A pigmented nevus (birthmark) is a benign skin neoplasm that occurs as a result of disruption of the normal structure of melanocytes—pigment cells containing melanin. They originate from the neural fold and, during embryogenesis, move to the basal (germ) layer of the skin of various parts of the human body. When the normal maturation or migration of these cells is disrupted, a congenital form of nevus occurs. Such deformed melanocytes (nevocytes) do not have processes, are characterized by poor metabolism and are capable of excessive pigmentation of the skin.
Moles, or pigmented nevi, occur in 90% of people
Melanoform nevus was assigned an ICD 10 code – D 22.
General information
Melanoma (other designations used are melanoblastoma , melanosarcoma ) is a malignant disease, one of the types of skin cancer, which is formed as a result of mutational changes in cells that accumulate the pigment melanin .
This formation develops, as a rule, in open areas of the skin - on the skin of the extremities, back, etc., less often on the mucous membrane (oral cavity, rectum, vagina), and the retina of the eye. The ICD-10 code is C43 (malignant melanoma of the skin). Melanoblastoma is an aggressive formation that metastasizes . Experts note that this tumor can demonstrate a very wide variety of clinical courses. According to statistics, 89% of patients with this disease die in the first years after diagnosis. A favorable prognosis is observed only at the first stage of the disease. However, the outcome and prognosis of the disease largely depends on the condition of the patient’s body and the characteristics of the tumor. A pre-melanoma condition can be Dubreuil melanosis, as well as a number of other diseases - melanosis of the colon, sclera, etc.
The human melanoma gene was discovered in 1965 by US doctor R. Tuckington. But there are still many points regarding this disease that require further research.
Speaking about what skin melanoma is, it should be noted that this is a very serious disease that progresses rapidly. As evidenced by Wikipedia and other sources, how quickly this malignant process develops depends on a number of factors. This article will discuss how to recognize the symptoms of this terrible disease and what methods of treatment are currently practiced.
Short description
Nevi (moles, birthmarks) are hamartoma-like malformations of the skin that can develop both from elements of the epidermis and the dermis itself (connective tissue, vascular elements or melanocytes). Nevi are pigmented formations that usually protrude above the surface of the skin. Almost every person has moles; they can be congenital or occur throughout life, especially during puberty, in women during pregnancy, and hormonal dysfunctions. The clinical picture is characterized by extreme diversity in the number, size, morphological type and degree of pigmentation of individual elements - spots, nodules, plaques - up to subtotal damage to the skin with the so-called giant nevi. Large congenital nevi are considered to be elements >20 cm or occupying 2.5% of the body surface; they are considered a risk factor for malignancy.
Code according to the international classification of diseases ICD-10:
- D22 Melanoform nevus
- I78.1 Non-tumor nevus
- Q82.5 Congenital non-neoplastic nevus
• Epidermal nevi (warty or mole-like) are most often found at birth, although they can also develop in childhood (very rarely in adults). Externally they may be similar to papillomas (viral origin), but are usually represented by large linear plaques or an array of small papules. Epidermal nevi are often asymptomatic. Malignization is rare, with the exception of nevi of the sebaceous glands (basal cell carcinoma occurs in 5% of cases). Histologically they are characterized by acanthosis and hyperkeratosis. Nevus of the sebaceous glands is also characterized by the presence of a large number of sebaceous and apocrine glands. Cellular atypia is not observed. Treatment is mainly for cosmetic purposes. Preventive removal of sebaceous gland nevus is performed due to clinical manifestations (hair does not grow on it), and not the danger of malignancy.
