Reasons for the appearance of a halo around a nevus
There are several reasons why a white spot appears around a mole.
- Heredity . If parents have moles on their bodies surrounded by a light spot, then there is a high probability that their children will also experience a similar phenomenon.
- Ultraviolet . When the sun's rays hit the skin, it can cause various changes. A white rim around a mole can also appear under the influence of ultraviolet rays. Some people experience this after sunbathing on the beach or in a solarium.
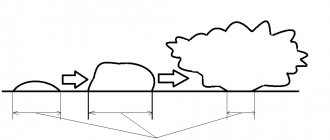
- Hormonal changes in the body. Changes in hormonal levels caused by various processes occurring in the body are another reason for the formation of a white spot on the skin. This can happen during pregnancy, menopause, in adolescence during puberty, after suffering stress or serious illness, as well as as a result of long-term use of hormonal drugs. Sometimes a severe hormonal imbalance in the body can cause a mole to completely disappear from the skin. However, this does not happen at one moment, but gradually: first a white halo appears around it, which increases in size and absorbs the nevus until it disappears completely.
- Radioactive radiation. If a person has been exposed to radiation, they may develop white spots around the nevus. Since radioactive radiation often leads to the formation of malignant tumors, a light rim around moles may indicate the beginning of this process.
- Mechanical impact. If a mole frequently rubs against clothing or is squeezed by it, white areas may form around it.
- Degeneration of a nevus into a malignant formation. The most dangerous reason for the appearance of a halo around a mole is the beginning of the process of its degeneration into skin cancer. Therefore, it is very important to recognize the threat in time and begin treatment.
Should the stain be removed or lightened?
If the stain does not pose a danger, is a benign formation that does not cause discomfort, you do not need to remove it, but carefully monitor it using photography techniques.
If the slightest changes appear, you should visit a doctor.
At the doctor's appointment, the area causing concern will be examined and after dermatoscopy a final diagnosis will be made. A mole with a rim of brown or other color is dangerous and requires surgical or laser removal. The procedure involves complete excision of the malignant tumor, with minor damage to healthy skin. Helps prevent further spread of melanoma cells. Removal must take place in a clinic using a special device. You should not go to beauty salons to solve this problem. Improper excision will lead to serious complications, possibly fatal.
The procedure for lightening moles is harmful; a highly qualified specialist will not resort to it; there is a risk of transformation of the nevus.
Types of nevi with a white halo
There are several types of birthmarks, surrounded by a light rim.
- Nevus of Sutton. It is an ordinary mole, around which there are white areas of skin that have an irregular shape or merge with each other. Such formations often appear in adolescence and can be single or multiple. They do not pose a threat to health and extremely rarely degenerate into a malignant formation.
- Nevus of Setton. This mole looks like a separate pigment spot surrounded by a large light halo. The size of the rim can reach 1 cm in diameter. In some cases, the skin around moles has a white-brown, mottled tint. Such a nevus also does not cause any inconvenience to a person.
- Vitiligo . This is a genetic disease, as a result of which the human body stops producing the pigment melanin. As a result, white spots appear around moles and in general on any areas of the skin. This disease can occur in both children and adults.
READ ALSO: How to distinguish dangerous and non-dangerous moles
Benign pigmented skin neoplasms (moles)
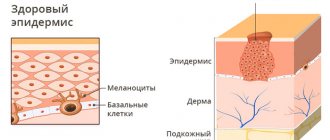
Nevus ( noncellular nevus , pigmented nevus , nevoid tumor , birthmark ) is a pigmented (colored) formation on the skin, which includes nevus (pigment) cells. Nevi are benign neoplasms; most researchers associate their occurrence with the migration in the embryonic period of the precursors of pigment cells (melanoblasts) from the neuroectodermal tube to the basal layer of the epidermis.
The nevus is of particular interest due to the fact that in place of a pre-existing congenital or acquired benign nevus, such a formidable malignant neoplasm as melanoma .
Almost all people have various congenital and acquired nevoid neoplasms. More than 90% of the population has pigmented skin tumors. The average number of nevi in each person is 20, ranging from 3 to 100, and their number usually increases with age. Not all nevi can potentially degenerate into melanoma, so they are usually divided into melanoma-hazardous and melanoma-non-hazardous.
