The skin disease caused by a fungus on the face is a type of mycosis of smooth skin, but has some features of external manifestations.
Mycosis of the facial skin is caused by a fungus of the genus Trichophyton, so the disease is classified as trichophytosis. The lesion does not involve the area of skin under the beard and mustache in men. The pathology is considered separately from mycosis of smooth skin, since its manifestations are often confused with pityriasis versicolor, rosacea, seborrheic dermatitis, or symptoms of lupus. Therefore, treatment for mycosis of the facial skin is prescribed by a dermatologist only after a thorough diagnosis.
The disease is quite rare. Infection occurs mainly through transmission of the pathogen:
- from animals;
- less often from a sick person to a healthy one.
At the same time, foci of infection may appear on the scalp or torso.
Mycosis of the facial skin causes not only health problems. Its signs are clearly visible and therefore cause aesthetic discomfort in the patient and surrounding people.
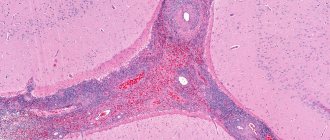
Signs of the disease are presented in the photo of facial skin mycosis:
General information
Fungal diseases are infectious diseases caused by pathogenic and opportunistic fungi.
Currently, the number of fungal infections is growing, which is associated with the expansion of risk groups and climate change. Risk groups include people with allergic conditions, malignant neoplasms, those who have undergone organ and stem cell transplants, patients with immunological diseases, those who have undergone complex operations and who have received massive antibacterial therapy. Superficial skin lesions can be caused by dermatophytes, molds and yeast-like fungi. Dermatophytes rank first in the list of causative agents of skin diseases, and they are grouped into three large genera: Trichophyton, Microsporum and Epidermophyton. Mycosis on the skin of the face (Tinea faciei) is considered a variant of mycosis of smooth skin, but is less common than mycoses of other localizations.
Most often, facial damage is caused by T. rubrum (rubromycosis disease) and T. mentagrophytes, less commonly by microsporum fungi: M. Canis and M. audouinii. Dermatophytosis of the face can be detected as an independent primary lesion, or be secondary in nature when the process spreads from primary lesions to the trunk, folds, neck or limbs. This is facilitated by concomitant pathology of internal organs, diabetes mellitus , pathology of the thyroid gland, as well as the lack of treatment for mycotic lesions. Facial mycosis caused by dermatophytes occupies a separate place in the classification - ICD-10 code B35.0. The most common yeasts that affect the skin of the face and scalp are Candida and Pityrosporum ovale yeast.
Diagnosis of fungal infection
To diagnose a fungus in the body, it is necessary to identify the clinical signs characteristic of a given disease, and then conduct a series of laboratory tests to identify the type of fungal infection (this is extremely important for further treatment).
Laboratory tests necessary to diagnose a fungal infection:
- Aspergillus fumigatus, DNA [PCR];
- Candida albicans, IgG, titer and DNA [real-time PCR];
- Analysis of vaginal microbiocenosis, including 8 indicators and quantitative DNA [real-time PCR];
- Sowing Candida spp, yeast-like fungi.
Other tests needed to diagnose a fungal infection:
- Ultrasound, which allows you to identify space-occupying formations of a pathological nature that may occur due to a fungal infection affecting internal organs.
Pathogenesis
The main location of pathogenic fungi is keratin-containing tissues (the stratum corneum of the epidermis, nails and hair), since they feed on keratin and actively multiply in these tissues. Dermatophytes penetrate the keratin of the skin using keratinolytic proteases. They also produce multiple proteases that destroy other proteins - fibrin , collagen , elastin .
The introduction of a fungus into the skin does not always cause the development of an infectious process. Thus, in the absence of skin damage, long-term asymptomatic carriage of pathogenic fungi occurs. For the development of the disease, certain conditions are necessary: viability, the number of fungi on the skin, the body’s ability to resist pathogens. Mycotic infection is resisted by the barrier function of the skin and immune . Patients with weakened immune systems are susceptible to fungal infections. Elimination of pathogens depends on the condition and function of phagocytic cells - macrophages and neutrophils. The former provide antifungal protection at the initial stages of infection, and neutrophils eliminate fungal invasion.
