Urticaria - symptoms and treatment
Diagnosing urticaria does not require specific laboratory diagnostics, although identifying the causes of the disease may require it.[3]
First of all, you need to see an allergist-immunologist as soon as possible. If there are no rashes at the time of the visit, try to provide the doctor with photographs of the rashes/swelling for maximum information (provided that the clinical manifestations were not severe and did not require emergency assistance during photographic recording).
During the appointment, the allergist-immunologist will collect a detailed medical history, life history, allergy history, and conduct a physical examination (examination, measurement of blood pressure, heart rate, respiratory rate, body temperature, listen to the heart and lungs, palpate peripheral lymph nodes, abdomen). In most cases, this diagnostic complex will be sufficient to make a diagnosis and select therapy.[2]
In more than 90% of cases, acute urticaria resolves within two weeks and does not require special examination, unless the triggering agent is identified.[1]
What tests are done for urticaria?
If there are frequent relapses of acute urticaria or there is a chronic disease, you will need:
- general blood test with leukocyte formula and ESR calculation;
- study of some biochemical blood parameters;
- examination for the presence of viral hepatitis B, C;
- conducting provocative tests (ice cube for suspected cold urticaria, hot heating pad for thermal urticaria, water compress for aquagenic urticaria, exercise test for suspected cholinergic urticaria, etc.);
- determination of antibody levels to thyroid peroxidase and thyroglobulin with an intradermal test with autologous serum;
- scratch tests with non-infectious allergens and/or the presence of specific immunoglobulin E in the blood for any allergen.[2]
If further diagnostic search is necessary, it would be advisable to:
- Ultrasound of internal organs (thyroid gland, abdominal cavity, pelvis);
- FGDS or fluoroscopy of the stomach;
- X-ray examination of the chest organs and paranasal sinuses;
- virological or bacteriological examination for the presence of infectious agents;
- analysis of the level of antibodies to the Cag A protein of Helicobacter, Giardia, helminths;
- rheumatic tests (ANF, AT to DNA, CRP);
- studies of complement components C3, C4, etc. [3]
An important diagnostic test in patients with urticaria is skin testing.[9] They are informative in patients with atopic urticaria and negative in patients with pseudoallergic urticaria (subject to the timing of the tests and the accompanying preparation for testing).[5] The bilirubin test against the background of an elimination test is also informative (carried out in a hospital, therapeutic fasting is prescribed with the intake of only water, showers and cleansing enemas). If the result of elimination, reduction or relief of symptoms is positive, the allergic genesis of urticaria is confirmed. In patients with allergic urticaria, the bilirubin level is reduced or within normal limits, in patients with pseudoallergic urticaria it is increased.[4]
Treatment of allergic urticaria in adults
Allergic urticaria is a dermatological reaction to exposure to a factor with a protein structure.
The disease is characterized by increased immune reactivity and is accompanied by specific rashes similar to nettle marks. In 40% of adult patients, the condition is combined with symptoms of angioedema1. It is characterized by isolated swelling of a part of the body with the formation of dense edema affecting the subcutaneous fat and dermis of the skin. Urticaria affects approximately 15-25% of the population, and in 30% the disease is chronic4.
The disease requires complex treatment aimed at eliminating the allergen from everyday life and blocking the mechanisms that provoke the formation of the rash. Ignoring the problem is dangerous, as the condition progressively worsens, up to anaphylactic shock. In addition, this type of allergy significantly worsens the quality of life and can cause psychological problems and neuroses.
Laboratory and instrumental diagnosis of urticaria
In addition to general clinical studies, tests should be performed to look for concomitant somatic pathology. Often, patients in this category have diseases of the gastrointestinal tract and hepatobiliary system of infectious and non-infectious origin, autoimmune diseases, including autoimmune thyroiditis, which is widespread today. At the same time, examination results often lie within the reference values, and it is difficult to associate the appearance of urticaria with any concomitant pathology.