Melanoma-dangerous nevi are much less common (about 10%) than melanoma-non-dangerous nevi. These nevi do not differ in the age of patients, localization of lesions and other clinical and anatomical data. It is important to consider that it is impossible to carry out differential diagnosis based on the degree of pigmentation of the lesion. Various injuries - mechanical, chemical, radiation, both acute and repeated - can be factors that provoke the transformation of some types of nevi into melanoma, primarily borderline or other melanoma-hazardous ones. In this regard, a biopsy of a suspicious skin element is strictly contraindicated, as well as its cosmetic treatment using directly traumatic methods (partial removal, electrocoagulation, cryotherapy, exposure to chemical and other agents). The percentage of melanoma patients who have clear indications of trauma preceding the development of the tumor (after incomplete cosmetic removal of a pigmented nevus, accidental trauma) varies from 20 to 78%. A biopsy or incomplete removal of the lesion in order to distinguish a melanoma-dangerous nevus from melanoma or other skin lesions is strictly unacceptable.
General principles of treatment of pigmented neoplasms
Any pigmented skin growths require special attention. Greater caution should be shown to nevi localized in traumatic areas of the skin, as well as to previously injured nevi that are rapidly growing or rapidly changing their pigmentation.
Therapeutic tactics for pigmented nevi boil down, first of all, to the categorical refusal of any traumatic treatment methods: electrocoagulation, cryodestruction and the use of various cauterizing solutions.
Treatment of pigmented neoplasms is radical surgical excision of the lesion within intact skin. The use of modern non-traumatic suture materials and the rules of aesthetic surgery makes it possible to achieve barely noticeable postoperative scars. Surgical treatment (excision along the edge of the formation), as well as various cosmetic manipulations (cryodestruction, chemodestruction) of melanoma-free neoplasms do not carry the risk of malignant transformation of these formations.
A completely different tactic is followed for melanoma-dangerous nevi. If a melanoma-hazardous formation is suspected, the patient should be immediately sent to an oncologist! The tactics and technique of surgical intervention are determined by the location and size of the melanoma-dangerous pigmented nevus. The best limits for excision on the trunk and limbs, taking into account, on the one hand, the clear limitation of “quiet” nevi and, on the other hand, cosmetic considerations, is considered to be a distance of 0.5 cm in all directions from the borders of the nevus; this is quite sufficient for the prevention of melanoma. The nevus is excised with surrounding incisions along with the surrounding skin and the surface layer of tissue; the tissue is sutured with a cosmetic suture using non-traumatic suture material, which allows one to achieve good cosmetic results. On the face, neck, auricle, fingers and nail bed, for anatomical and cosmetic reasons, more economical excision of melanoma-dangerous nevi is allowed, but not less than 0.1-0.2 cm from their borders. On the face and neck, sutures are applied with a very thin thread, which allows for maximum cosmetic effect. In all cases of surgical excision of a pigmented nevus without exception, histological confirmation of the diagnosis is necessary - i.e. the excised area is necessarily sent for microscopic examination; if the result is atypical cells (melanoma), the patient is referred to an oncologist.
Patients who refuse radical surgical treatment, as well as in the case of its impossibility due to difficult anatomical localization, should carefully protect their tumor, exclude its injury, solar radiation and be monitored by an oncologist.
Borderline pigmented nevus
A borderline pigmented nevus is a flat dark brown or black nodule up to 1 cm in diameter with a smooth, dry surface, develops at the border of the epidermis and dermis, and is characterized by increased activity of pigment cells (melanocytes). Sometimes a border nevus looks like a spot of round or irregular shape with smooth wavy edges. Borderline nevus does not have a favorite location. It can be located on the skin of the face, neck, and torso. Pigmented nevi on the skin of the palms, soles, and genitals are almost always borderline. Borderline nevus is most often congenital, but can appear in the first years of life or even after puberty. An important differential diagnostic sign of a borderline pigmented nevus is the complete absence of hair on it.
