Testicular cyst (spermatocele) is a fairly common disease of the scrotum. It is found in every third man during an ultrasound.
A testicular cyst in men is a cystic formation in which fluid accumulates. Usually there is a smooth, soft, well-defined cyst that is located in the area of the epididymis. Cyst formation occurs in the excretory ducts through which sperm move.
Epididymal cysts are benign. Sometimes a testicular cyst is confused with hydrocele, varicocele, hernia or other tumors.
According to scientists, if a patient develops a cyst on the left testicle, the volume of fluid in it will be much greater than when a testicular cyst forms on the right side. Most often, there is very little or no fluid in the right testicular cyst.
Classification
The most common of all testicular tumors are germ cell tumors; they develop from germ cells. With the right tactics, these tumors can be completely cured, but an important condition is their timely detection and treatment in a specialized center.
Germ cell tumors (account for 95% of testicular tumors)
- seminoma,
- nonseminoma (embryonic carcinoma, yolk sac tumor, postpubertal teratoma).
Sex cord and stroma tumors (<5% of all testicular cancers)
- Leydig cell tumor
- Sertoli cell tumor
- granulosa cell tumor.
Other tumors (the proportion of all cases of testicular tumors is not precisely determined)
- hemangioma,
- adenocarcinoma.
Complications
The main thing that patients suffering from testicular varicose veins need to understand is the serious situation with the appearance of offspring. Infertility can become a sad complication of varicocele, so you should not delay going to the clinic for diagnosis and treatment. Doctors from the Global Clinic Center can provide qualified assistance. Statistics show that patients diagnosed with varicocele in 60 cases out of a hundred are faced with the problem of sperm dysfunction. 40% of men with testicular varicose veins become infertile.
Risk factors for developing testicular tumors
There are no clear risk factors for developing testicular tumors. One of the most likely causes is cryptorchidism - undescended testicle. With normal development, the testicles are located in the abdominal cavity before birth and by the time the child is born, they descend independently into the scrotum. In about 3% of children, one or both testicles may not descend into the scrotum. In such cases, surgery is performed. Surgical treatment of cryptorchidism before puberty reduces the risk of developing testicular tumors.
Cryptorchidism
Occupational activity may increase the likelihood of developing a testicular tumor; it is believed that workers in the gas and oil industries, miners and firefighters have an increased risk of developing a testicular tumor. White men are 5 to 10 times more likely to develop a testicular tumor than African American men. Asian and African men have a very low risk of developing a testicular tumor. Trauma and surgery on the genitourinary organs do not significantly increase the risk of developing testicular tumors.
Advantages of Marmara microsurgery:
- A small cosmetic incision in the groin area, in the hair growth area (the scar is almost invisible)
- The greatest efficiency of the operation is achieved through the use of operating binoculars and microsurgical instruments
- Lowest percentage of relapses and complications (less than 5 percent)
- Can be performed on an outpatient basis, without hospitalization
- Short and easy postoperative and recovery period
I am aware of my responsibility for preserving the main thing that my patient trusts me, and I will do everything to justify the trust!
Diagnostics
A testicular tumor may appear as a painless mass on the scrotum or testicle. The table below lists possible symptoms.
With a widespread process, the patient may be bothered by various symptoms: cough, shortness of breath, back pain, headaches, nausea, vomiting. If you experience these symptoms, you should urgently consult an oncologist or urologist.
Our doctors
Khromov Danil Vladimirovich
Urologist, Candidate of Medical Sciences, doctor of the highest category
Experience 36 years
Make an appointment
Kochetov Sergey Anatolievich
Urologist, Candidate of Medical Sciences, doctor of the highest category
35 years of experience
Make an appointment
Perepechay Dmitry Leonidovich
Urologist, Candidate of Medical Sciences, doctor of the highest category
41 years of experience
Make an appointment
Testicular tumor symptoms
A testicular tumor can be detected by the patient or his sexual partner. If any formation is detected in the testicle, you should immediately consult a doctor.
To detect a testicular tumor in a timely manner, we recommend performing a self-examination.