• Dermal nevi •• Connective tissue nevi are predominantly congenital and are often represented by dense, single papules and flesh-colored plaques. The number of hair follicles in them can be significant (“pigskin”). This variant of nevi is idiopathic and is not associated with other diseases, with the exception of “shagreen skin” in tuberous sclerosis. Histologically, they consist of dense conglomerates of collagen and elastic fibers. Prognostically safe and removed solely for cosmetic reasons •• Vascular nevi (hemangiomas) are vascular formations lined with endothelium, mainly capillary, but cavernous structures can also occur, especially in large nevi. Three clinical types are considered typical: strawberry nevus, cherry nevus and cavernous hemangioma. Strawberry nevus and cavernous hemangiomas more often undergo spontaneous regression, while cherry nevus continues to grow throughout life. Surgical treatment is carried out for cosmetic reasons, for functional disorders (localized in the conjunctival area, lips) or thrombosis of the cherry nevus (due to suspicion of malignancy) •• Melanocytic nevi are of the greatest clinical importance, given the need for differential diagnosis with melanoma •• Pathohistology. Nevus cells are located in the form of nested clusters of various sizes and configurations in the dermis, subepidermally and between cell complexes. Sometimes the accumulations become diffuse and are located very close to the epidermis along the basement membrane, and atrophic changes in the epidermis are noted. The cells are large, of various shapes and sizes, with a clearly visible nucleus, sometimes several hyperchromatic nuclei, arranged in the form of “rosettes” or lumpy clusters. In some elements, the shape of the cells is spindle-shaped, which makes the nevus resemble a neurofibroma. Pigment content may vary. In “young” nevi, the stromal component is weakly expressed; over time, the connective tissue stroma begins to predominate; such a nevus is considered “fibroepithelial.” Localization of nevus cells among basal keratinocytes and in the zone of the basement membrane without its disruption is characteristic of a border nevus, and in combination with the intradermal component - of a mixed nevus.
Clinical types of nevi • Basal cell nevus - a hereditary disease (109400, 601309, BCNS gene, 9q22.3, Â) - characterized by (usually benign) skin lesions of the eyelids, nose, cheeks, neck, upper jaw, looks like a flesh-colored papule, without signs erosion, histologically does not differ from basal cell carcinoma. • Verrucous nevus is a skin-colored (or darker) lesion of the epidermis similar to a wart, often linear, appearing at birth or in early childhood; can be of different sizes and localization, single or multiple “verrucous nevus. • Hairy nevus is a mole covered with a large amount of growing hair. • Giant pigmented nevus is a large congenital, with pronounced hair growth, pigmented nevus with a predominant localization on the lower extremities “pigmented hair nevus” .
• A blue nevus is a wide-based papule or plaque of varying shades of gray-blue color. Histologically, clusters of process melanocytes with a high pigment content are found in the dermis, located parallel to the epidermis, which determines the optical effect of blueness when incident rays of the visible spectrum “Jadassohn-Tische nevus”. • Intradermal nevus - a nevus with localization of nests of melanocytes in the dermis, and not at the border between the epidermis and dermis. • Ito nevus - pigmentation of the skin area innervated by the lateral branches of the supraclavicular nerve and the lateral cutaneous nerve of the shoulder; nevus cells lying randomly in the dermis.
• Strawberry nevus is a small vascular nevus similar in size, shape and color to a strawberry - a bright red solitary formation of spongy density. It is observed in 3% of newborns and often spontaneously obliterates by 6–7 years of age. « cavernous hemangioma « cavernoma « cavernous hemangioma. • Unilateral nevus is a congenital linear nevus, which is located along the nerve either on one side of the body or on part of a limb also on one side linear nevus. • Ota nevus (oculodermal melanosis) - skin pigmentation in the area of innervation of the trigeminal nerve and conjunctiva of the eye in the form of bluish-gray spots; occurs in Asia, more often in women. The treatment is cosmetic. • Nevus is dark blue orbital-maxillary .
• Borderline nevus - a nevus consisting of nests of nevus cells near the basal layer, the border of the epidermis and dermis, appears as a small, slightly raised, flat, non-hairy, pigmented (dark brown or black) tumor epidermis - dermal nevus. • Acquired nevus is a melanocytic nevus that is not detected at first after birth, but appears in childhood or in adults. • Flaming nevus ( port wine stain) is a large, vascularized nevus with a purple coloration, usually located on the head and neck. Unlike other vascular nevi, in this case there is no proliferation of a large number of vascular elements, but an expansion of the normal number of skin vessels. As the size of the vessels progresses, protrusion appears and the color of the nevus changes from pink to purple-red. See also Sturge-Weber syndrome in the appendix to this article. • Sebaceous nevus (Jadassohn) - congenital hyperplasia of the sebaceous glands with papillary acanthosis of the epidermis. • With thick curly hair, nevi are congenital foci of growth of spirally twisted hair in the scalp “limited [symmetrical] allotrichia.