Pigmented border nevus must be distinguished from cavernous hemangiomas, which are characterized by a softer consistency of the node, from seborrheic (“senile”) keratoma, which, as a rule, has a less smooth, “rough”, greasy surface. In the differential diagnosis between borderline pigmented nevus and early melanoma, anamnesis plays an important role. Most patients with melanoma indicate that their tumor developed in place of a pigmented nevus that existed for a long time or even from birth, which did not cause any inconvenience. The nevus grows slowly according to body weight. During puberty, patients may notice an acceleration in nevus growth - a consequence of hormonal changes and an increase in the level of metabolic processes, including pigmentation. Mechanical trauma is the predominant factor accompanying the malignancy of previously “quiet” nevi.
The following borderline nevi are especially dangerous: systematically injured, located on the sole, nail bed, or in the perianal area. Timely removal of nevi in these localizations is a reliable prevention of melanoma. Excessive insolation, thermal or balneological treatment of concomitant chronic diseases also play a negative role in the development of melanoma. Acceleration of nevus growth after injury or active insolation, inflammatory changes, discoloration, the appearance of itching, weeping, and induration should be alarming.
Blue or blue nevus
Blue or light blue nevus (Jadassohn-Tiche nevus) is a dark blue or bluish node, sharply demarcated from the surrounding skin, round in outline, densely elastic consistency with a smooth, hairless surface. The blue color is due to massive accumulations of melanin in the deep layers of the dermis. The size of the node, as a rule, does not exceed 0.5 cm. Blue nevus is most often located on the face, limbs, and buttocks. In most cases, blue nevus is a solitary formation. Blue nevus occurs in all age groups, most often in middle-aged women . Clinically, a blue nevus is difficult to distinguish from a pigmented borderline nevus. However, clinical features such as large demarcation and infiltration, blue or blue color, appearance at a later age and hemispherical shape allow for a differential diagnosis. With a deeper location in the skin, a blue nevus sometimes has to be differentiated from a dermatofibroma. Symptoms such as less infiltration, color and usually a solitary lesion help to distinguish it. The development of melanoma at the site of a blue nevus is rare, but this nevus is classified as melanoma-dangerous .
Nevus Ota
Nevus of Ota, or oculodermal melanocytosis, is a large, usually unilateral pigmented nevus on the face in the area of innervation of the I and II branches of the trigeminal nerve (the area of the forehead, cheeks and nose). Clinically, dark brown pigmentation is noted in various parts of the eye: conjunctiva, sclera, iris. At the same time, a massive pigmented nevus (or nevi merging with each other) is detected on the cheek, upper jaw and zygomatic region of the same side, black and bluish in color. All this creates the impression of “dirty skin” on the affected side of the face. In rare cases, the red border of the lips and the mucous membranes of the soft palate, pharynx, larynx and nose are affected. Women get sick more often. Nevus of Ota is congenital, but can occur in early childhood or even during puberty. It usually grows slowly. Apart from cosmetic inconveniences, it does not cause any disorders, including visual impairment. There are known cases of melanoma developing in its place. Close to the nevus of Ota and an even rarer variety is considered to be the nevus of Ito, located in the supraclavicular, scapular regions and the deltoid muscle region.
Giant pigmented nevus
A giant pigmented nevus is always congenital, increases in size as the child grows, reaching a large size (from the palm of the hand or more) and sometimes occupies a large part of the torso, neck and other areas. Usually, over a considerable extent, the surface of the nevus is lumpy, warty, with deep cracks in the skin. Areas of hypertrichosis (hair nevus) are common. The color varies from grayish to black and is often heterogeneous in different areas. Malignancy of a giant pigmented nevus occurs in 1.8-10.0% of cases. Treatment tactics for suspected pigmented borderline and blue nevi, especially if they are located on accessible insolation and frequently injured areas of the skin, boil down to the categorical refusal of any traumatic treatment methods: electrocoagulation, cryotherapy, the use of various cauterizing solutions and incomplete surgical excision. If necessary, economical surgical excision of the lesion with the surrounding skin is performed at a distance of 0.5 cm in all directions from the borders of the nevus along with subcutaneous fatty tissue; this is quite enough to prevent melanoma. On the face, neck, auricle, fingers, due to anatomical features, a more economical excision of melanoma-dangerous nevi is permissible with a deviation of 0.2-0.3 cm from its borders. For giant nevi, which cause great cosmetic inconvenience to patients, step-by-step excision is used, followed by skin plastic surgery .
