our clinic, the ulcer looked as shown in the first picture.
We were able to restore the skin through systemic antibacterial therapy and local treatment. Perforations were made in the bones, and the growth of granulations from these holes was stimulated through cell therapy. Then autodermoplasty was performed. Again, due to cell therapy, it was possible to achieve engraftment of the transplanted skin flap.
Obliterating endarteritis, also known as Buerger's disease, also known as Winivarter-Buerger disease, is characterized by inflammation that primarily affects the peripheral arteries in young smokers. The photo shows the leg of a patient with obliterating endarteritis, treated in our clinic.
With this disease, there is a very strong dependence on smoking: this disease does not occur in non-smokers, and if you quit smoking, the prognosis is favorable. Initially, the arteries of the distal parts of the feet become inflamed and close, then the disease spreads proximally. When the popliteal arteries are involved, intermittent claudication will occur. Therefore, the Fontaine-Pokrovsky classification does not apply here: ulceration and gangrene may precede intermittent claudication. Diagnostic criteria for the disease are presented below.
Trophic ulcer - radiofrequency treatment (RFA, RFO)
The radiofrequency treatment method is considered the most modern and safe if you have a trophic ulcer. RFA treatment in Moscow involves heating the walls of the vein with microwaves, it “closes”, and the trophic ulcer gradually shrinks. RFO treatment - and after a few months the problem vein is a connective tissue cord, and the entire load is transferred to neighboring, healthy vessels. This is how the trophic ulcer gradually heals.
Treatment of trophic ulcers with radiofrequency (RFA, RFO) in our center
RFO treatment in Moscow is carried out quite quickly; the patient goes home 10 minutes after the intervention. The radio frequency method provides the following advantages:
- short duration of the procedure - 30-40 minutes;
- exposure parameters are selected automatically and without the participation of a doctor;
- cosmetic effect - the absence of additional trauma promotes the formation of a less rough scar where there was a trophic ulcer. RFA treatment is very positive in this regard.
- the procedure is completely painless and easily tolerated;
- Hospitalization is not required, the patient can lead a normal life, limiting activity only after the procedure.
Is a diet necessary when treating a trophic ulcer?
What should be avoided if there is a trophic ulcer? Photos of complications will help you control yourself when dieting. Diet for trophic ulcers excludes salty foods and spices. It is necessary to saturate the body with nutrients, vitamins and Omega-3 acids. Vegetables (carrots, tomatoes, cabbage), fruits, nuts, milk, cheeses, vegetable and butter, and fish are especially useful. You should eat small portions to avoid a sharp increase in blood sugar. A radical change in diet is not required; a small adjustment will have a beneficial effect on the healing process.
Trophic ulcer - prevention
To prevent the trophic ulcer from returning and the treatment not to be in vain (the cost of which can only be found out after consultation), take care of prevention. Measures to prevent the occurrence of trophic ulcers and relapses:
- early detection and treatment of diseases that provoke the appearance of trophic ulcers;
- moderate physical activity (daily walking 2-3 km);
- use of compression hosiery;
- ignoring baths and saunas, hardening procedures for the legs;
- refusal of flour and sweets, predominance of fruits and vegetables in the diet;
- medical examination 2 times a year.
Frequently asked questions from our patients on the Internet about trophic ulcers
How to treat non-healing wounds on the legs?
To effectively treat non-healing leg wounds, it is necessary to understand how such wounds appeared. Long-term non-healing wounds on the legs can form as a result of a number of completely different pathologies, and each requires its own specific treatment.
How to treat non-healing wounds at home?
Before you begin to treat long-term non-healing wounds at home, you need to find out the cause of such wounds. Most often this is:
- Diabetes.
- Obliterating atherosclerosis.
- Chronic venous insufficiency.
If you want to cure long-term non-healing wounds, then in addition to the local use of ointments, it is necessary to deal with the underlying pathology that caused the problem.
How to treat a deep wound?
How to treat a deep wound should be asked to the doctor during an in-person consultation. Treating such wounds on your own, using the Internet, can be fraught with progression of the process and the development of a life-threatening condition.
My father developed sores on his legs six months ago, how can I get rid of them?
If “sores” on your legs appear and do not go away for a long time, as a rule, only a doctor will help you get rid of them. Long-term non-healing wounds are often a sign of a serious pathology that requires specific treatment.
Trophic ulcer - treatment. Reviews from our patients.
Patient's review of laser treatment for trophic ulcers in our center.
Victor Petrovich, 65 years old.