• Atypical nevus syndrome (ICD-10: D22 Melanoform nevus; *155600, #155601 [mutation of the CDKN2A cyclin-dependent kinase inhibitor 2A gene, OMIM 600160.0001]) is an inherited disease (Â)) of pronounced familial nature. Prevalence: in the USA up to 5% of the general population; in the late 90s, about 40 thousand familial cases and 4.6 million sporadic forms were registered. Synonym: dysplastic melanocytic nevus •• Clinical picture. Usually spotted elements, but there are papular, plaque-like elements with a central papule or micropapules, oval or irregular in shape, sometimes with processes, 5 mm in size or more, with a finely scalloped clear outline, of varying intensity of brown color (up to black), with an erythematous rim along the periphery •• Pathohistology. There are no generally accepted criteria for diagnosing dysplastic nevus. The architecture of a dysplastic nevus suggests uneven hyperplasia of the epidermal processes with hypertrophy of the terminal sections. Melanocyte cells of adjacent processes are often connected. Among epidermal melanocytes, a spectrum of cytological changes is observed: from moderate pleomorphism to obvious atypia. The pronounced degree of the latter can be interpreted as melanoma in situ. • Red-blue vesicular nevus syndrome (*112200, Â)). Blister-like hemangiomas of the skin, especially the trunk and upper extremities, night pain, regional hyperhidrosis, bleeding gastrointestinal hemangiomas, angiomatous gigantism, cerebellar medulloblastoma.
• Mucosal spongy white nevus is a congenital keratosis of the mucous membranes, manifested by a thickened white spongy fold of the oral mucosa. • Vascular nevus is a congenital uneven red coloration of the skin due to the proliferation of skin capillaries “vascular nevus” hemangioma. • Spitz nevus is a benign juvenile melanoma (see below Juvenile nevus). • Elastic Levandowski nevus - clusters of smooth or bumpy papules of ivory or flesh color, found symmetrically on the trunk and limbs “collagenous nevus”.
• Juvenile nevus •• Spindle cell and/or epithelioid cell nevus (juvenile melanoma, benign juvenile melanoma, Spitz nevus) is a benign melanocytic nevus, usually acquired, having a characteristic histological structure different from other types of melanocytic nevi. Initially it was believed that it occurs mainly in children, but it has now been shown that juvenile nevus is more common (up to 60%) in adults •• Clinical picture. Usually the exophytic formation is hemispherical, less often flat; dense elastic consistency, with clear boundaries; color - from light red to dark brown, sometimes black; the surface is smooth or papillomatous •• Pathohistology. According to its architectonics, a nevus can be borderline, mixed (most often), intradermal. According to the cellular composition, it can be spindle-shaped, epithelioid cellular, and more often mixed. The pigment content in melanocytes is variable. Characteristic is the presence of eosinophilic accumulations - fragments of the basement membrane (the so-called Camino bodies). Spindle-shaped melanocytes are elongated with an elongated nucleus and a large eosinophilic nucleolus. In the epidermis, melanocytes have long cytoplasmic processes and form large elliptical nests, the long axis of which is usually perpendicular to the skin surface. In the dermis, spindle cells are often located parallel to each other in the form of bundles or cords. Polygonal or round epithelioid cells with abundant fine-grained, reticulate or vacuolated cytoplasm. Giant multinucleated cells are often found.
Pathogenesis
The pathogenesis of melanoma is a very complex process, characterized by significant metabolic and molecular abnormalities. Many aspects of pathogenesis still remain unclear to scientists.
Melanoma develops from melanocytes, pigment cells that produce melanin. In order for a tumor to appear and begin to develop, a certain effect on normal tissues or cells is necessary. Their damage provokes proliferative reactions. necrosis of cells or tissues occurs But if proliferation is delayed under the influence of certain carcinogenic factors, cell differentiation may be disrupted, as a result of which the change in the membrane antigenic structure is disrupted and hyporesponsiveness to the influences of regulatory factors of the body is noted.