Having penetrated the skin, the fungus forms threads of mycelium, which penetrate into healthy areas of the skin, causing characteristic damage. If the rate of exfoliation of the stratum corneum (desquamation) is low, then the rate of growth of the fungus prevails and the infectious process spreads quickly. If the rate of desquamation exceeds that of the fungus, then the infection does not spread, since the fungus is eliminated with dead scales of the stratum corneum.
Who is at risk for fungal infection?
- People who sweat intensely;
- People whose immune systems are weakened (say, if a person is taking glucocorticoid drugs);
- Patients suffering from diabetes;
- People who work in warm and humid conditions;
- People walking barefoot in public places (swimming pools and gyms);
- People who wear poorly ventilated clothing, shoes, socks;
- People who neglect the rules of personal hygiene, use other people's towels and bed linen, wear someone else's shoes;
- Patients who have completed a course of antibacterial therapy;
- People who are in areas where the prevalence and incidence of one of the types of fungal infections is endemic.
Classification
In the classification of all mycoses, the following lesions are distinguished:
- Superficial ( dermatomycosis ).
- Deep subcutaneous lesions.
- Visceral mycoses (damage to internal organs).
Superficial mycoses are classified according to the localization of the process:
- Mycosis of the feet.
- Smooth skin of the body.
- Inguinal mycosis.
- The scalp.
- Mycosis of the hands.
- Onychomycosis (damage to nails).
- Mycosis of the face.
Facial dermatophytosis is most often found in countries with warm climates. There are two forms: classic and with deep inflammatory lesions. In the first form, the lesion is represented by flat scaly papules, the borders of which are raised and enlarged, turning into a ring-shaped lesion. The desquamation border contains elevated papules and vesicles. The merged elements occupy large areas.
Deep lesions are caused by the fungus Trichophyton verrucosum, which is transmitted from cattle. Large inflammatory foci with a raised surface and pustules appear on the skin of the face. A secondary bacterial (staphylococcal) infection is often associated. The process resolves with hyperpigmentation and scarring .
Types of fungal skin infections
Depending on the pathogen, the symptoms of mycosis may vary slightly in each individual clinical case. In order to verify the preliminary diagnosis, additional tests are prescribed. During the latter, as a rule, the direct causative agent of the disease is identified. Subsequently, based on the data obtained, one of the following diagnoses is made:
- Trichophytosis (ringworm) - the causative agent of the disease is fungi of the genus Trichophyton. As the latter penetrates into the deep layers of the dermis, bright red spots appear on the patient’s facial skin. The affected areas peel off and become covered with multiple nodules.
- Pityriasis versicolor (varicolored) - the pathology is caused by the yeast-like pathogenic fungi Malassezia furfur. Against the background of the disease, the infected person develops pink scaly spots, which subsequently increase significantly and merge into a single pathological focus.
- Seborrheic dermatitis - this type of lesion occurs due to infection with fungi of the genus Malassezia furfur. Focal manifestations of this disease are located mainly in places of greatest accumulation of sebum. In some cases, pathological formations are covered with a hemorrhagic crust. Seborrheic dermatitis is accompanied by itching.
- Rubromycosis - the causative agent of this type of mycotic infection is fungi of the genus Malassezia rubrum. With this form of lesion, large red spots appear on the patient’s skin, surrounded by a ridge of papules.
- Microsporia – this type of mycosis is caused by Microsporum. The disease is characterized by large red spots, above which rises a ridge covered with multiple blisters.
- Candidiasis is caused by a yeast fungus of the genus Candida. Along with the skin, the pathogen can infect mucous membranes. Thus, painful blisters filled with serous fluid are often found not only on the skin, but also in the patient’s mouth.
Causes
Fungal infection occurs:
- Zoophilic fungi Microsporum and Trichophyton in direct contact with animals (cats, dogs, cattle). Animals of any breed are susceptible to infection. Most often, the lesion is caused by Trichophyton, rarely by M. canis. Microsporum canis is spread by cats. Trichophytosis is common among horses, mice, rats, and pigs. There are cases of Trichophyton Arthroderma infection from guinea pigs. Trichophytes infect any area of the skin causing acute infections.
- Through infected objects, instruments and skin flakes.
- With autoinoculation - transfer of the pathogen from other foci of dermatophytosis (torso, limbs, scalp).
Most often, microsporia occurs in children. Infection occurs in the summer during contact with sick cats, and appears in the autumn when returning from vacation. Facial dermatophytosis is very common in athletes (wrestlers) and is caused by Trichophyton tonurans. Dermatophytosis of the beard area is caused by the fungi Trichophyton mentagrophytes, Trichophyton rubrum, and rarely Microsporum canis.