I am a pensioner with a whole cartload of all sorts of ailments. My legs had been hurting and swollen for a long time, but I, like many, put off going to the doctor until later. I took some pills on the advice of a neighbor nurse, although I didn’t notice any particular improvement. In general, I lived to the point where I had a huge ulcer on my leg. God bless your doctors, I already thought that I would be left without a leg. They gave me laser treatment. I didn’t particularly delve into the nuances of this case; the doctors guaranteed a good result. Everything went without pain, literally after a few days my trophic ulcer began to disappear before my eyes, and after two weeks only a small scar remained. Of course, various medications were prescribed, then I went to a sanatorium and forgot about this terrible disease. Thanks to all the doctors of the Medical Center for Phlebology, especially Dr. Malakhov Alexey Mikhailovich.
A patient's review of the treatment of trophic ulcers using the EVLO method in our center.
Komissarova L.I.
Our patient with surgeon-phlebologist A.M. Malakhov. after treatment
My leg ached constantly, there was a buzzing sensation in it at the end of the day, and then a trophic ulcer formed, which became larger and larger. I didn’t dare to have surgery using the classical method, because I was afraid after reading reviews online and all sorts of complications. Well, my daughter is in the know, she found me an experienced doctor in Moscow, Alexey Mikhailovich Malakhov. Before the operation, and this is endovasal laser coagulation, at the medical center in Moscow, where I decided to have it, they did an ultrasound, donated blood and that’s it. After the operation, I was forced to get up from the table and walk for about an hour. After 3 weeks I saw my doctor. I didn’t worry about scars, the main thing was that the ulcer healed faster. It's been 3 months since the laser procedure on my leg. Everything is fine, the ulcer has become very small, but I hope it will heal completely soon.
I'm very glad that everything went well. Thanks for all. Komissarova Lyudmila Ivanovna, December 7, 2016
Examples of patients with venous ulcers treated in our Center
Patient N., 24 years old Diagnosis: Varicose veins of the left lower limb. After complete healing of the trophic ulcer (this took 1 month), the patient underwent outpatient surgery - he underwent removal of the varicose great saphenous vein. In the second photograph, taken three weeks after the operation, traces of punctures are still visible, through which this vein destroyed by varicose disease was removed. The patient is observed for 9 years after the operation - there is no recurrence of the ulcer.
Patient Alexandrova L.B., 66 years old, before and after outpatient treatment in our Center. Diagnosis: Postthrombotic disease of the left lower limb. Circular trophic ulcer of the left leg. The photo shows a galosh that filled with lymph every half hour of walking. The clinic website has
.
The story of this patient was described by a journalist who interviewed her for an article about Andreev D.Yu. "Healing Man":
“The professional life of an obstetrician-gynecologist is a struggle for the health of patients. This is what Lyudmila Borisovna Alexandrova did. At the age of sixty, she herself became a patient. Now I can’t even remember all the offices of vascular surgeons, phlebologists, lymphologists, where they tried to fight her trophic ulcer. Everywhere - to no avail. She walked with a huge man's galosh on her foot. The ulcer that consumed her body released lymph that flowed down her leg. Every half hour it was necessary to pour one and a half glasses of this liquid out of the galoshes. I was constantly in pain... After six years of such a life, Alexandrova, in a fit of despair, wrote a letter to the Minister of Health (T. Golikova).
The administrative-bureaucratic machine began to move and got the head doctor of the local clinic when the writer was at the dacha. There she was found by an ambulance sent by the chief. They were admitted to the hospital (“St. George”). A council was quickly assembled, headed by a professor, one of the city’s leading lymphologists. Conclusion of venerable specialists: amputation, urgently.
“As a surgeon,” Lyudmila Borisovna recalls now, “I myself understood that with a circular ulcer there are only two outcomes: amputation or death. But how hard it is to give up hope!…
The night passed without sleep. In the morning, no longer remembering why, she went downstairs. There's a newsstand in the lobby. On the counter lay the magazine “Prevention, Health, Beauty.” I took it...
I started calling. I contacted vascular surgeon Andreev. Friendly voice, clear, specific questions. And then confident: “I will cure you”...
On the same day, Lyudmila Borisovna left St. George. The next day I met with Andreev. It was the end of November. In May, she parted ways with her six-year curse, an aggressive circular ulcer.
“I have no words to express my gratitude,” says the healed woman. “I think as many people as possible should know about this doctor.”