As a result of these processes, undifferentiated proliferating cells can escape the body's control.
Speaking about the pathogenesis of melanoma, scientists do not exclude that changes in the DNA of the cell with disruption of its protein structure and differentiation in the future may occur due to primary damage.
More than half of primary skin melanomas develop against the background of previous pigmented nevi . Therefore, such nevi are regarded as optional precancer. The most important exogenous factors influencing the development of this tumor are trauma to nevi and UV radiation. The mechanism for the harmful effects of UV radiation may be the formation of highly active free chemical radicals in healthy cells. A tumor occurs when these radicals damage the cell's DNA and interfere with its normal repair.
If we describe the sequence of development of skin melanoma due to the influence of UV radiation, it is as follows: UV radiation affects melanoblasts, melanocytes or nevus cells, cell DNA is damaged, cell differentiation is disrupted, the protein structure changes and new membrane antigens appear. Hyporesponsiveness and tumor growth are noted. The possibility of this mechanism of carcinogenesis is confirmed by the fact that melanomas often develop after a single and strong influence of UV radiation (with a sunburn).
The essence of the mechanism of the carcinogenic effect of injury to pre-existing pigmented nevi is tissue proliferation in response to damage. However, trauma does not provoke tumor development. Cells in a state of proliferation are more sensitive to carcinogenic effects. They are especially vulnerable during the mitotic cycle. Consequently, proliferation (active reproduction) of cells can provoke their neoplastic transformation.
If we describe the sequence of development of skin melanoma due to trauma to pre-existing pigmented nevi, it is as follows: nevus cells are damaged, inflammation and proliferation of the damaged tissue occurs. Long-term proliferation is observed, and under the influence of endogenous carcinogenic factors, the structure of the cell's DNA is disrupted. As a result, cell differentiation is disrupted, its protein structure changes, and new membrane antigens . Hyporesponsiveness and tumor growth are noted.
Signs of malignant degeneration
Signs of the transition of a typical pigmented nevus to melanoma are as follows:
- change or heterogeneity in color;
- rapid growth;
- dropouts (appearance of small dots around the central focus);
- blurred or broken boundaries;
- ulceration, bleeding, hyperemia;
- enlargement of regional lymph nodes.
It is difficult to distinguish melanoma from a nevus by external signs; a doctor’s examination is required
To determine treatment tactics, consultation with an oncologist and a surgeon is indicated.
Classification
In total, depending on the characteristics of the process, four types of melanoma are distinguished:
- Superficially spreading - according to statistics, approximately 70% of developing melanomas are of this type. Most often, this tumor is asymptomatic and develops on the skin of the legs in women and on the torso in men. The formation has irregular outlines, brown or light brown color, and there may be spots on the surface - red, white, blue or brown. It may also have small blue-black nodules. In some cases, small tooth-like notches appear along the edges, the size increases, and the color changes.
- Nodular melanoma – 15-30% of melanomas are of this type. It can appear on any part of the skin and looks like a black papule or gray-black plaque. It may be amelanoma (non-pigmented, meaning that it has no pigment at all) or it may contain little pigment. Nodular melanoma can also look like a vascular tumor.
- Lentigo malignant melanoma - up to 5% of such formations belong to this type. Most often develops in older people. Formed from lentigo maligna (Hutchinson's freckle or melanoma in situ). Typically, this melanoma appears on the face, but it can also form on other areas of the skin that have been exposed to sunlight. An asymptomatic flat spot or light brown or brown plaque appears on the face or other areas of the skin, having irregular outlines and unevenly located on the surface.
- Acral - 2-10% of formations belong to this type. This type of melanoma is most often diagnosed in people with dark skin color. It develops on the soles, skin of the palms, under the nails. Its symptoms and histological features are similar to lentigo melanoma.
- Amelanotic melanoma - any of the varieties listed above can be non-pigmented. Most often, small formations are non-pigmented (spitzoid, desmoplastic, neurotropic melanomas, etc.). This type occurs in less than 10% of cases. The color of this formation is pink, red or brownish. Since such a tumor can easily be mistaken for benign, late diagnosis often worsens the prognosis.
