06/07/2018 I’ll start today’s article with what has already become a classic situation.
A person comes to see a doctor (dermatologist or oncologist) and shows him his moles.
And then something like this happens:
– You have dysplastic nevi here, here and here.
- What is this? Is it dangerous?!
– Dysplastic nevi are moles with an uneven edge and uneven color. Dysplastic nevi can develop into melanoma and must be removed.
- Oh!!! How scary!!! Let's delete it quickly!!!
The moles are safely removed and sent for histology.
A person comes home and starts reading on the Internet about dysplastic nevi. And then they add fuel to the fire:
- A dysplastic nevus is any nevus with an uneven edge and uneven coloration.
- All dysplastic nevi turn into melanoma in 146% of cases.
- To prevent death from melanoma, you need!!! URGENTLY!!! remove all dysplastic nevi.
All this “beauty” has been copied from one site to another for many years and fills the domestic segment of the Internet to the brim.
Let's understand all this from the point of view of evidence-based medicine.
Linear nevi - symptoms
Linear epidermal nevus was first described by Baerensprung in 1863 as naevus unius lateralis. These are congenital changes, most often present at birth, but sometimes they may not appear until childhood.
At the first stage of the disease, they look like limited areas of excessive pigmentation that do not protrude above the surface of the skin, smooth spots or papules that match the color of the skin. Later in the disease they take on a papillary form. The discoloration is associated with mild hyperkeratosis.
Epidermal moles can be found on any area of the skin, including the anus and urogenital areas. They are often located on the face and neck, scalp, trunk or limbs. The most common changes are linear and unilateral, along Blaschko's line, not extending beyond the midline of the body.
They can be:
- single, clinically resembling seborrheic keratosis;
- multiple warts, sometimes generalized, affecting large areas of the skin and persisting throughout life.
Sometimes they have a linear, vortex, striped system, often generalized, covering large areas of the body.
Moles appear in early childhood, grow with the patient and do not regress. Sometimes they can flare up and disappear, especially in the case of inflammatory linear papillary epidermal nevus, which can be accompanied by pain, burning and erosions, but never completely goes away.
Cases of the development of a malignant neoplasm in an epidermal nevus are rare, but not excluded. Isolated cases of development at the site of the lesion have been described:
- keratoacanthomas;
- basal cell carcinoma;
- squamous cell carcinoma.
Such moles may be associated with other developmental defects of the central nervous system, skeletal system, vision, as well as with some developmental disorders, for example, Proteus syndrome, McCune-Albright syndrome, Klippel-Trenaune syndrome.
Out of sight, out of sight. How to get rid of moles
Not an easy question. Many factors influence the ability to remove tumors. Unfortunately, no pills have yet been invented that will relieve you of annoying or dangerous moles.
Yes, treatment of small nevi usually does not cause problems.
Successful removal depends on:
- Doctor's qualifications
- Mole size
- Nevus locations
The first option is surgery. The doctor cuts off the mole, some adjacent skin, and then stitches the wound. After removal, the nevus heals quite quickly, but a noticeable mark remains.
Whether this is good is up to you to decide.
What about laser surgery?
Yes, modern technologies do offer new treatments, but they do not work miracles, as some people believe. Some skin diseases are treated with lasers. But not all nevi.
The laser beam vaporizes the outer layer of skin and cells of the mole. The deeper it is rooted, the more difficult it is to destroy it completely - sometimes the surface layer is burned out, but the base remains intact. Then the nevus grows back.
The operation has to be repeated again and again, and there is no guarantee of results. So the surgical procedure is sometimes more reliable than laser surgery.
However, in some situations, a high-tech procedure accomplishes the task. Removes small nevi. Working with large tumors is much more difficult.
We recommend choosing laser nevus removal only after consulting a dermatologist and checking the tumor.
Another important point is the choice of doctor. Many doctors have accumulated vast experience in removing small moles. Everyone has them. Therefore, doctors work with them very often and know well how to quickly remove nevi.
But what about large moles?
They are not common and therefore it is difficult to find a doctor who regularly operates on them. Read reviews about nevus removal on the websites of different clinics. This is useful. You will learn what operations the doctors of these medical institutions performed and the patients’ impressions of their work.
Gather more information.
When you see your dermatologist, ask about available methods for removing moles. Perhaps in your case, surgery and laser therapy are not the best options. Harmless nevi do not need to be removed at all.
Many medical institutions remove moles. But where to go? We would like to recommend one of these clinics.
Diagnosis - histopathological features of linear nevi
There is considerable variability in histopathological studies. The most common manifestations:
- hyperkeratosis;
- acanthosis;
- papillomatosis.
Some moles may exhibit acantholysis and dyskeratosis, resembling Darier's disease.
