A benign neoplasm, which is formed from the synovial (articular) membranes, is called “hygroma” or “tendon ganglion”. This bulge inside is filled with mucus and fibrin protein strands. The tumor can appear on any joint (fingers, hands, feet).
Hygroma on the finger is one of the most unpleasant types of pathology. As a rule, the formation appears near the distal joints between the phalanges or in the area of the flexor muscles. The lump looks unsightly and causes pain. If left untreated, the mobility of the joint worsens and the nail becomes deformed.
What is Dupuytren's disease
The name of the disease comes from the name of the surgeon Guillaume Dupuytren, who first described the disease. The word "contracture" means loss of joint mobility, that is, they cannot be bent or straightened. Needless to say that this greatly affects the quality of life?
In Dupuytren's syndrome, contracture occurs due to fibrous degeneration of the palmar aponeurosis - a wide tendon plate made of dense collagen and elastic fibers. As a rule, the disease affects the ring, middle and little fingers.
The fingers are firmly bent towards the palm, and various procedures are prescribed to straighten them. Unfortunately, this does not solve the problem: sooner or later the disease returns and affects new areas.
In addition, a person with Dupuytren's syndrome loses the ability to fine motor skills; in rare cases, the pathology is accompanied by unpleasant sensations and itching. But most often the process is painless and affects men over 40 years of age, and much less often women.
According to many experts, Dupuytren's contracture syndrome is hereditary and depends on the presence of a special gene. However, if your relative suffers from the disease, it is not a death sentence for you: many carriers of palmar fibromatosis (another name for the disease) never encounter it in their entire lives.
Symptoms
A synovial cyst is a dense, elastic formation with a smooth surface in the shape of a ball. The tumor shell is attached to the surrounding tissue, so it does not move. But sometimes during palpation you can notice that the growth moves.
When you feel the cyst, you may feel clots, cholesterol crystals, and “rice bodies” inside. They are quite mobile, often changing their position. Usually, when you press on the tumor, there is no pain or minor discomfort.
Reference. If painful sensations occur during palpation, this indicates that the pathology has become chronic. The formation increases gradually; at the early stage, there are no pronounced unpleasant sensations.
Hygroma on the finger has the following external signs:
- spherical shape, size - about 5 cm, sometimes more;
- the surface of the cyst is elastic, smooth;
- when pressing, a slight nagging pain appears in the area of the damaged joint;
- the skin over the tumor is thick and rough;
- During the inflammatory process, the skin turns red.
Symptoms depend on the stage of the pathological process: at first there are no pronounced signs, and in advanced cases they are clearly expressed. Clinical manifestations of hygroma (early stage):
- tumor size – from 5 mm;
- the cyst is inactive;
- the growth is soft, elastic;
- there are no painful sensations;
- the skin over the capsule is smooth and even.
The hygroma on the finger is practically invisible. At first, the tumor does not affect surrounding structures and is not accompanied by other pathologies.
Symptoms of an advanced stage of pathology:
- growth size – from 10 cm;
- when palpated, the tumor practically does not move;
- the cyst is dense and hard;
- nagging or sharp pain, which sometimes radiates to the arm;
- the skin over the cyst turns red, becomes rough, rough.
The hygroma on the finger is clearly visible, as its size has increased. It compresses the surrounding nearby joints, nerves, tendons, and blood vessels. The pathology is accompanied by limited mobility in the affected joint, numbness, tingling, redness of the skin, inflammatory, purulent process.
Types of Dupuytren's contracture
According to the location of the lesion, Dupuytren's fibromatosis occurs:
- palmar;
- finger;
- mixed.
Patients often complain of a feeling of stiffness, fatigue of the hand, funnel-shaped deformity, as well as the presence of a dense scar, sometimes fused to the skin.
According to the nature of development, the syndrome can be:
- Primary. It lasts for 10 years in a person over 50.
- Secondary. It fully manifests itself in 3–5 years; the patient’s age is approximately 45.
- Mixed. Progresses over a year and a half, the patient is usually no older than 35 years.
- Malignant form. Dupuytren's contracture can occur in children with pronounced heredity and develops very quickly. The entire aponeurosis is affected, accompanied by disease of the plantar aponeurosis and the aponeurosis of the penis.