She herself spoke about it in a letter to Elena Malysheva, Doctor of Medical Sciences, professor, one of the creators of the “Calling” project, who hosts the “Health” program on Channel 1 TV. But either the letter did not arrive, or the respected professor and TV presenter, like some of Andreev’s colleagues in St. Petersburg, also sometimes use the formula: “This cannot happen, because it never happens” ... "
We examine all patients with venous ulcers for concomitant arterial pathology. And if it is present, we determine the ankle-brachial index. This is important for prescribing adequate compression therapy. Here is an example of such a patient:
Patient Sh., 65 years old. Diagnosis: Postthrombotic disease of the left lower limb. Obliterating atherosclerosis. Occlusion of the superficial femoral, popliteal and anterior tibial arteries. Ischemia stage III ABI 0.5.
Thus, this patient has a combined lesion of the veins and arteries of the left lower limb. Stage 3 ischemia means that due to a sharp decrease in arterial blood flow, the patient cannot remain in a horizontal position for a long time - severe pain occurs; at night he is forced to sleep with his leg off the bed or sitting. In one of the clinics in St. Petersburg there was an attempt - unsuccessful - to restore arterial blood flow. By using the technologies we developed, we - without vascular surgery - managed to improve blood supply and significantly cleanse the ulcer. Then we performed skin grafting:
Complete healing of ulcers – after 8 months of treatment:
All treatment, including skin graft surgery, was carried out on an outpatient basis; hospitalization in our clinic was not required.
Usually located in the distal parts of the limb; surrounded by pale or cyanotic skin. Typical localization is the toes, forefoot and heel area (especially in bedridden patients). They are less common on the dorsum of the foot, on the anterior surface of the lower leg and in the area of the lateral and medial ankles. In the last two cases, they can mimic venous ulcers. Provoking factors are minor skin injuries (for example, when wearing tight shoes). The bottom of the ulcer is usually necrotic tissue; There are few granulations, they are pale. As a rule, there is no swelling of the lower limb. Unlike venous ulcers, which almost never penetrate deeper than the proper fascia of the leg, with these ulcers there are frequent cases of exposure of tendons and bones. Other distinctive features are a small amount of wound discharge and the lack of severity of the inflammatory reaction in the tissues surrounding the ulcer, even at the first stage of the wound process. Another difference from ulcers of venous etiology is that raising the affected limb above the level of the heart increases the pain, and does not alleviate it, as with venous ulcers.
The main contingent of patients are elderly men. Since in obliterating atherosclerosis ulcers are a manifestation of stage IV of arterial ischemia (according to the Leriche-Fontaine-Pokrovsky classification), their occurrence is preceded (and accompanied) by the appearance of a symptom of intermittent claudication (stage II) and pain in the distal parts of the limb at rest (primarily - in a horizontal position) – stage III of ischemia.
When examining the patient, the absence of pulsation of the popliteal artery and arteries of the foot is revealed - the main criterion for distinguishing these ulcers from ulcers of venous etiology.
Ultrasound duplex scanning of the arteries of the lower extremities allows confirmation and clarification of clinical findings.
The photographs below demonstrate modern treatment options for these ulcers.
Patient R., 70 years old.
Diagnosis: Obliterating atherosclerosis. Occlusion of the right superficial femoral, popliteal and anterior tibial arteries. Trophic ulcer of the right leg. Purulent arthritis and fistula of the right ankle joint. Ischemia stage IV Concomitant diagnosis: type II diabetes. ABI 0.2. Systolic pressure at a. tibialis post. 30 mmHg This patient came to our clinic with very severe pain. There is a terrible ulcer on my only right leg. You can see the exposed ankle joint. Note that the ulcer is in a typical location for venous ulcers, although the patient's veins are normal.
To cure this patient, it was necessary to perform an autovenous femoral-tibial bypass with an autovenous vein, after which it became possible to heal the ulcer through local treatment:
The patient has been observed for 11 years - there is no recurrence of the ulcer.
Trophic ulcers in diabetes mellitus are manifestations of diabetic foot syndrome and/or diabetic necrobiosis lipoidica.
According to the international classification (Netherlands 1991), neuropathic, ischemic and mixed (neuroischemic) forms of this syndrome are distinguished. Differential diagnosis of neuropathic and ischemic forms of diabetic foot syndrome is given in the table.
Diabetic ischemic foot syndrome (and ulcers associated with this syndrome) are caused by atherosclerotic damage to the arteries of the lower extremities of diabetic patients. It is well known that diabetes mellitus is one of the leading risk factors for obliterating atherosclerosis. Thus, despite the differences in atherosclerotic damage to the arteries of the lower extremities in patients with and without diabetes mellitus (see table below), ulcers in ischemic diabetic foot syndrome are more correctly classified as atherosclerotic trophic ulcers, considering diabetes mellitus as a concomitant disease.