- Lentiginous melanoma of the mucous membranes is a rare form of the disease, occurring in approximately 1% of cases. Formed on the mucous membranes - in the nasal cavity, mouth, perianal and vulvovaginal areas. It is characterized by pronounced uneven pigmentation.
- Malignant melanoma of soft tissues - forms on ligaments and aponeuroses.
- Melanoma of the eye (uveal) - affects the eyelid, conjunctiva or choroid. Choroidal melanoma is also diagnosed, a tumor of the retina that develops from choroidal melanocytes. A tumor of the choroid of the eye is a lesion of its choroid. As a rule, it progresses rapidly. The prognosis is unfavorable - due to the aggressive development of the process, death is recorded in approximately 70% of cases.
- Subungual melanoma is a very dangerous type, as it can develop rapidly and at first unnoticed by the patient. Initially, a pigment spot develops under the nail, usually dark in color. The nail plate becomes brittle and sometimes deformed.
The types of the disease are also determined depending on the development of metastases during tumor progression. Melanoma of the central nervous system is a condition in which damage to the central nervous system develops. We are talking about secondary tumors of the central nervous system.
What are nevi?
- It can occur anywhere on the body and in any age group. It is most often found on the skin from birth, and increases in proportion to the child’s growth (in case of excessive growth, immediate consultation with an oncologist is required).
- One of the most common skin formations (80-90% of the population). Occurs more often in women. In representatives of dark races, pigmented nevi are less common than in whites.
- It does not cause discomfort to a person and has no symptoms even in case of degeneration (10-20%). For this reason, self-monitoring and periodic (once a year) examination by an oncologist are recommended.
- In older people, pigmented nevi are more common due to age-related skin characteristics.
- Moles are extremely sensitive to external influences (direct sunlight, for example). They have a tendency to malignancy, especially in constantly injured areas. The only treatment option is surgical removal of the formation.
Causes
Skin melanoma develops due to a combination of the influence of the underlying cause and environmental conditions, as well as the internal environment of a person. Today, scientists do not have data on the main etiological factor in the development of skin melanomas. There is a theory that melanoma is a polyetiological disease.
Factors influencing the development of this disease are divided into exogenous and endogenous .
The following exogenous factors :
- Place of residence of a person (geographical latitude) and associated solar radiation activity. The influence of the ultraviolet spectrum is one of the most important factors affecting the development of skin melanomas. Its negative impact is also determined by the fact that ozone decreases in the stratosphere, which leads to an increase in the carcinogenicity of solar radiation. There is confirmed evidence that what is more dangerous in this context is not the chronic influence of ultraviolet radiation, but its sudden and very strong influence, sometimes one-time. Sunburns received in childhood and adolescence are important.
- Injuries to pre-existing nevi - bruises, cuts, abrasions, as well as chronic injury from clothing or shoes.
- The influence of chemical carcinogens.
- Fluorescent lighting – a negative effect is observed with intense exposure to fluorescent lighting sources.
- Ionizing radiation.
- Electromagnetic radiation.
- Socio-economic factors also play a role. In particular, it is noted that the incidence is higher among the urban population; that patients tend to have a higher social status. It is also noted that melanomas occur more often in people working in the rubber, electronics, petrochemical, and coal industries; in contact with polyvinyl chloride, plastics, benzene, pesticides, radiation.
- Biological - dietary habits (large amounts of proteins and fats in the diet), bad habits (alcohol abuse), and taking certain medications have a certain influence.
The development of the disease is also influenced by the following endogenous factors :
- Precancerosis – there are a number of conditions against which a tumor can develop. These are xeroderma pigmentosum (hereditary, recessively transmitted photodermatosis), Dubreuil melanosis (lentigo - areas of skin pigmentation).
- Nevus plays a certain role in the etiology of skin melanomas. It should be noted that in addition to pigmented ones, there are non-pigmented nevi. In addition, there are so-called acquired nevi that appear during life, and which a person may not notice until they transform into a malignant formation. Nevi are a morphologically unstable population of cells, since their localization in the layers of the skin changes throughout life. The number of nevi depends on the hormonal background of the body. Nevi should be considered a phenotypically unstable population of cells. The fact that melanomas develop from nevi is generally accepted, but still, research and observation data do not allow us to state that nevi are the cause of absolutely all melanomas.