Differential diagnosis is carried out with a number of diseases, such as urticarial vasculitis, Dühring's dermatitis herpetiformis, erythema multiforme exudative, contact urticaria, as well as blood-sucking insect bites.
Drug treatment of allergic urticaria
Taking medications is necessary for both acute and chronic cases. The following groups of drugs are used:
- Antihistamines. Cetrin is a second-generation drug that blocks histamine receptors, helping to eliminate the symptoms of allergic urticaria. The drug is used once a day, as it is effective for 24 hours. The drug begins to act within 20 minutes after administration2.
- Enterosorbents. Eliminates the allergen from the gastrointestinal tract, which is why it is not absorbed into the blood.
- Corticosteroids. Taken in severe cases of allergies as prescribed by a doctor and as an emergency aid to relieve Quincke's edema1.
Treatment of the disease in adults should be comprehensive, aimed at completely eliminating irritating factors. Antihistamines are drugs indicated for any form and severity of an allergic reaction.
New trends
The effectiveness of treating urticaria with alternative groups of drugs is currently being studied. Among them: antidepressants, androgens, slow calcium channel blockers (nifedipine), M-anticholinergic blockers, sulfasalazine, methotrexate, colchicine.
The use of plasmapheresis and phototherapy in patients with solar urticaria is actively discussed. Separately, it is worth dwelling on the issue of the use of biological agents. The idea of binding and inactivating molecules involved in immune responses has always seemed extremely attractive in the search for a cure for hives. The appearance in practice of monoclonal antibodies (MAbs), which make it possible to solve this problem with high specificity and selectivity for target molecules, gave rise to a number of biomedical studies that studied the possibility of using MAbs for the treatment of immune-mediated diseases, including allergological diseases.
Currently, mAbs against immunoglobulin E, the drug omalizumab, are registered in Russia. The drug binds to IgE, blocks its interaction with receptors on mast cells, which prevents their subsequent degranulation; there is also a decrease in the number of IgE receptors on the surface of basophils. Omalizumab, originally used to treat severe atopic asthma, later showed its effectiveness in the treatment of chronic urticaria. However, scientists do not rest on this and continue to search for new biological agents to treat different types of urticaria.
Causes of urticaria in adults
Allergic rashes are caused by the following environmental factors:
- Food (seafood, nuts, chocolate and other products containing cocoa, honey, eggs, dairy products, citrus fruits, exotic fruits, strawberries and other berries, various herbs for herbal tea);
- Medicines (penicillin antibiotics, acetylsalicylic acid and other NSAIDs, B vitamins, vitamin C, non-narcotic painkillers and any other medications in the form of individual intolerance);
- Insect bites: bees and wasps;
- Animal fur, saliva (by inhalation, bites or scratches);
- Plant pollen (rarely manifests itself as urticaria);
- Mold.
Sometimes the factor that caused the allergy is obvious due to the direct connection between the appearance of the rash and its exposure. For example, after eating a certain product. In some cases, it is not possible to determine the allergen on your own, so you have to conduct specific studies.
Traditional therapy
How to treat hives? The first step is to eliminate the causes and triggers of the disease if possible. Refusal of medications that provoke rashes, an attempt to avoid the influence of provoking physical factors, as well as adherence to a hypoallergenic diet can reduce the frequency of relapses of the disease, but all this has rather low effectiveness without drug therapy.
An important task is the rehabilitation of foci of chronic infection and correction of concomitant somatic pathology. Sometimes these measures are enough to prevent relapses.
The main drugs for urticaria, with which drug therapy begins, are, of course, H1-histamine receptor blockers. According to the recommendations of the World Allergy Organization, therapy should begin with second-generation antihistamines.
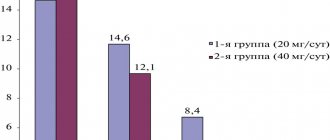
If symptoms persist for 2 weeks, then it is permissible to increase the dose to four times and continue taking it for up to 4 weeks. A sedating H1 blocker may be prescribed at night. If ineffective, it is recommended to change the drug or add antileukotriene drugs. During exacerbations, a short course of systemic glucocorticosteroids (3–7 days) is acceptable.