Causes of warts on the palms
All warts, without exception, are a consequence of human infection with the papilloma virus, which has about 120 varieties. The direct cause of the appearance of warts on the palms is HPV types 2 and 4.
In this case, infection can occur both through contact with a carrier of the viral agent, for example, during a handshake, and through shared objects.
Being in the body in a latent (inactive state), the papilloma virus may not manifest itself in any way until a sharp weakening of the body, which is usually associated with a decrease in immunity. At the same time, the prevalence of localization of warts in the palm area is quite understandable. Hands are most often exposed to microtrauma, damage and disruption of the integrity of the epidermal covers, which also contributes to the penetration of the virus into the body. In addition, it is the hands that usually come into contact with the contaminated surface.
Causes of Dupuytren's contracture
Despite the fact that the disease has been known for several centuries (the doctor himself lived in the 19th century), the exact causes have not yet been identified. There are only speculations: supporters of the traumatic theory believed that the syndrome develops with serious damage to the palmar aponeurosis. Dupuytren, in describing the disease, suggested that it develops in people “who are forced to squeeze the fulcrum in their hand for a long time.”
In modern medicine, a whole list of possible reasons has been added to this:
- concomitant diseases such as diabetes, epilepsy, etc.;
- age-related changes in the structure of tissues - if at the age of 40 men suffer from Dupuytren's contracture of the palms more often, then by the age of 80 both women and men are equally affected by this disease;
- bad habits: such as alcoholism or smoking;
- gender;
- type of employment - if the work involves heavy loads on the hand, the likelihood of the syndrome increases;
- hand injury;
- cervical osteochondrosis;
- atherosclerosis;
- obesity;
- decrease in male sex hormones.
All this, according to orthopedists, can provoke diseases in the carrier of the gene. In addition, it is important to note that so far only the northern peoples of the Caucasian race have encountered this problem; nothing similar has yet been noticed among other nationalities.
Reasons for the appearance of compaction
Neoplasms appear at any age. Some varieties are more common in women, others in men. Depends on what reason influenced the growth of the tumor. This may be hard physical monotonous work, disruptions in the hormonal system, degenerative processes in soft tissues.
Treatment will depend on the etiology of the disease . To correctly make a diagnosis, it is necessary to conduct an examination, which includes examining the hand, talking with the patient, and taking tissue samples for histological examination. An important factor is a biochemical blood test for hormones.
Hygroma
Hygroma is a benign tumor, inside of which there is serous fluid . Appears due to excessive physical exertion, constant stress, and occupational injuries.
Treatment is only surgical , although there are cases of spontaneous disappearance of hygroma. This happens when a person reduces stress, increases immunity, and the body copes with the problem itself.
Valeria
General doctor
Ask a Question
As a result of injury or bruise, the capsular sac containing fluid may burst, possibly causing suppuration of the soft tissues. It is not recommended to deliberately injure your palm in order to get rid of the lump. Moreover, after crushing the hygroma, a lump with two or three capsules instead of one may appear in its place.
Hygroma often occurs in people who are prone to joint diseases . The disease is typical for athletes, as well as those who work a lot at the computer and spend the whole day in muscle tension.
To treat hygroma, you must contact a surgeon . He will perform the operation under local or general anesthesia and efficiently remove the tumor so that there is no relapse.
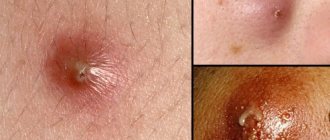
Atheroma
Atheroma occurs in people of any gender and age. It occurs due to blockage of the sebaceous gland .
Inside it there is a thick yellow content, similar to a purulent plug. This is a secretion from the sebaceous gland that cannot come out through the ducts. The danger of atheroma is that inflammation can begin with the formation of purulent masses in the subcutaneous tissue. This occurs when the duct ruptures.
If the sebaceous gland duct is not released, the lump will begin to grow. Eventually it will have to be removed surgically.
Atheromas are often multiple and located side by side on any area of the skin. This is a mobile neoplasm, painless before the onset of the inflammatory process. This type of tumor is very similar in appearance to a lipoma, but the reasons for the formation of seals are completely different. They also need to be treated differently.