- Biological - researchers note that the tumor develops more often in people of the white race. A pigmentation disorder in the body, in which the skin reacts inadequately to ultraviolet radiation, also plays a role. Melanoma most often develops in people with weak skin pigmentation and high sensitivity to UV radiation. Those who are prone to sunburn are more likely to get sick. Heredity also plays a certain role. It has been established that melanoma is inherited in an autosomal dominant manner. Hormonal fluctuations also influence the development of the disease ( estrogens and androgens ). Certain importance is attached to immune factors - the risk of disease is increased by immunosuppression and immunodeficiency states.
Characteristics of various types of pigmented nevi
Border
It is formed in utero (often it does not appear immediately, but 1-2 months after birth). There is no favorite localization; it occurs on any area of the skin. The risk of transformation into a malignant form is high. The prognosis is favorable with proper treatment.
Appearance (pictured):
- flat lesion of round or oval shape;
- color from dark brown to black, uneven color (pigmentation intensifies at the edges in the form of concentric rings);
- size from a few millimeters to 4-5 cm;
- the surface is smooth, the boundaries are clear;
- hair may grow on the surface of the formation;
- single or multiple;
- sometimes there is slight infiltration around the formation.
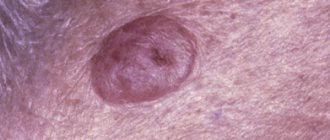
Intradermal
It usually occurs between 10 and 30 years of age. Favorite localization is the face, neck, torso. The prognosis is favorable. The risk of malignancy is low.
Intradermal nevus has clear boundaries and is dark in color.
Appearance:
- papule or node with a diameter of up to 1 cm (protrudes above the surface of the skin);
- spherical or hemispherical shape;
- color dark brown or black.
Difficult
Occurs in people of all ages. Favorite localizations are the face, scalp and torso. The prognosis is favorable, the risk of malignancy is average.
Appearance:
- up to 1 cm in diameter;
- covered with hair;
- located at skin level;
- has a light brown tint.
spindle cell
It is also called Spitz nevus. It predominates in children; it practically does not occur in older people. Favorite localization – face, legs. The prognosis is favorable (prone to involution), the risk of degeneration is low.
Appearance:
- often single;
- round or oval shape;
- the surface is smooth (less often it can be warty);
- color from pink to dark brown;
- diameter on average 1-2 cm;
- affects deep-lying layers, therefore it can bleed when injured.
Balloon cell nevus
It occurs more often in young people. There is no favorite localization. The prognosis is conditionally favorable due to rapid growth, the risk of malignancy is average.
Externally:
- has the appearance of a spot, does not protrude above the skin;
- color from yellow to dark brown;
- has clear boundaries (yellow rim around the formation).
Skin melanoma symptoms
Photo of the initial stage of skin melanoma
The clinical picture of pigmented malignant tumors can be very diverse. Therefore, the symptoms of skin melanoma can manifest in different ways. The tumor can have different shapes, colors, sizes, etc.
Since this tumor is formed from melanocytes (pigment-forming cells), it can develop in almost any organ or tissue. But still, melanoma most often appears on the skin.
The question of how to recognize melanoma is quite complex. After all, its clinical picture has high variability. Melanoma develops predominantly on congenital or acquired nevi. However, a tumor can also appear if the patient has Dubreuil melanosis, as well as on skin where there are no signs of a nevus or other formation.
Due to the fact that the degeneration of a mole into melanoma is a fairly common phenomenon, it is necessary to clearly know the clinical manifestations of malignancy of nevi. Simply put, you need to understand how to distinguish a mole from a melanoma, what melanoma looks like, and identify which birthmarks are potentially dangerous.
The following signs should alert a person:
- growth, induration or ulceration of the nevus;
- weakening or strengthening of the color of the birthmark;
- the appearance of radiant growths around the nevus - they can be either pigmented or non-pigmented;
- hyperemia or stagnant halo around the birthmark;
- the appearance of an exophytic component on its surface;
- frequent development of bleeding;
- enlargement of regional lymph nodes;
- the appearance of satellites near the nevus - pigmented or non-pigmented nodules.