Testicular self-examination
Most often, testicular tumors are confused with inflammatory diseases. Epididymitis is an inflammation of the epididymis, in most cases of an infectious nature, requiring anti-inflammatory therapy. If tenderness and swelling persist after a course of treatment, including antibiotics, further diagnosis is necessary.
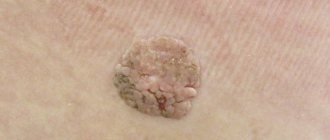
Testicular tumor
Examination of a patient at a doctor's appointment begins with an examination. The doctor will perform an examination, palpation of the chest for gynecomastia (enlarged mammary glands), abdominal cavity, testicles, and assess the condition of the inguinal and peripheral lymph nodes.
Severity of acute epididymitis
The transition of the pathology to the acute stage is accompanied by pronounced symptoms. There are 3 stages in total: mild, moderate, severe:
- Mild – lasts up to 3 days. An ultrasound reveals an enhanced vascular pattern, and a blood test shows an increase in leukocytes to 12,000.
- Moderate – lasts up to 6 days and has severe symptoms, including an increase in body temperature to 39 degrees Celsius and pain. Ultrasound examination reveals inflammation and hypoechoic neoplasms up to 10 mm.
- Severe – lasts more than 7 days and is accompanied by severe symptoms. A blood test shows a leukocyte count of up to 25,000, which indicates a strong inflammatory process (body temperature rises to 40 degrees Celsius). The accumulation of pus is maximum, the epididymis is significantly enlarged.
Instrumental methods
Ultrasound examination (US) of the scrotum is the preferred initial imaging study for assessing testicular mass. Ultrasound can confirm the presence of a neoplasm, determine its location and assess the condition of the opposite testicle (Fig. 4). The sensitivity of the method is quite high - from 92% to 98%.
Computed tomography of the chest, abdominal cavity, and pelvis is used to assess the spread of the tumor process (Fig. 5).
As an additional diagnostic procedure, magnetic resonance imaging of the brain can be used.
A prerequisite for diagnosing testicular tumors is a blood test for biological tumor markers. These include AFP (alpha fetoprotein), β-hCG (β unit of human chorionic gonadotropin) and LDH (lactate dehydrogenase).
The presence of a tumor formation in the testicle, detected by ultrasound, and an increased level of tumor markers (all or one of them) require immediate referral of the patient for surgical treatment to a specialized oncology center.
If a primary tumor is detected in the retroperitoneal space, it is necessary to undergo a full examination provided for a testicular tumor.
Ultrasound image of the testicle
How does epididymitis manifest?
The most common symptoms of this disease are swelling, pain and swelling of the scrotum, as well as redness on the affected side.
Ultrasound of the scrotum
- Cost: 3,000 rub.
More details
Epididymitis also manifests itself:
- the appearance of bloody impurities in the semen;
- temperature rise to 38-39 degrees Celsius;
- discomfort and pain in the groin and lower abdomen;
- pain and burning during ejaculation or during urination;
- discharge from the opening of the urethra;
- increased pain in the scrotum during movement or defecation;
Stages
When a malignant tumor is detected, it is necessary to find out how far the tumor process has spread, that is, to determine the stage of the disease. Further treatment depends on this.
Benign testicular tumors are not staged.
Stages of malignant disease range from I to III. The earliest stage of testicular cancer is stage 0 (or germ cell neoplasia in situ). Stage III of testicular malignancy is distinguished. Depending on the stage of the disease, prognostic signs (level of tumor markers, the presence of secondary tumor changes in organs), according to developed standards, a decision on treatment tactics is made.
Etiology of the disease
The diagnosis of spermatocele can only be made by a doctor. The disease can be congenital or acquired. The first group includes pathologies of intrauterine development. The second is a consequence of the following reasons:
- genital trauma;
- scrotal disease;
- hormonal changes in the body (puberty or androgen pause);
- inflammatory processes of the testicle, vas deferens, seminal vesicles or appendages.
The cause of spermatocele is obstructed fluid outflow and its accumulation in the epididymis. This provokes the formation of a cystic cavity where secretions accumulate. The latter may contain epithelium, seminal plasma, leukocytes, and sperm.