Dubreuil's melanosis
Dubreuil's melanosis is a nevoid formation, the connection of which with melanoma is indisputable. Dubreuil's melanosis usually begins as a small brownish pigmented spot that slowly spreads around the periphery. A clinically mature lesion has blurred boundaries and an uneven surface of dark brown and sometimes black color, more saturated than the color of pigmented nevi. Within the formed focus there are areas of different shades (brown, gray, black, bluish). The skin pattern over the lesion remains unchanged and becomes rougher. Elements resembling a senile wart may appear. Sometimes atrophy, hyperkeratosis, and flat surface papillomatosis develop. Characterized by increased pigmentation along the periphery of the lesion. Inflammatory phenomena are extremely rare. In most patients, Dubreuil's melanosis manifests itself in one focus. The most common location is open areas of the skin, especially the face (cheeks, nasolabial folds, nose, forehead), less often the neck and scalp. Dubreuil's melanosis mainly affects older people, which allows it to be classified as a senile dermatoses. The clinical picture of limited precancerous Dubreuil's melanosis, especially in the stage of a formed lesion, in most cases is so characteristic that it does not cause great diagnostic difficulties.
Differential diagnosis must be made with large seborrheic (senile) keratoma, pigmented basal cell carcinoma, and some forms of nevi. However, all these nosological forms are characterized by clearly demarcated lesions. With basal cell carcinoma, a raised ridge with “pearls” is visible (especially through a magnifying glass); the central part of the tumor is often ulcerated. The surface of a seborrheic keratoma is more lumpy and often “greasy” to the touch. A clinical symptom such as uneven hyperpigmentation, as well as medical history - onset of the disease in old age and very slow progression of a single lesion - are very helpful in diagnosing Dubreuil's melanosis.
The causes of malignancy of Dubreuil's melanosis have not been established; trauma and insolation are considered to be the impetus for the onset of invasive tumor growth . Dubreuil's melanosis is a more pre-melanoma skin lesion than borderline pigmented nevus, not to mention other melanoma-dangerous nevi. Therefore, Dubreuil’s melanosis is considered not so much melanoma-dangerous as directly pre-melanoma and even an absolute precancer of the skin .
The treatment strategy for Dubreuil's melanosis differs significantly from that for melanoma-dangerous nevi. First of all, it is unacceptable to leave patients without active treatment , which is possible with Ott’s nevus and other melanoma-dangerous nevi after warning patients about the danger of injury. Another difference is that wide surgical excision of Dubreuil's melanosis , given its predominant location on the face, is associated with serious technical and cosmetic difficulties, especially with large lesions . Sometimes excision of large lesions on the body is completed with plastic surgery using displaced flaps. The method of choice for Dubreuil's melanosis on the trunk and limbs is excision of the lesion, 0.5 cm from its edges.
Fibroepithelial nevus
Fibroepithelial nevus belongs to the group of melanoma-NON-dangerous nevi and nevoid skin lesions . Fibroepithelial nevus, along with pigmented intradermal nevus, is the most common nevoid formation on human skin and the most common reason for visiting a surgeon. Fibroepithelial nevus often first appears during various periods of intrauterine life, sometimes existing from birth. Its growth is usually very slow. Localization can be very different, but mainly on the face and torso. The number of formations varies from one to several dozen. Histologically, fibroepithelial nevus has the structure of a soft fibroma.
Clinically, a fibroepithelial nevus is a hemispherical, painless formation rising above the skin level with a soft or soft-elastic consistency ranging from a few millimeters in diameter to the size of a bean and, rarely, larger. Color varies from normal skin or pinkish-red (usually with a slight bluish tint) to bluish-violet and dark brown. With the latter or close to it coloring, the greatest difficulties arise in differential diagnosis with borderline pigmented and blue nevus. The shape of a fibroepithelial nevus is usually regular, round, and the surface is smooth, although less smooth than that of a borderline pigmented nevus. The surface of the nevus is often penetrated by single vellus or bristly hairs or even a coarse tuft of hair, especially in women (fibroepithelial pilaris nevus). With a pronounced vascular component in the form of a telangiectatic mesh on the surface, they speak of angiofibroepithelial nevus, which can also be hairy.