How does fungal infection occur?
Infection with fungal skin diseases can occur in two ways:
- Straight way. It occurs upon contact with an infected person, animal, plant, or soil.
- Indirect path. Infection occurs through objects used by a sick person or animal.
There are factors that create favorable conditions for fungal infection:
- Decreased immunity.
- Severe and chronic infections.
- Skin injuries.
- Frequent and prolonged stress, chronic fatigue, weakening of the body.
- Long-term use of antibiotics in large dosages. These drugs destroy bacteria that are in a competitive relationship with fungi.
- Long-term use of hormonal drugs and other drugs that affect the immune system.
At CELT you can consult a dermatologist.
- Initial consultation – 3,500
- Repeated consultation – 2,300
Make an appointment
Symptoms
You can think about a fungal infection of the skin of the face if you have any rash with scales. Signs of inflammation may be absent or mild in dermatophyte infections caused by Trichophyton rubrum. Clinically, mycosis of the face can manifest itself as typical round pink spots surrounded by an edematous ridge of vesicles and pustules. These spots increase along the periphery, and their central part is covered with scales (this form is called circinar).
The lesions are most often localized in the area of the lower lip and chin. Hair in the lesion rarely becomes infected. In atypical forms, edematous erythema appears with or without peeling, which is accompanied by itching and burning. It is also possible to develop an infiltrative-suppurative form with the appearance of bluish-red nodes with a bumpy surface. Merging, numerous pustules form abscesses. In this case, the hair in the lesion is affected and can be easily removed without pain.
Microsporia
It appears as erythematous plaques with clear boundaries, which are often covered with gray-white scales. Increasing in size, the plaque takes on a ring-shaped shape, resolves in the center and has a raised red ridge along the periphery. Sizes range from 1 to 8 cm in diameter.
Photo of fungus on the face (microsporia)
Most often, plaques are located asymmetrically. They are localized on the cheeks and chin, less often on the forehead, nose and near the eyes. The patient may complain of itching, and there is also increased sensitivity to sunlight. Microsporia of the face is similar in appearance to the rash of lupus erythematosus , eosinophilic granuloma of the face and lymphocytic infiltration.
Rubrophytia
Caused by the fungus Trichophyton rubrum. Lesions of smooth skin with it have any localization, including the face, which is less common than lesions of large folds, buttocks and legs. In typical cases, rubromycosis appears as pink or bluish spots that have rounded outlines and are clearly demarcated from unaffected skin. Small scales are visible on the surface of the spots, and a ridge of papules, vesicles and crusts forms along the periphery.
The spots are small, but increase in size due to peripheral growth. Over time, the inflammation subsides, the blisters disappear, and the peripheral ridge becomes flat. The spots become bluish and brownish in color.
Fungus on eyelids
Fungal blepharitis is a fungal infection of the skin of the eyelids, caused by the spread of the pathogen from neighboring lesions on the face. Most often these are yeast fungi Malassezia furfur and Candida. Deficiency of T-cell immunity predisposes to the development of infection with yeast-like fungi. It is most likely that Candida fungi are transferred from other areas to the eyelids by hand. There are also cases of fungal blepharitis after corneal transplantation. In this case, it may be due to long-term use of corticosteroids.
Characteristic symptoms are swelling of the eyelids, the skin of the eyelids is covered with scales, under which there may be erosion. The process often extends beyond the skin of the eyelids to the area around the eyes.
Candidiasis
Isolated candidiasis of the lips spreads to surrounding tissues - the corners of the mouth and the skin of the face. Candidal angular cheilitis occurs when oral candidiasis and infection of the corners of the mouth. This is facilitated by saliva flowing into the corners of the mouth.
This pathology affects both corners of the mouth. The disease begins with redness and itching. Then cracks form in the area of the corners, painful when opening the mouth, touching and moving the lips. Erosion forms on the cracks, along the edge of which the epidermis peels off. With candidiasis, erosions have a whitish coating. This process enters the chronic stage.
Any localization of skin candidiasis begins with persistent itching. A main focus of bluish-red color with a moist, shiny surface appears, and screenings appear in the form of small superficial blisters and pustules. Surface erosions and cracks form at the source. The surface of the erosions is red, bordered by a white rim.