Due to damage to the ducts, the timely evacuation of secretions is impaired, which leads to the accumulation of fluid and the growth of the cyst. In some cases, the formation may have several chambers.
Surgery
The surgical method is the primary step in the treatment of all types of testicular tumors. At the first stage, when a tumor is detected, surgery is performed to remove the testicle (orchidectomy). As a rule, a radical inguinal orchidectomy (surgical removal of the testicle) is performed. The operation is of a therapeutic and diagnostic nature, since in addition to removing the tumor, it allows you to establish a morphological diagnosis (determine the type of tumor), which is necessary to determine further tactics.
Therapy
Treatment of small spermatoceles involves a wait-and-see approach. If the tumor does not bother you and does not increase, you should regularly see a urologist. If the cyst progresses, there is a risk of rupture of the cystic formation or suppuration, the doctor will recommend surgical intervention.
Don't be scared: spermatoclecectomy is a minor operation performed under local anesthesia. Using optical technology, the doctor makes a minimal incision in the scrotum and removes the tumor to the surface. With this intervention, neither the testicular tissue nor the epididymis is damaged.
After removal of an epididymal cyst, it must be submitted for histological examination in order to study its structure and exclude an oncological nature.
It is important to understand that although the intervention is minor, the success of the treatment and the absence of complications depend on the quality of the operation. The Dr.AkNer Urology Center offers qualified assistance in the treatment of spermatocele. We employ experienced specialists and have the most up-to-date medical equipment.
Radical inguinal orchidectomy
Surgery to remove a testicle for cancer is called a radical inguinal orchidectomy. The tumor is removed along with the testicle and spermatic cord.
Orchidectomy may be postponed if the patient is in extremely critical condition (in this case, treatment begins with chemotherapy for life-saving reasons).
Tumor in the testicle
After receiving a histological report on the nature of the tumor, examination data: CT of the chest, abdominal cavity, CT/MRI of the pelvis, the level of tumor markers, staging is carried out, the prognosis is determined, and a team of specialists makes a decision on treatment tactics.
When planning chemotherapy, you should discuss with your doctor the risk of fertility problems and the need for sperm cryopreservation. The procedure must be performed before starting chemotherapy.
Varicocele causes
Varicocele does not cause pain, and only occasionally can be manifested by aching or pulling sensations in the testicle . This is the insidiousness of this disease, because it can be difficult to convince a patient who is not in pain to go under a knife (although today it is, of course, not a knife, but a microsurgical instrument ). But it is necessary to undergo surgery, because due to varicose veins of the spermatic cord, blood stagnation occurs in the testicle , its blood supply suffers and the local temperature rises. All these factors, acting gradually and imperceptibly, lead to disruption of the process of formation and maturation of sperm, and in advanced cases - to a decrease in the size and atrophy of the testicle . The sooner varicocele , the greater the chance of preventing negative consequences for the man’s body.
In patients with varicocele, pathological changes in the spermogram are often detected. The most common are oligozoospermia (a decrease in the concentration of sperm to less than 15 million per ml), asthenozoospermia (a decrease in the concentration of progressively motile sperm to 32% or less), teratozoospermia (a large number of pathological forms of sperm, exceeding 96%). Varicocele is characterized by damage and fragmentation of sperm DNA .
Several studies in recent years have confirmed the relationship between varicocele and decreased testosterone levels and erectile dysfunction . Thus, in 2011, a group of Indian scientists led by Sathya Srini V. published the results of treatment of 200 patients with hypogonadism and erectile dysfunction in combination with varicocele. Some of these patients received hormone replacement therapy, while others underwent surgical treatment of varicocele. In 78% of patients who underwent surgery to eliminate varicocele, normalization of testosterone levels was achieved with improvement in erectile function. Similar results were demonstrated by the Polish urologist D. Paduch. In his study of infertile men with varicocele and hypogonadism, 76% achieved normalization of testosterone and improvement in sexual function after surgical treatment of varicocele.
Chemotherapy
Chemotherapy is one of the main methods of treatment for malignant testicular tumors. These tumors are highly sensitive to chemotherapy, and complete cure is possible even with a large spread of the tumor process. Chemotherapy is not used to treat benign testicular tumors.