In most patients, there is no inflammation around the fibroepithelial nevus. Sometimes after an injury the nevus becomes inflamed (when shaving the face, after a blow). In these cases, an inflammatory rim develops around the circumference. In typical cases, diagnosing a non-inflammatory fibroepithelial nevus is not difficult. Differences from borderline pigmented and blue nevi: color (even with pigmented fibroepithelial nevi, the color is less saturated), shape, multiplicity, frequent presence of hair. In its clinical picture, an inflamed fibroepithelial nevus differs sharply from the picture observed during malignancy of a melanoma-dangerous nevus.
Papillomatous nevus
Papillomatous nevus has an uneven, bumpy surface, often localized on the scalp, but can also occur on any other part of the skin. The sizes are often large, up to several centimeters, the outlines are irregular, the color varies from the color of normal skin to brownish, less often - dark brown or even black. Like fibroepithelial nevus, papillomatous nevus is often riddled with hair. As a result of injury, the papillomatous nevus becomes inflamed. The location of the papillomatous nevus on the face and other open areas of the skin causes patients to persistently desire to get rid of the formation, which can be subjected to cosmetic treatment.
Verrucous nevus
Verrucous nevus is a clinical type of papillomatous nevus. Its surface is even more lumpy, in pronounced cases it has the appearance of a “head of cabbage”, penetrated by deep folds and cracks. It protrudes significantly above the surface of the skin and is usually more pigmented (pigmented, or pigmented verrucous nevus). Like papillomatous nevus of the extremities, most often there is a single focus. Clinical recognition of verrucous nevus does not present any particular difficulties. Sometimes, especially if it is small, a verrucous nevus can be mistaken for a giant common wart. Correct recognition is helped by anamnestic data (exists from birth or early childhood, grows very slowly), frequent presence of hair on the surface; usually the lesion is single. The treatment and tactical approach is similar to papillomatous nevus.
Halo nevus (Setton's nevus)
Halo-nevus is clinically a reddish-brown nodule, slightly raised above the skin level, 4-5 mm in diameter, round or oval, surrounded by a rim of depigmented skin. The width of the depigmented area is 2-3 times greater than the diameter of the hyperpigmented nodule. Halo nevus is often multiple, predominantly localized on the torso and arms, less often on the face. Often, Halo nevus undergoes spontaneous regression. The clinical picture of Halo-nevus is typical and does not cause differential diagnostic difficulties. The development of melanoma at the site of the Halo-nevus, even after injury, is not observed. It has been noted that Halo nevus sometimes occurs in malignant tumors of internal organs and melanoma.
"Mongolian Spot"
“Mongolian spot” is an irregularly shaped rounded skin lesion, colored bluish or brownish, up to 5-6 mm in diameter, located exclusively in the lumbosacral region. The “Mongolian spot” is almost always a congenital formation; in most patients it disappears without a trace in childhood. The development of melanoma at the site of the “Mongolian spot” is not observed and does not require treatment.
Intradermal nevus
Intradermal nevus, or common birthmark, occurs in almost all people. Birthmarks are located in the skin and mucous membranes. Most often, these nevi are congenital; the pigmentation is usually brown. For the vast majority of people, birthmarks do not cause cosmetic discomfort.
Dysplastic nevus
Dysplastic nevus is an acquired pigment formation, histologically represented by a random proliferation of polymorphic atypical pigment cells (melanocytes). It occurs on clear skin or as a component of a complex nevus. Dysplastic nevus has characteristic clinical and histological features that distinguish it from acquired noncellular nevi. It is considered a precursor to superficial spreading melanoma and is considered a risk factor for melanoma.
Dysplastic nevus are pigmented spots of irregular shape and with unclear boundaries, slightly raised above the skin level, their color varies from reddish-brown to dark brown on a pink background. Dysplastic nevi first attracted attention for their unusual appearance and increased frequency in some families (they are inherited). As a rule, they are larger than ordinary birthmarks, reaching 5–12 mm in diameter; the localization is also different: dysplastic nevi, although they can occur anywhere, are more often found in areas usually covered by clothing (on the buttocks, chest), or on the scalp. Most people have an average of 10 ordinary moles, while dysplastic nevi can have more than 100. Ordinary nevi usually appear during puberty, while dysplastic nevi continue to appear even after 35 years.