It is important to consider that the symptoms of the initial stage of melanoma are difficult to determine, since the first signs of malignancy are often similar to the symptoms of a normal inflammatory process.
Photo of skin melanoma
In typical cases, the initial stage of skin melanoma manifests itself as follows: a birthmark for no apparent reason or after an injury begins to grow. Its color changes, and an exophytic tumor appears in one of the areas of the nevus. The initial stage is not always determined in a timely manner, since melanoma during this period can have a small diameter: as a rule, it is no more than 1-2 cm. Large tumor nodes form in the later stages.
During the development of the tumor, the signs of skin melanoma can be varied: it can be a flat spot, a formation with a slight protrusion, papilloma growth, mushroom-shaped formation, etc.
The shape of the tumor can be round, oval, or irregular. As a rule, melanoma is a solitary formation. But often additional outbreaks appear near it. They can either merge with the main tumor (multicyclic form), or be located nearby and separated from the tumor by areas of healthy skin.
The surface of the tumor may initially be shiny and smooth, but later irregularities and ulcerations appear on it. The tumor site may bleed even with minor trauma. As the tumor grows, tissue infiltration and disintegration of the tumor node often appear on it, as a result of which the surface resembles cauliflower. Sometimes there are no signs of ulceration, and thin skin covers the tumor. In rare cases, early stage melanoma begins as localized redness and gradually develops into an ulcer that does not heal.
The consistency of the tumor can also be different - it can be either soft or hard or dense. One tumor can form areas of varying consistency.
The color of the tumor depends on the amount of melanin. It can be purple, red, blue-black, brown, black. Pigmentation may be uniform or uneven. In the center the tumor appears more pigmented.
When benign nevi become malignant, their color often changes. This is one of the warning signs. Pigmentless tumors develop to form secondary tumors containing pigment. In the later stages of melanoma, the patient’s general well-being also worsens.
Thus, the signs of nevus malignancy are the following symptoms:
- nevus growth along the plane and above the skin;
- bleeding from its surface;
- asymmetry of its edges;
- peeling of the surface;
- change;
- burning sensation in the area of the nevus;
- hair loss from its surface;
- formation of nodes.
Kinds
Classification of melanocytic nevi according to J. Bhawan (1979) depending on the origin:
| View | Subspecies |
| Epidermal | Intraepidermal, borderline, complex. This group also includes special forms: spindle cell or epithelioid, nevus of balloon-forming cells, halonevus |
| Dermal | Mongolian spot, nevus of Oto, nevus of Ito and blue |
| Mixed dermal and epidermal | Combined |
| Melanoma precursors | Congenital, dysplastic |
Formations of epidermal origin are usually acquired and occur in adolescence.
Size classification:
- small (0.5–1.5 cm) – only observation is indicated;
- medium (1.5–10 cm), planned surgical removal of the tumor is optimal;
- large (over 10 cm) planned palliative therapy is indicated (surgical treatment due to the large area is not always indicated);
- giant – occupy one or more anatomical areas; Only palliative therapy and observation are indicated (surgical treatment is not used).
Tests and diagnostics
It is very important to see a doctor as soon as possible, because the success of treatment depends on how quickly the diagnosis is made.
Dermatoscopy is a method for early diagnosis of melanoma. To carry it out, a magnifying glass or a dermatoscope (epiluminescence microscope) is used. During the diagnostic process, it is possible to determine whether a nevus is dangerous. The doctor makes conclusions using the so-called ABCDE system . It has been used since 1985, analyzing nevi and determining the presence of such changes:
- A - asymmetry, that is, asymmetry;
- B - border irregularity, the presence of an uneven edge
- C - color, different parts of the mole have different colors;
- D — diameter, diameter greater than 6 ml;
- E - evolving, variability.
In modern medicine, a number of research methods are used when the development of melanoma is suspected.
- Indication of a tumor with radioactive phosphorus is based on the fact that selective accumulation of radioactive phosphorus occurs in the tissue of a growing malignant tumor. This test has not only diagnostic value, but also allows you to evaluate the effectiveness of treatment.