Chemotherapy is usually given in cycles of 3 weeks. For malignant testicular tumors, it is very important to strictly observe the intervals between chemotherapy cycles.
The regimen and duration of treatment depend on the stage of the disease, prognosis group, treatment received previously, and the individual characteristics of the patient.
Possible side effects of chemotherapy
Chemotherapy drugs act on rapidly growing cells and dividing tumor cells. But chemotherapy also damages normal tissues in the body, such as cells in the bone marrow (where new blood cells are made), the lining of the mouth, intestines, and hair follicles. The side effects of chemotherapy depend on the type and dose of drugs used and the length of treatment. The most common complications are: decreased blood counts (decrease in the level of leukocytes, neutrophils, hemoglobin, platelets), hair loss, stomatitis (inflammation of the oral mucosa: swelling, redness, plaque, ulcers), nausea and vomiting, weakness, diarrhea, decreased appetite.
Most side effects are short-lived and go away after treatment ends, but some may last a long time, such as hearing loss or kidney or lung damage. Therefore, chemotherapy should be carried out according to absolute indications in accordance with the developed recommendations, and the patient should be under the supervision of an oncologist for a long time.
After chemotherapy and examination, the issue of removing the remaining tumor foci is discussed. One type of surgical treatment is the removal of retroperitoneal lymph nodes (retroperitoneal lymph node dissection).
Depending on the type of tumor and the stage of the disease, lymph nodes around the major blood vessels (aorta and inferior vena cava) may be removed after chemotherapy. Not all patients with a testicular tumor need to have their lymph nodes removed, so it is important to discuss this (and your options) with your doctor. This is a complex and lengthy operation. In most cases, a large incision is made in the middle of the abdomen to allow lymph nodes to be removed. Retroperitoneal lymph node removal should be performed by a surgeon who does it frequently. Experience matters a lot.
How to treat varicocele
Operation Palomo
In this operation, a 5-6 cm long incision is made in the lower lateral part of the abdomen, above the inguinal canal. In this place, the testicular vein is usually a single trunk, running along with the testicular artery and lymphatic vessels. The surgeon isolates, ligates and cuts the vascular bundle as a single block. General or spinal anesthesia is most often used. The disadvantage of the Palomo operation is the intersection of the testicular artery that supplies the corresponding testicle, which can worsen its functional state. The intersection of lymphatic vessels can lead to the formation of hydrocele (hydrocele). Recovery and rehabilitation after Palomo surgery takes about 2 weeks.
Operation Ivanissevich
The length of the incision is approximately the same as during the Palomo operation, but the incision itself is made lower, directly in the area of the inguinal canal. The spermatic cord (containing dilated veins) lies quite superficially in this place, which makes it possible to isolate it. Typically, the operation is performed under general or spinal anesthesia, although local anesthesia is also possible.
During the Ivanissevich operation, the surgeon tries to preserve the testicular artery and lymphatic vessels, but the lack of optical magnification makes this task difficult. In case of ligation of the artery and lymphatic vessels, the complications described above may occur (testicular atrophy, hydrocele formation). The recovery period after Ivanissevich's surgery lasts about 2 weeks .
Operation Marmara
Marmara operation (subinguinal microsurgical ligation of the veins of the spermatic cord). This technique was first described by American urologist Joel Marmar in 1985. Through a small (about 2 cm) skin incision in the groin area (below the inguinal canal), the spermatic cord is isolated. Using optical magnification (operating microscope or binoculars) and microsurgical techniques, the elements of the spermatic cord (vas deferens, testicular artery, tributaries of the internal spermatic vein and lymphatic vessels) are separated. Venous vessels with a diameter of more than 2 mm are ligated (ligated) and divided. All other elements remain intact. The operation ends with the application of a cosmetic suture.
In 1992, another American urologist-andrologist Mark Goldstein modified the Marmara operation, proposing to cross not only the branches of the internal spermatic vein, but also the veins of the scrotum (branches of the external spermatic vein and gubernacular veins), for which it is necessary to remove the testicle into the surgical wound. The Goldstein modification is still actively used by urologists around the world, especially for recurrent forms of varicocele.