Comparative characteristics of dysplastic nevus and acquired noncellular nevus
| Sign | Dysplastic nevus | Acquired noncellular nevus |
| Color | Heterogeneous - various combinations of light brown, brown, black, red and pink; dysplastic nevi can differ significantly from each other | Uniform - light brown or brown |
| Form | Incorrect; fuzzy, blurred boundaries; peripheral areas are at skin level | Regular, round or oval; boundaries are clear; the formation is either at the level of the skin or evenly raised above it |
| Dimensions | Usually > 6 mm in diameter, often > 10 mm; occasionally < 6 mm | Typically < 6 mm in diameter |
| Quantity | Often multiple (> 100), but single lesions possible | On average, an adult has from 10 to 40 nevi; approximately 15% do not have them at all |
| Localization | Open areas of the body, most often the back; found on the scalp, mammary glands and buttocks | Typically exposed areas of the body above the waist; scalp, mammary glands and buttocks - extremely rare localization |
Vascular nevus
Vascular nevus (naevus flammeus, port-wine stain) is an anomaly of the capillaries of the dermis, manifests itself in the form of a spot from light pink to red-brown. Vascular nevus, located in the center of the face or back of the head, is not combined with other developmental defects and usually fades with age. With an asymmetrical, unilateral localization (on the face or limbs), a vascular nevus is usually one of the manifestations of Sturge-Weber syndrome or Klippel-Trenaunay syndrome. In this case, with age, the nevus usually darkens, and its surface in some places becomes bumpy and rises above the skin level.
Capillary hemangioma
Capillary hemangioma or strawberry nevus is the most common congenital vascular tumor. It begins as one or more pale pink papules that grow rapidly, become lobulated, and range in color from bright red to dark blue. Capillary hemangiomas appear at 3-5 weeks of life; 70% of them disappear spontaneously by the age of 7 and do not require treatment. Treatment. If the location and rapid growth of the tumor lead to visual or respiratory problems, resort to the injection of corticosteroids into the lesion, cryodestruction, laser therapy or surgical excision.
Are white spots around a mole dangerous?
White patches of skin in themselves do not pose a health threat. But if there are other symptoms indicating the development of a pathological process, then you should immediately show the nevus to a doctor. So, the following signs are cause for concern:
- the shape and size of the nevus changes;
- the edges become uneven;
- cracks, peeling, nodules, and bumps appear on the surface of the mole;
- it is swollen and inflamed;
- pain, burning, itching and other unpleasant sensations are felt;
- blood, pus or exudate is released from the mole;
- the nevus changed color.
If you have one or more symptoms, you should consult a doctor. All these phenomena may indicate malignant degeneration of the birthmark, so it is very important to conduct an examination as early as possible.
Dangerous symptoms
An immediate visit to a doctor is necessary if, in addition to changes in skin color near nevi, the patient is concerned about:
- A feeling of itching, discomfort, burning and, especially, pain in the area of the mole.
- Change in color of the mole itself.
- An increase in the size of the neoplasm, including its thickness.
- Changing the usual shape of a mole.
- The appearance of bleeding and any discharge.
- Peeling of the surface of the mole.
- The appearance of bumps, cracks, etc. on the mole.
Even if a person has only one dangerous symptom from the above, you need to make an appointment with a doctor as soon as possible and not experiment with your own health.
Treatment of nevus with a white rim
If you don't like a mole with a white halo, you can get rid of it. To do this, you need to see a dermatologist. To begin with, he will prescribe a special examination for you, which will determine whether the nevus is a benign formation and whether it can be removed.
If everything is in order, you will be asked to choose one of the methods for removing the birthmark. Modern medicine offers several methods:
- electrocoagulation – cauterization of the nevus with electric current;
- cryodestruction – freezing with liquid nitrogen;
- laser method - removal of formation using a laser;
- radio wave method - exposure to high-frequency radio waves;
- surgical method - excision of the mole with a scalpel.