Fungus in the nose
Also common are ENT mycoses, the causative agents of which are opportunistic fungi (Candida and Aspergillus). These conditions occur when immunity . There are not only fungal pharyngitis and otomycosis (ear damage), but also mycoses of the nose (occur in 14% of cases) and paranasal sinuses. In more than half of patients suffering from chronic sinusitis , it is caused by fungi. In this case, the mycelium grows inside the sinus cavity and does not grow into its mucosa. The disease develops slowly - from the moment the inflammation begins until the initial symptoms appear, it takes from two to 15 years.
Symptoms of a fungus in the nose include constant nasal congestion and heavy discharge, which depend on the stage of the process. Signs of fungus in the nose also include severe soreness of the nasal mucosa. For fungal infections of the nose and sinuses, systemic therapy is prescribed - Intraconazole 100 mg per day or Medoflucon 50 mg per day are taken orally. The effectiveness of both drugs is 93%.
Treatment
The essence of therapy for mycotic skin infections, first of all, comes down to the speedy elimination of the pathogenic agent from the affected area. In the background is the elimination of factors leading to infection. In view of this, in the treatment of mycoses, the use of systemic and local medications with an antifungal effect is justified. Regarding the former, it is important to say that the dosage and regimen of their use is determined individually for each patient.
Oral antimycotics are extremely toxic to the liver, so their use should be under strict medical supervision. In addition to systemic therapy with tablets, local agents are mandatory when treating fungus. Special ointments, creams and other medicinal formulations contain specific substances that are harmful to the fungus. Simultaneously with the treatment of mycosis, it is extremely important to take all measures necessary to strengthen the immune system:
- get rid of chronic diseases;
- maintain a sleep-wake schedule;
- lead an active lifestyle and adhere to the basics of proper nutrition;
- take vitamins and probiotics.
- Chicken and potato pie: recipes with photos
- How to remove wrinkles above the upper lip - products and procedures for women
- How soon after training can you eat and drink?
Drug treatment
Fungal diseases of the facial skin require effective treatment, which entirely depends on the correct diagnosis of the pathogen based on scraping tests of the patient’s skin flakes and visual examination. In the absence of adequate therapy, the pathogen begins to multiply unhindered, resulting in the disease taking a chronic course. In most cases, to combat a fungal infection, a comprehensive treatment regimen is developed using the following groups of drugs:
- multivitamin complexes;
- antihistamines;
- systemic drugs with fungicidal and fungistatic effects;
- external antifungal agents;
- enzymes and probiotics.
Systemic therapy for fungal infections involves oral administration of antifungals. The use of the latter promotes selective accumulation of the drug in the affected area in a concentration necessary to effectively suppress the development of the pathogen. For the purpose of systemic influence on a foreign agent, the following drugs are mostly used for internal use:
- Nizoral - the active ingredient of the drug is ketoconazole. Nizoral has a fungicidal, fungistatic effect. The medicine acts against dimorphic, yeast and other fungi. The drug is indicated for systemic lesions, mycoses of soft tissues and skin. The course of therapy is determined individually in each specific case. The average dosage for adults is 200 mg per day. Limitations for taking Nizoral include renal or liver failure. Side effects of the drug include hepatitis, paresthesia, and abdominal pain.
- Lamisil - the active component of the drug is terbinafine. This substance suppresses the early stage of sterol biosynthesis in the pathogen cell, which results in the death of the latter. Lamisil has a wide spectrum of action, so it is used for any type of fungal infection. For adults, the drug is prescribed 250 mg once a day. To treat mycosis caused by yeast, it is recommended to take the tablets for 2-4 weeks. The fight against other pathogens lasts about 2 months. The drug is contraindicated in persons with liver and kidney pathologies. Taking Lamisil can cause:
- headache;
- hepatitis;
- bile duct dysfunction;
- cutaneous lupus erythematosus;
- joint pain;
- dyspepsia.
Ointment
Complete treatment is impossible without the use of local drugs. Modern antimycotic ointments effectively eliminate inflammation and pathogenic flora, while providing a complex effect on the lesion. Local therapy for facial skin mycosis involves long-term use of the following antifungal agents for external use:
- Miconazole - this drug has a detrimental effect on almost all types of such infections. Miconazole ointment destroys pathogenic microorganisms by suppressing the production of ergosterol. The drug is indicated for lesions of the skin, nails, secondary infection with streptococci and staphylococci. Miconazole must be rubbed into the affected areas twice a day for 4 weeks. The ointment should not be used if you are intolerant of its individual components. The use of Miconazole, as a rule, does not cause side effects.