If manifestations of urticaria/angioedema persist, the issue of switching to 2nd line drugs must be resolved - glucocorticosteroids, immunosuppressants (cyclosporine), monoclonal antibody drugs (omalizumab). In the treatment of urticaria pigmentosa, as well as urticaria caused by physical factors, the stabilizer ketotifen is used mast cell membranes.
Angioedema (with the exception of hereditary forms associated with defects in the complement system or kinin system) is treated according to the same principles. In case of life-threatening conditions associated with the risk of asphyxia (swelling of the larynx, tongue), emergency treatment with the administration of adrenaline is required; emergency intubation or tracheostomy may also be necessary.
Forecast
Often, an episode of acute urticaria may be the only one in a patient's life. If the patient is less fortunate and the allergy becomes chronic, then spontaneous remission can be expected in 50% of cases.
Potentially life-threatening are laryngeal edema with urticaria and the acute form of the disease with anaphylactic reactions. For patients with cold urticaria, swimming in cold water can be fatal due to asphyxia or systemic reactions with a drop in blood pressure.
Anamnesis
Given the ephemeral nature of urticaria rashes, it is extremely important to properly collect anamnesis. The doctor must understand whether it is urticaria, what provokes it and what mechanisms support it. Therefore, you should pay attention to the following points:
- description of the elements and associated sensations (itching, burning, pain);
- life expectancy of elements and the presence of secondary changes - hyperpigmentation, erosions, crusts, etc.;
- the cyclicity of the appearance of elements, the duration and frequency of the disease. For women, it is worth paying attention to the connection with the phases of the menstrual cycle;
- triggers, including medications, food intake, insect bites/stings, as well as physical factors and stress;
- previous therapy and its effectiveness;
- presence of allergic diseases in personal and family history;
- the presence of concomitant somatic pathology, including those associated with chronic urticaria, infectious diseases, autoimmune diseases, non-infectious chronic inflammatory diseases, especially involving the gastrointestinal tract, paraneoplasia;
- professional activity/hobby.
Classification, types of urticaria and pathogenesis
A wheal is a local swelling of the dermis, usually characterized by itching, limited swelling of the skin, and hyperemia.
The blister completely resolves within a relatively short time. In addition to dividing urticaria into acute and chronic, there is a division into types depending on the factors that provoke exacerbation. Different forms of urticaria can occur simultaneously in the same patient. In addition, a number of conditions have been described that were once classified as urticaria, but are not such, or contain urticaria/angioedema as one of the symptoms of the clinical picture:
- Urticaria pigmentosa (mastocytosis) is a disease caused by the accumulation and proliferation of mast cells in tissues.
- Polymorphic skin rashes, including urticarial ones, are characteristic.
- Urticarial vasculitis - vasculitis with skin rashes - nodules and blisters, angioedema. After resolution of the elements, hyperpigmentation may be observed.
- Nonhistaminergic angioedema, such as hereditary angioedema, often associated with defects in the complement or kinin system.
- Exercise-induced anaphylaxis/urticaria.
- Cryopyrin-associated periodic syndrome (in the clinic there is an urticarial rash, fever, arthralgia or arthritis, increased fatigue and headaches. Includes familial cold autoinflammatory syndrome (Muckle-Wells syndrome (with the development of sensorineural hearing loss and renal amyloidosis) and infantile multisystem inflammatory disease .
- Schnitzler syndrome is a chronic urticaria with monoclonal IgM gammopathy.
- Gleich syndrome is episodic angioedema with eosinophilia.
- Wells syndrome is a granulomatous dermatitis with eosinophilia.
The key point in the pathogenesis of urticaria is the release of mast cell mediators (histamine, serotonin, chemotactic factors, arachidonic acid metabolites) and the development of their effects: vasodilation, increased permeability of the vascular wall with the appearance of edema and hyperemia; smooth muscle spasm; phenomena of itching and burning.