Sometimes you can find a picture of epidermolysis with hyperkeratosis, reminiscent of congenital bullous erythroderma ichthyosis. In these cases, mutations in the keratin 1 or 10 genes are found.
Diagnosis of nevus
Types of epidermal nevi
There are several clinical types of epidermal nevi. This classification is not definitive, since epidermal moles can be hard, linear and inflamed at the same time.
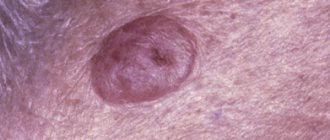
Soft papillary nevus of the epidermis . This is most often a small flesh-colored or gray formation with a soft, velvety surface. Individual papules forming clusters resemble senile warts.
Hard papillary nevus.
Unilateral, segmented, most often located on the trunk and limbs. These are tall or flat, raised discolorations of normal skin, light or dark brown, with a papillary surface.
Inflammatory linear verrucous epidermal nevus.
This is a special form of epidermal nevus with inflammation and severe itching. ILVEN may worsen and disappear, especially in the form of psoriasis-like psoriasis.
According to the conclusions of the study. Altman and Mehregan, diagnostic criteria for such moles include a number of features:
- early onset is noted - in 75% of cases before 5 years,
- more common in females (4 times more often);
- frequent localization on the left lower limb and buttocks;
- itching is usually present;
- histopathological appearance resembling psoriasis - a characteristic pattern of parakeratotic areas with visible psoriasis-like epidermal hyperplasia, mild spongy edema and exocytosis of lymphocytes;
- Such nevi have no tendency to spontaneous regression and resistance to treatment.
The lesions are linear, pruritic, erythematous lesions with a flaking surface and may resemble psoriasis lesions with a linear pattern. They are distinguished from psoriasis by the absence of Munroe microcirculation and the lack of epidermal involucrin expression in ILVEN. The connection with psoriasis is confirmed by the participation of the cytokines IL-6, IL-1, TNF-alpha, ICAM-1 in the pathogenesis.
Horny nevus (nevus corniculatus)
. This is the rarest form of epidermal nevus. The clinical picture shows very intense keratosis with the formation of thick papillary growths and filamentous formations. Histopathological examination shows foci of acantholysis with depressions in the epidermis filled with dense keratin.
Pediatric epidermal nevus.
This variety is characterized by congenital hemidysplasia, unilateral ichthyosis and limb defects. All of these disorders can occur, but it can only be the cutaneous form. The lesions are located unilaterally and do not extend beyond the midline of the body, with the most common lesions being the flexor folds. They have the character of erythematous lesions covered with yellow hyperkeratotic scales and sometimes with horny plugs. This type of mole occurs only in women because the gene responsible for the condition is located on the X chromosome.
Epidermal nevus syndrome, which is a combination of epidermal nevus with other developmental defects, has been clinically identified.
There are 4 clinical variants of the syndrome (Michalovsky classification):
- four-symptom form - lesions of the skin, bones, nerves and eyes.
- three-symptomatic form - skin, bone and nervous changes.
- two-symptomatic form - skin and bone changes.
- monosymptomatic form - the presence of a linear papillary epidermal nevus.
Differential diagnosis
To make an accurate diagnosis, a dermatologist must conduct a series of tests, since the symptoms of linear moles are similar to those of other skin diseases.
At issue are:
- warty neurodermatitis
- characterized by lycosis and itching; - lichen planus papillary
- characterized by itching and its occurrence at a later age, determined by the presence of typical lesions of lichen planus in other places and histological examination; - lichen striata - characterized by inflammatory papular rashes and spontaneous resolution within a few months.
Risk factors
The transformation of a nevus into a malignant form depends on intrauterine mutations and developmental characteristics. External factors, including nutrition, physical activity, and working conditions can only speed up or slow down the process.
Dermatologists identify the main risk factors for the transformation of moles into malignant ones:
- an abundance of large formations from infancy;
- sudden appearance of moles in old age;
- the presence of giant nevi;
- location in places of friction with clothing;
- injuries on moles.
When degenerated, the nevus grows rapidly, which is accompanied by painful sensations. The texture and color of the formation quickly change, and the skin may begin to peel and bleed.
Treatment of epidermal moles
Epidermal moles persist throughout life, do not tend to disappear spontaneously and are primarily a cosmetic problem, especially on the skin of the face and neck. These are benign formations, although there are risks of developing cancer. A case of squamous cell carcinoma inside a nevus has been described in the literature. Treatment of epidermal moles is necessary for cosmetic reasons.
Treatment uses many different methods, varying in effectiveness and availability. When treating epidermal nevi, the following is used:
- surgical removal of the lesion;
- electrocoagulation;
- cryotherapy;
- dermabrasion;
- CO 2 laser;
- dye laser;
- tretinoin;
- 5-fluorouracil;
- acitretin;
- calcipotriol;
- dithranol;
- podophyllin;
- keratolytic drugs.