- Clotrimazole - the drug is an antimycotic with a wide spectrum of activity against most types of fungi. Clotrimazole inhibits the growth and reproduction of the pathogen by disrupting the synthesis of ergosterol. Indications for the use of the ointment are mycosis of the facial skin, pink and pityriasis versicolor. In order to eliminate the pathogenic agent, Clotrimazole is recommended to be applied to the affected area 2-3 times a day for 3 weeks. The drug should not be used if you are hypersensitive to its individual components. The use of ointment can cause:
- burning;
- itching;
- redness;
- swelling.
Antifungal creams
The main criteria for choosing a particular local antimycotic agent are the spectrum of action of the drug and its effectiveness against a specific pathogen. Today, the pharmacy chain offers consumers a huge selection of a wide variety of drugs for external use. Taking into account the above conditions, it is considered optimal to purchase one of the following antifungal creams:
- Travogena - used when the process is localized in the folds of the skin and the area of the external genital organs, mycoses of the feet. The drug suppresses the growth and development of fungus on the face, causing its death. Travogen is applied to the affected area once a day for 2-3 weeks. The drug should not be used by persons with individual intolerance to its individual components. In most cases, Travogen does not cause any side effects.
- Mycoqueta - suppresses the synthesis of ergosterol, phospholipids and triglycerides, which ultimately leads to the death of the fungus. Mycoket cream is indicated for dermatomycosis of smooth skin, athlete's foot and hands, seborrhea, pityriasis versicolor. The drug is applied to the affected area once a day for 2-4 weeks. The cream should not be used if you are hypersensitive to ketoconazole. The use of the drug can cause a number of side effects such as burning, itching, and swelling.
- Ecodaxa - the active ingredient of this drug stops the synthesis of ergosterol and leads to the destruction of the infection. Ecodax cream is used for mycoses and mixed fungal-bacterial skin infections caused by microorganisms sensitive to the drug. The product is used twice a day. The course of treatment lasts about 4-6 weeks. Ecodax is contraindicated in persons with hypersensitivity to econazole. The use of the cream may cause side effects such as irritation, itching and hyperemia of the skin.
Traditional methods
In a situation where the use of medications does not provide a lasting therapeutic effect, natural methods of combating ailments, proven by many generations, can help. Remember that decoctions of medicinal herbs, any solutions and other means should be used only after consultation with a specialist. Meanwhile, the most effective folk remedies are considered to be:
- Garlic ointment. The product must be crushed and mixed with a small amount of butter. Then the finished composition should be applied to the affected area of the skin. After 30-40 minutes, the garlic ointment should be washed off with warm water. It is recommended to repeat the procedure once a day until the condition improves.
- Honey water. This remedy helps to quickly eliminate yeast fungus on the face of adults and children. For this type of lesion, you should dilute a teaspoon of honey in 100 mg of clean water. The resulting solution must be used to treat existing lesions 3-4 times a day until the disease is completely resolved.
Tests and diagnostics
The diagnosis is made based on examination of the patient and laboratory data:
- Microscopy of material is a quick method of preliminary diagnosis. The materials used for laboratory examinations are hair, scales, skin scrapings, and crusts, which are taken from areas that have not been treated. Test preparations are pre-treated with potassium hydroxide (KOH, which is why the test is called a KOH test). With a microscopic examination, a laboratory technician can see and distinguish groups of fungi: dermatomycetes, yeast molds and yeast-like fungi. In scrapings, dermatophytes are represented by thin, straight and almost non-branching mycelium. M. furfur is detected as round cells (diameter 3–8 μm) that are collected in clusters, and curved banana-shaped mycelial hyphae can also be detected. Fungi of the genus Candida are represented by budding yeast cells and pseudomycelium in the form of a branching chain of cells. In most cases, lichen versicolor is diagnosed only by microscopy of the specimen, since culture of the material is often inconclusive.
- Cultural research - inoculation on a medium with subsequent identification of the species.
- For hair microsporia and pityriasis versicolor, an examination is carried out under the rays of a WOOD lamp - the lesions have a characteristic glow. With microsporia, the lesions have a bluish-green glow. With pityriasis versicolor, there is a copper-orange glow and even subclinical forms of infection are detected. The examination is carried out not only for primary diagnosis, but also to monitor the healing process.