Each of these methods has its pros and cons. The doctor will tell you which one to choose, taking into account your problem.
Treatment
If we are talking about simple inflammation, the specialist will prescribe products for external use that accelerate tissue regeneration. Ichthyol and salicylic ointments show good results. Frequent inflammation of a mole is an indication for its removal.
One of the methods can be used:
- electrocoagulation;
- excision with a scalpel;
- radio wave exposure;
- cryodestruction;
- removal using laser.
After surgery, antiseptic treatment of the wound surface is performed. If the area of exposure was extensive, antibiotics are prescribed as prophylaxis.
Your doctor will be able to determine the cause of the nevus change.
If a mole becomes inflamed while on vacation (this often happens after a long stay in the open sun), it is not always possible to seek help from a doctor in a timely manner.
The following measures will help you avoid unpleasant consequences:
- It is recommended to lubricate the inflamed area several times a day with medical alcohol or calendula tincture; a gauze bandage with salicylic ointment can be applied to the mole;
- At the first opportunity, you must seek qualified medical help.
Therapy will be longer if the white dot on the mole appears as a result of its malignant degeneration.
The choice of treatment methods for melanoma depends on the stage of its development and the presence of metastases. If you contact an oncologist in a timely manner, surgical removal of the tumor using one of the above methods will be sufficient. However, in case of malignant degeneration, the specialist affects not only the tumor, but also the neighboring tissue within a radius of 5 cm. Thanks to this measure, the chances of developing a relapse are significantly reduced. Additionally, immunotherapy using interferon is performed. In the most difficult cases, radiation and chemotherapy are performed.
Changes in the nevus often indicate the development of melanoma
Unfortunately, the disease often ends in death. Even with timely developments in medicine, every third patient has a poor prognosis. More than 40% of patients do not survive 5 years after diagnosis.
Preventing the appearance of white spots
To avoid the formation of light areas around the birthmark, you need to follow some recommendations.
- Avoid prolonged exposure to the sun. If you have sensitive skin or a lot of moles on your body, then you should not stay in the open sun for long. Do not go to the beach between 11:00 and 17:00. At this time the sun is most aggressive. The best time for sunbathing is in the morning or late afternoon. Be sure to apply sunscreen to your skin.
- If the mole has already turned white, cover this area of skin with clothing so that it is not exposed to ultraviolet radiation. Depigmented areas burn easily in the sun.
- Try not to injure moles, because any mechanical damage can negatively affect their condition.
Now you know that a white circle around a birthmark is harmless in most cases. But if a mole begins to bother you and cause inconvenience, try not to delay contacting a doctor. It’s better to be on the safe side than to get sick.
Possible complications and precautions
Knowing the causes and signs of the degeneration of benign formations into a cancerous tumor, you can avoid dangerous complications. Melanoma is a serious consequence. Treatment in the early stages will give positive results. If you delay visiting the hospital, the consequences will be serious and will require a lot of effort and money. If the tumor is not removed in time, it will metastasize, affecting the lymphatic system and distant organs. Removing them will not be easy. Treatment will not bring positive results, and death is possible.
You can protect yourself by following simple preventive measures:
- do not sunbathe in the sun during dangerous hours (between 11 o'clock in the afternoon and 5 o'clock in the evening);
- use sunscreen;
- visiting a solarium is not recommended;
- timely treatment of damaged nevi;
- Regular examination of all moles and spots.
If suspicious signs appear, see a doctor immediately. Vigilance is never superfluous; timely and high-quality treatment will help avoid complications.
Diagnostics
During your initial visit to a dermatologist, the doctor will conduct a visual examination of the mole and collect an anamnesis. Usually, doctors carefully analyze the condition of a mole using a dermatoscope - a special device that allows you to enlarge the neoplasm several times, as well as “see” the skin almost right through. Thanks to this, the doctor can scan what is happening in the lower layers of the epidermis and assess the risk of malignancy of the tumor.
In the future, the patient may also need other tests:
- Examination of skin scrapings.
- Blood tests.
- Carrying out a biopsy of the tumor and further histological examination of the resulting sample.
Most often, doctors can make a preliminary diagnosis after the first visit to the clinic. Therefore, you should not postpone a consultation with a dermatologist until later.