Conservative methods fail to achieve complete recovery, and scars remain after surgical removal of the lesion. The mechanism of action of individual methods is not always fully understood. For example, calcipotriol can affect the production and function of cytokines and normalize the differentiation of epidermal cells, 5-fluorouracil has an antiproliferative effect.
Some of the treatments that were used in the past are now only of historical significance.
According to many scientists, the most effective method of treating linear lesions in a small area is to remove the nevus by surgical excision; however, when completely removing large lesions, it is necessary to cover the defect with a free skin graft, which is often associated with the formation of an unaesthetic scar.
The effect of laser on moles
Introduction
Every child has melanocytic nevi; they can be single, multiple, exist at birth (congenital) or appear over time (acquired).
The tactics for managing patients with melanocytic formations in childhood can be implemented in three ways: surgical excision of the element, dynamic observation of the formation, and zero-intervention tactics, when further observation or surgical intervention is not required. The doctor makes a decision based on an analysis of all factors characterizing the nevus: the child’s age, morphology, location, size and melanoma danger of the element.
The predominance of aggressive surgical tactics in relation to nevi in children forced us to turn to scientific literature data reflecting the state of this problem in the world.
The purpose of the work is to analyze literature data over the past 10 years on the pathogenesis, clinical picture, diagnosis and management tactics of congenital and acquired nevi in children.
Laser removal of warts
The use of lasers gives promising results. Various types of lasers have been used to treat moles, including: CO 2 lasers, dye laser. Landthalter et al. Dermatologists have successfully used argon laser in patients with localized papillary epidermal nevus. Also, very good results are achieved using the argon laser in most patients with superficial nevus, while satisfactory results have not been obtained in patients with papillary nevus.
Another method of laser treatment of warts is the removal of epidermal nevus with a pulsed Er: YAG laser operating at a wavelength of 2940 nm and having the properties of high absorption of water contained in the tissue, as well as CO 2 laser removal.
The pulse energy is aimed at ablation, and the area of thermal damage is small, which minimizes the possibility of scarring and guarantees a relatively rapid healing process. This type of laser can remove superficial changes with very good cosmetic results.
In the case of large papillary moles of the epidermis, the best method is CO2 laser treatment.
Uch. Michel et al have used the CO 2 laser in the treatment of papillary epidermal moles with good cosmetic results when the appropriate specifications are met. The small lesions have completely disappeared, leaving only a discolored scar. Relapses were observed with too gentle procedures.
Based on these results, scientists claim that CO 2 laser treatment is more effective than other lasers, but at the same time has a higher risk of scarring. Laser treatment is a relatively new, but very promising method of treating papillary nevi of the epidermis.
Sources
- Du Vivier A.: Atlas of Clinical Dermatology, 2002.
- Gur E, Zucker R: Complex facial nevi: a surgical algorithm, 2000.
- Rosen T: Keratoacanthomas arising within a linear epidermal nevus. J. Dermatol. 1982.
- Mikhalovsky R.: Dermatological syndromatology, 1984.
- Goldberg HS: Basal cell epitheliomas developing in a localized epidermal nevus. 1980.
- Ichikawa T. et al.: Squamous cell carcinoma arising in a verrucous epidermal nevus, Dermatology, 1996.
- Molin L, Sarhammar G: Perivulvar inflammatory linear verrucous epidermal nevus treated with CO2 laser, 1999.
- Michel JL et al: CO 2 laser dermabrasion in the treatment of linear papillary epidermal nevi, Dermatologica, 2001.
- Pavlacik M. et al.: Epidermal nevus syndrome - a two-symptomatic form, 1996.
- Zvulunov A. et al.: Calcipotriol for topical use for the treatment of inflammatory linear verrucous epidermal nevi: 1997.
- Pearson IC, Parland CC: Treatment of epidermal nevi with pulsed erbium laser, 2005.
- Boyce S, Alster TS: CO 2 laser treatment of epidermal nevi long-term success. 2002.
Causes
The appearance of moles in infants can be influenced by two main factors.
Hereditary predisposition
If a newborn has birthmarks or moles in the same places as the parents, then this fact only proves that the nevus is inherited. Such neoplasms also include a variety of Mongolian spots.
Frequent stress during pregnancy
According to some experts, frequent changes in blood pressure can negatively affect the condition of blood vessels, resulting in disruption of placental blood circulation. The accumulated vessels may later appear as a red vascular mole.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
In addition, doctors identify several other reasons that can trigger the appearance of a nevus in the first months of a child’s life. These include:
- prolonged exposure to direct sunlight ;
- hormonal changes .
According to statistical data, nevus is more often formed in premature infants, in children with a light skin tone, as well as in girls (in boys, the formation of neoplasms is diagnosed much less frequently).