Lipoma
Wen or lipoma also refers to benign skin tumors. It does not hurt when pressed, but a person may feel discomfort. The main difference from atheroma is that lipoma is fixed , it does not move along with the surrounding tissues.
The main reasons for the formation of a wen:
- hereditary predisposition;
- hormonal changes in the body associated with menopause, pregnancy, illness;
- insufficient personal hygiene of the skin area.
Lipomas should not be punctured or attempted to be squeezed out. This can lead to infection and suppuration. As a result, inflammation will occur in the palm with the release of foul-smelling contents.
Most often, lumps grow slowly, so few people go to the doctor unless the lump is located on the face.
Lipoma responds well to treatment with folk remedies, homeopathy , so you should first try conservative methods.
Cyst
A cyst on the palm can appear anywhere : in the center, on the finger, close to the nail. This benign tumor is formed due to repetitive movements, trauma, hereditary factors, excessive physical stress on the arms or joints of the hand.
The cyst can be single-chamber or multi-chamber. The neoplasm is mobile upon palpation. On the palms, cysts are not very large; they resemble cartilage, causing discomfort. The seal is elastic and painless. The contents can become inflamed and fester . In this case, pain appears.
The inflamed cyst is removed surgically . A small compaction can be eliminated using conservative methods - ointments, physiotherapeutic procedures.
Dupuytren's contracture
This is a scar change in the fascia covering the tendon . With Dupuytren's contracture, the tendons shorten and this leads to the inability to fully extend the fingers . The ring and little fingers are most often affected.
Contracture most often occurs in middle-aged men. The disease progresses rapidly over time if treatment is not started. In women, this pathology is less common and develops slowly, most often in old age.
Xanthoma
Xanthomas are subcutaneous neoplasms of lipids . There are:
- papules (xanthomas);
- plaques (xanthelasma);
- nodes (lumpy xanthomas);
- flat plaques;
- infiltrates (tendon xanthomas).
The reasons for the formation of compactions are:
- metabolic disorders - lipid metabolism;
- biliary cirrhosis of the liver;
- dysfunction of the thyroid gland - hypothyroidism;
- histiocytosis;
- hereditary hyperlipoproteinemia.
Histologically, subcutaneous deposits are accumulations of macrophages carrying huge amounts of lipids.
Treatment consists of a strict diet that excludes fatty acids and cholesterol-containing foods that sequester bile acids. In some cases, a liver transplant is required.
Corn or condyloma
Wet callus
A callus with liquid inside (wet) on the palm appears due to strong mechanical friction. Subsequently, the liquid disappears, and a dry skin remains on top, which can be carefully removed.
Dry calluses occur due to prolonged, but not too intense friction. This way the skin protects soft tissues from damage.
The callus has a deep root. It can only be removed surgically.
Condyloma is a skin manifestation of human papillomavirus infection. They usually occur during menopause in women, as the immune system weakens. Diagnosis of the type of virus is required - oncogenic or non-oncogenic.
Dry callus
Callus
Condyloma
Stages of Dupuytren's contracture
Like any other disease, Dupuytren's palmar fascial fibromatosis occurs in several stages:
- A small nodule appears in place of one of the tendons , which people tend to consider a callus. It doesn’t bother me in any way and the joints still retain the same mobility.
- The nodule develops into a scar cord and passes to the proximal digital phalanx. The skin in the area of the scar cord becomes rough and red, the finger bends at an angle of 30 degrees and loses mobility.
- The disease spreads over the entire finger , the skin on it becomes wrinkled and folded, and the finger itself bends 90 degrees, contracture of the entire hand is observed. At this stage, fusion of the joint surfaces is already possible, in other words - ankylosis.
- Adjacent fingers are affected, sometimes the entire palm. Often they grow together into a single large scar, with the first affected finger at a 90-degree angle, and the rest severely deformed. The palm may be dislocated, and the patient feels aching pain in the deformed areas.
There is no discomfort until the last stage, and it is rare for the disease to progress that far. In the first stages, it can only be detected visually, so diagnosing the problem is possible only with a person’s attentive attitude to health.