In children
The main sources of infection of children with zoophilic fungi are stray cats and kittens. The latter are more susceptible to the disease because they have an imperfect immune system and a developed delicate undercoat, which is a breeding ground for microsporum. Microsporia in children is called “feline” lichen. The main contingent consists of children aged 5 to 14 years. The peak incidence occurs in August-October. Microsporia spreads quickly when the pathogen is introduced into schools, sports clubs and kindergartens. Infection from a sick child is possible through household items, a shared towel. The incubation period of zoonotic microsporia is 5-8 days. Anthropophilic pathogens of microsporia (M. ferrugineum) are transmitted through household items and from person to person.
A fungus on a child’s face manifests itself in small, coin-shaped, multiple lesions 1-2 cm in size. They tend to merge. Visually, these foci are difficult to distinguish from foci of trichophytosis . The difference is that with microsporia there are a larger number of foci, vellus hair, eyebrows and eyelashes are more often affected. Microsporidae can also occur - these are allergic rashes, like nodules.
Manifestations of anthroponotic microsporia are similar to superficial trichophytosis. The lesions have clear boundaries and merge, forming bizarre outlines. The primary elements in the lesions are bubbles or nodules, and the secondary elements are crusts. In the classic version, two lesions are formed in the shape of a “ring within a ring”.
Photo of a fungus on a child’s face
With microsporia and trichophytosis, lesions are often found on the head. These are large, round, scaly patches of baldness. The hair within the lesion is broken off and, with microsporia, protrudes several millimeters above the skin; with trichophytosis, it breaks off at the level of the skin and is visible as a black dot (“stump”). Inflammatory phenomena on the scalp are not expressed. Only bestial pathogens in some cases can cause an infiltrative-suppurative form, in which the lesion protrudes above the skin and is covered with purulent crusts. In case of complications, the child may be hospitalized. If the diagnosis of microsporia and trichophytosis is confirmed, the patient is isolated for 35 days. Contact persons during this period are examined by a doctor. The fireplace is disinfected.
Prevention
- Prevention of skin candidiasis involves taking antifungal drugs with long-term or frequent use of antibiotics, hormones, and immunosuppressants. Taking antifungal drugs orally ( Natamycin , Fluconazole ) should continue throughout the main course of antibiotic treatment.
- For trichophytosis, which is transmitted by animals, it is important to carry out disinfection in the habitats of stray animals and treat sick animals. For trichophytosis, which is transmitted from sick children or adults, it is necessary to identify the source of infection, isolate it, and disinfect it in schools, kindergartens and hospitals.
- It is necessary to carefully examine the fur of pets for the presence of disease and promptly treat them.
- Avoid contact with stray animals.
- After playing with animals, you should wash your hands thoroughly.
- Improve the living conditions for children in health institutions and carry out regular disinfection.
- Carrying out disinfection measures in sports complexes, hairdressing salons, hotels and saunas.
- Mandatory processing of professional tools in hairdressing salons.
What are the signs of skin fungus? When should you visit a dermatologist?
Fungal skin infection can be suspected if the following signs are present:
- peeling;
- increased skin dryness;
- redness, swelling - signs of inflammation;
- pain, itching;
- bubbles;
- cracks.
If these symptoms do not go away on their own, then you should see a dermatologist for timely treatment.
List of sources
- Kubanova A.A., Potekaev N.S., Potekaev N.N. Guide to practical mycology. – Moscow, Financial Publishing House “Business Express”, 200 p.
- Sergeev A. Yu., Sergeev Yu. V. Fungal infections. Guide for doctors. M.: BINOM-Press, 2003. 440 p.
- Clinical dermatovenerology. Guide for doctors in 2 volumes / Ed. Yu. K. Skripkina, Yu. S. Butova. M.: GEOTAR-Media, 2009. T. 1, 720 p. T. 2, 928 p.
- Potekaev N. S. Microsporia in adults / N. S. Potekaev, L. R. Plieva, S. V. Shkrebets // Clinical dermatology and venereology. - 2008. - No. 4. - P. 19–21.
- Sergeev Yu.V., Shpigel B.I., Sergeev A.Yu. Pharmacotherapy of mycoses. M.: Medicine for everyone, 2003. – 200 p.