The Marmara operation can be performed under general or spinal or local anesthesia. The minimal incision length and microsurgical technique make it possible to perform this operation on an outpatient basis, without hospitalization.
In most cases, the patient can leave the clinic within 1-2 hours after surgery. Complications during the Marmara operation are much less common than with other types of operations used for varicocele. The functional and cosmetic results of Marmara surgery are also significantly better than other techniques. The number and motility of sperm increases to a greater extent. It is natural that the Marmara operation is currently considered as the “gold standard” for the surgical treatment of varicocele.
Scrotal access
Varicose testicular veins can also be divided at the level of the scrotum. Through a small incision of about 1-2 cm, the spermatic cord is isolated, followed by the intersection of varicose veins. The main stages of the operation correspond to the Marmara technique . The main difficulty with scrotal access is that the internal spermatic vein at the level of the scrotum is represented by a network of veins of different sizes, forming a pampiniform (or pampiniform) venous plexus. To achieve a good effect, it is necessary to cross each of these branches, which, of course, increases the operation time. The scrotal approach is currently rarely used for the treatment of varicocele.
Laparoscopic ligation of the testicular vein
Like any other laparoscopic surgery, ligation of the testicular vein is performed through punctures in the anterior abdominal wall. The operation is performed only under general anesthesia. Instruments and an optical system are introduced through punctures into the abdominal cavity. The testicular vein is isolated near the internal opening of the inguinal canal, metal clips are applied to it, and the vein is divided. The functional results of laparoscopic surgery for varicocele are generally close to the results of the Ivanissevich operation.
The postoperative period is easier than during the operations of Palomo and Ivanissevich , punctures in the abdomen heal quite quickly. Typically, the patient is discharged home the next day after laparoscopic ligation. The only advantage of laparoscopic surgery for varicocele, in my opinion, is the ability to cross the testicular veins on both sides (for bilateral varicocele) through the same access. The disadvantages of the laparoscopic approach are the need for general anesthesia, as well as the risk of complications associated with the introduction of instruments into the abdominal cavity.
Testicular vein embolization for varicocele
This technique is the least invasive among all those used to treat varicocele . The absence of an incision allows embolization to be performed under local anesthesia (or without anesthesia at all!). Naturally, there is no need for seams. A thin catheter with a flexible guide is inserted through a needle into the femoral vein. Contrast is injected through the catheter into the vasculature, and the location and movement of the guidewire and catheter are monitored using fluoroscopy. The catheter is passed retrogradely (from the renal vein towards the testicle) into the internal spermatic (testicular) vein. The structure and features of the testicular vein are assessed, and possible additional branches and tributaries are identified. After this, a coiled spiral is inserted through the catheter into the lumen of the vein. In the lumen of the vein, the spiral expands, firmly pressing against the walls of the vein and fixing itself inside. Then an embolic substance is injected into the lumen of the vein, completely closing the lumen of the vein. A control study of blood flow through the vein is performed. If there is no blood flow, the operation is completed.
The patient can leave the clinic within two hours after the operation . Recurrence of varicocele after embolization is very rare. Another advantage of embolization for varicocele is that during the procedure, fluoroscopy of the veins is performed, which makes it possible to diagnose various anatomical anomalies, additional branches connecting the testicular vein with the vein of the same name on the opposite side, and other vascular features leading to relapses of varicocele. In this regard, embolization may be particularly effective in cases of recurrent varicocele. Like any method, testicular vein embolization is not without its drawbacks.
One of the significant ones is the need to administer a contrast agent (usually the same as is administered during computed tomography). Some people have an allergic reaction to contrast and cannot undergo embolization. In addition, the administration of contrast is contraindicated in renal failure. Therefore, before this operation, the blood creatinine level must be checked.
Another limitation for embolization is right-sided varicocele. Right-sided localization is uncommon with varicocele. But, due to anatomical features, inserting a catheter and guide into the right testicular vein is often very difficult. Therefore, for right-sided (or bilateral) varicocele, it is better to resort to surgical treatment methods rather than embolization.