- Thermal differential test - it is based on the temperature difference between the tumor site and healthy skin. An electric thermometer is used to carry out the test.
- Cytological diagnosis is the only morphological method for verifying a clinical diagnosis. a biopsy be performed if melanoma is suspected because of the danger of stimulating the growth of the tumor. To conduct the study, smears and scrapings are taken from the surface of the tumor. If melanin pigment is present in the cytoplasm of tumor cells, this is a significant sign of the development of melanoma. For different types of tumor, distinctive features are determined during a cytological examination.
The final diagnosis is established after a histological examination, which is carried out after total removal of the nevus. If necessary, additional research is carried out.
Treatment
Treatment is indicated for dysplastic, nodular and giant pigmented nevi due to their possible malignancy • Indications for excision of any pigmented formation •• Change in color, size, shape and consistency •• Pain syndrome •• Regional lymphadenopathy • Further therapy after excisional biopsy of a healthy area skin are prescribed based on the results of histological examination and localization of the formation.
ICD-10 • D22 Melanoform nevus • I78.1 Non-tumor nevus • Q82.5 Congenital non-tumor nevus
Application. Sturge-Weber syndrome (185300) is classified as phakomatoses, characterized by a triad: congenital cutaneous angioma (flaming nevus), usually along the trigeminal nerve, often unilateral; homolateral meningeal angioma with calcification and neurological signs; angiomas of the choroid, often with secondary glaucoma; in incomplete forms, any two or more signs are possible, sometimes with angiomas of a different localization “encephalotrigeminal angiomatosis” Sturge-Weber disease “nevoid amentia.”
Treatment with folk remedies
Under no circumstances should you use unverified sources regarding any traditional methods of treating melanoma. Treatment with herbal preparations, soda or other methods can lead to short-term relief of the condition, but in the end the person will miss precious time, and the outcome will be sad.
Many similar reviews and stories can be found on thematic forums: “Melanoma Fight”, “Life Forum”, etc. If you read any patient forum or VKontakte discussions, you can find out a lot of evidence that treatment with traditional methods can become a fatal mistake.
Prevention
To prevent the development of a malignant tumor, important rules of prevention should be taken into account:
- Conduct self-diagnosis, paying attention to all changes in nevi. At the first suspicion, consult a doctor. If a specialist advises removing the nevus, you must do so.
- Avoid exposure to harsh sunlight. Do not be in the sun from 10 am to 4 pm, do not overuse sunbathing, and do not visit solariums. When exposed to sunlight, wear clothing that protects exposed skin.
- Use sunscreens with a protection factor (SPF) of 30 or more. Follow the instructions when using such products.
Diet
Diet for cancer
- Efficacy: no data
- Duration: until recovery or lifelong
- Groceries cost: 2500 - 4800 per week
The diet of patients with melanoma should be light, low in calories, but still contain a sufficient amount of protein. The menu must include the following products:
- Lean meat - chicken, turkey, rabbit, beef, veal.
- Eggs – preferably quail.
- Vegetables – carrots, pumpkin, avocado, broccoli.
- Fruits – apples, citrus fruits.
- Cereals – buckwheat, lentils, wheat.
- Legumes - peas, beans.
- Dairy – cheese, milk, curds.
- Fish, seafood.
- Sesame seeds, flax.
- Nuts.
- Green tea.
It is better to cook by steaming, in the oven, using natural seasonings and spices. It is better to avoid fried foods. It is recommended to replace side dishes with boiled vegetables.
The following foods should be excluded from the diet:
- Margarine.
- Lard, animal fats.
- Sweets.
- Alcohol.
- Smoked meats, canned food.
- Pickles.
Prognosis for melanoma
This tumor spreads very quickly, so the prognosis depends on how early the disease is diagnosed and treatment started.
- In the first stage, the 5-year survival rate is 95-97%, the 10-year survival rate is 95%.
- Prognosis for stage 2 melanoma: 5-year survival rate is 70-86%, 10-year survival rate is 57-67%.
- At the third stage: 5-year survival rate – 40-78%; 10-year survival rate – 24-68%.
- Life expectancy at stage 4: 5-year survival rate - 15-20%. 10-year survival rate is 10-15%.