The high cost and relatively low availability of embolization are also of particular importance. The cost of embolization for varicocele, as a rule, is several times higher than the cost of surgical treatment (including the Marmara operation). This is due to the use of expensive disposable consumables and the need to work in an endovascular operating room equipped with high-resolution fluoroscopic equipment (angiograph). Embolization is a highly operator-dependent technique, the effectiveness and safety of which largely depends on the surgeon (human factors).
Complications from testicular vein embolization are rare . These include an allergic reaction to contrast, impaired renal function, bleeding from the puncture site, and perforation of the vein wall. A rare specific complication is migration (displacement) of the installed coil and its movement along the vascular bed with the occurrence of embolism in various organs.
Comparison of different operations for the treatment of varicocele :
| Cut length | Anesthesia | Rehabilitation period | Relapse rate | |
| Operation Palomo | 5-6 cm | spinal | 2 weeks | 29 % |
| Operation Ivanissevich | 5-6 cm | spinal | 2 weeks | 13,3 % |
| Operation Marmara | 2 cm | local/general | 7-10 days | up to 4% |
| Laparoscopy | 3 punctures | anesthesia | 5-7 days | 3-7 % |
| Embolization | No incision | local | 1 day | to 10 % |
, in accordance with the recommendations of the European Association of Urology , I perform on my patients the most modern operation for varicocele - microsurgical subinguinal ligation of varicose veins according to Marmar, and I have extensive experience in this operation.
Treatment of varicocele without surgery
Many of my patients, who are faced with such a problem as varicocele for the first time, are primarily interested in whether it is possible to treat varicocele without surgery. Of course, it would be very tempting to do without surgery, or even better to cure varicocele with folk remedies. Unfortunately, I have to disappoint them. There are currently no effective methods for treating varicocele without surgery. A temporary positive effect can be provided by some herbal remedies that increase the tone of the veins (horse chestnut tincture, grape leaves), as well as medications (for example, Aescusan, Detralex, Phlebodia, etc.). Varicoceles, of course, will not go away with these medications, but the symptoms may decrease. To reduce the symptoms of varicocele, adherents of traditional medicine recommend limiting physical activity and wearing tight-fitting underwear (so that the scrotum does not sag, but is pressed against the perineum). Temporary relief can be expected from these measures, but the varicocele itself will not disappear. Therefore, I must state that attempts to cure varicocele without surgery only waste precious time.
Treatment of varicocele - operations
As I already mentioned, conservative methods of treating varicocele are ineffective.
Consequences of lymph node dissection
Removal of retroperitoneal lymph nodes is a major operation. It does not cause impotence, and men retain erectile function. But during this operation, some of the nerves that control ejaculation may be damaged. If these nerves are damaged, then when a man ejaculates, the sperm does not exit through the urethra, but goes back into the bladder. This is called retrograde ejaculation, and this complication can make fatherhood difficult.
In case of a widespread process (when there are metastases in other organs), in order to obtain the best result and reduce the risk of the disease returning, various types of operations can be performed to remove all tumor foci. If the remaining tumor foci are not removed or are not completely removed, the risk of the disease returning increases several times.
More often the operation is successful when it is performed by experienced doctors.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Appointment with a surgical doctor (primary, for complex programs) | 3 000 |
| Ultrasound of the scrotum | 3 000 |
| Duplex scanning of scrotal vessels | 3 500 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Fertility
Malignant testicular tumors most often occur in men of reproductive, young age, when they start a family and children. During chemotherapy there is a high risk of impaired fertility, so it is necessary to discuss the need for sperm cryopreservation with your doctor before starting treatment. Sperm cryopreservation is a method of storing ejaculate, which involves freezing it (most often in liquid nitrogen), followed by restoration of sperm function after thawing. Cryopreservation should be performed before starting chemotherapy.
Examination before cryopreservation:
- spermogram (method for examining ejaculate to assess fertilizing ability);
- sperm cryotest (carried out to find out whether the quality of sperm decreases after thawing);
- blood test for infections: syphilis, HIV 1.2 (IgG and IgM), hepatitis B and C;
- urethral smear for genital infections.
After undergoing the examination, sperm is collected by masturbation. Within a few minutes after this, the biomaterial enters the embryology laboratory. Manipulations are carried out to cleanse and concentrate sperm, special substances are added to protect sperm, and the sperm is placed in special thin containers. Your container is labeled (individual data is noted) and then stored at very low temperatures.
Treatment of testicular cysts in men
Treatment of testicular cysts in men is carried out in cases where the cystic formation increases to a size at which discomfort and symptoms of the disease appear. Conservative treatment of testicular cysts in men is ineffective. Urologists first perform a puncture of the cyst, followed by suction of fluid from the cystic cavity. The resulting contents are sent to a cytology laboratory for examination under a microscope.
Sclerotherapy is a procedure for enucleating a cyst with the introduction of a chemical substance into the cavity that “glues” the walls of the cavity. This method of treating testicular cysts in men can be complicated by impaired patency of the spermatic cord, which subsequently leads to infertility. Therefore, urologists at the Yusupov Hospital offer this method of treatment to patients who do not plan to have children in the future.
Observation
All patients with a malignant testicular tumor should be carefully observed for a long time - up to 10-15 years after initial treatment, since, despite the treatment, there remains a risk of developing a relapse of the disease. The risk of tumor recurrence is highest within two years after initial treatment.
Follow-up includes medical history, examination, tumor markers, ultrasound of the scrotum with elastography, inguinoiliac areas, abdomen and retroperitoneum, and chest x-ray. The observation schedule depends on the stage of the disease. If relapse is detected, treatment options include chemotherapy and surgery.
In addition, the reasons for the development of epididymitis can be:
- complications after infectious mumps (so-called mumps);
- hypothermia;
- constant difficulty urinating;
- complications of tuberculosis.
Indications
Surgical treatment is indicated in the following cases:
- Abscess of the epididymis or testicle.
- Accumulation of pus.
- Lack of results from antibiotic treatment.
- Acute form of the disease.
- Infertility due to obstruction of the appendage.
Contraindications
It is not recommended to perform surgery in case of exacerbation of chronic diseases and allergic reactions to medications and painkillers.
Forecast
Advances in the treatment of testicular cancer are among the greatest achievements of modern medicine. Today, cure is achievable in 95% of all patients with testicular tumors, and in 80% of patients with the advanced form of the disease. Despite this, the metastatic form of the tumor remains incurable in approximately 10% of patients. The prognosis depends on the histological type of testicular cancer, the extent of the tumor process, and the treatment performed. In some regions of the Russian Federation, the survival rate of patients with testicular tumors reaches only 60%. This is due to various reasons (rarity of the tumor, late presentation of patients, low awareness of doctors).
National Medical Research Center of Oncology named after. N.N. Petrova is a specialized center for the treatment of testicular tumors with many years of experience in the treatment of this group of oncological diseases. Our Center employs a team of highly qualified professionals - oncologists, including surgeons (urologists, thoracic and abdominal surgeons), specialists in drug therapy for adults and children (chemotherapists, oncopediatricians), radiation diagnostics, morphologists, anesthesiologists, resuscitators, radiologists. The management of each patient with a testicular tumor is discussed repeatedly by a multidisciplinary team.
If you or a loved one develops symptoms that suggest a testicular tumor, you should consult a doctor immediately. Considering the high percentage of complete cure for this group of diseases and the high effectiveness of drug therapy, in our Center you can quickly receive all the necessary help from specialists who have extensive experience in treating this pathology.
List of used literature:
- Practical recommendations of the Ministry of Health of the Russian Federation: “Germ cell tumors in men”, 2022.
- Garner MJ, Turner MC, Ghadirian P., Krewski D. Epidemiology of testicular cancer: an overview. Int J Cancer 2005;116:331–9.
- Ferlay J., Colombet M., Soerjomataram I. et al. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2022. Eur J Cancer 2018;103:356–87.
- WHO classification of tumors of the urinary system and male genital organs. Ed. by H. Moch et al. Lyon: IARC, 2016.
- Tryakin A.A., Gladkov O.A., Matveev V.B., et al. Practical recommendations for drug treatment of germ cell tumors in men //. Malignant tumors: Practical recommendations RUSSCO, 2022.
- Gilligan T., Lin DW, Aggarwal R., et al. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Testicular Cancer. Version 1.2020 — November 5, 2022.