Features of warts on the palm
Warts can affect absolutely any part of the epidermis of the hands, but most often form on the back of the hand or in the area of the fingers. Moreover, most of these formations are classified as vulgar growths, which do not differ in color from healthy skin and are relatively small in size - 0.1-1 cm.
As for the number of such neoplasms, there are both single skin defects and multiple warts that tend to merge.
The distinctive signs of warts on the palms are the following:
- No pain or itching;
- The site of the skin defect does not have an epidermal pattern, which is usually restored after removal of the wart;
- Black dots, which represent coagulated vessels, may appear on the surface of the formation.
Based on all of the above, we can conclude that warts on the palms are more of an aesthetic defect, which, however, in the absence of timely treatment can lead to a significant growth of tumors and a high risk of mechanical damage.
How to treat Dupuytren's contracture
Before you begin treatment, make sure you have this problem. It can be found both in the doctor’s office and on your own: place your hand on a flat horizontal surface, for example, on a table, palm down. If there is an arched gap between the fingers and the table - stage 2 is possible, the gap looks like a hut - stage 3, there is no space between the finger and the table - then you do not have the disease.
The diagnosis is made by an orthopedic surgeon based on the patient’s complaints and visual assessment of the hand. He may also order an x-ray examination.
The treatment itself is aimed at reducing the scar stage and depends on the degree of disease progression. So, at the first stage it is still possible to avoid surgery, but at the second stage, most likely, it will be needed. In subsequent stages, surgical intervention is mandatory.
Depending on the degree of Dupuytren's contracture, treatment can be conservative or surgical.
Surgical treatment is used starting from the second stage of Dupuytren's contracture and involves surgical intervention. Can be done in several ways:
- needle aponeurotomy with lipofilling;
- dissection of the cords through the skin, otherwise needle percutaneous aponeurotomy;
- dissection of scar cords, or open aponeurotomy;
- removal of scar cord within healthy tissue, the medical term is open aponeurectomy.
The open aponeurectomy method is used quite widely: it is considered a reliable way to cure Dupuytren's contracture on the hands.
Conservative treatment of Dupuytren's contracture is only a preparation for surgery and includes:
- thorough handling, that is, washing hands with a brush;
- softening and moisturizing the skin with cream;
- local injections with a complex of vitamins and corticosteroids;
- phonophoresis with hydrocortisone.
The early stages can still be cured with the help of physiotherapy with Fermenkol, the main thing is to recognize the problem in time and choose the right drug for it. Experienced surgeon A.V. talks about this in more detail. Zhigalo in his interview.
What does it look like?
Warts are small, dry, flesh-colored lumps. They have a rough surface and are sometimes painful. On the hands, this can lead to a pronounced cosmetic defect.
When warts appear on the feet, severe pain appears, making it difficult to walk. Another type of wart, genital warts, develops on the genitals. This can make intimate relationships difficult. It is important to note that in women, condylomas of this localization can be caused by strains of the virus that increase the risk of cervical cancer.
Such situations require immediate treatment.
Recovery after surgery
Depending on what kind of intervention was performed, restorative procedures and treatment complexes are selected.
Thus, rehabilitation schemes have been developed after “open” operations for Dupuytren’s contracture and after needle aponeurotomy - a relatively new method without surgical intervention.
Scheme of recovery procedures after “open” operations
After surgical intervention on the hand, hardening of the palmar surfaces, tissue swelling and limited joint mobility are observed.
3-4 weeks after surgery you can follow the following scheme:
- magnetic laser therapy;
- paraffin for 30–40 minutes;
- On a hot hand, either ultraphonophoresis is applied (it is recommended to use it with Fermenkol gel, information about it below), or electrophoresis with Fermenkol solution.
For magnetic laser therapy, a scanning method is used to influence the palm, the device moves at a speed of 0.5-1 cm/s, the duration of the procedure is 5 minutes.
Paraffin and physiotherapy (this includes ultraphonophoresis and electrophoresis) are carried out according to standard methods. The duration of the course varies from 10 to 15 procedures; you can recover after surgery for Dupuytren's contracture at home - to do this, it is enough to purchase a Reton device for phonophoresis or an Elfor device for electrophoresis.
Rehabilitation therapy after needle aponeurotomy
After undergoing treatment, you can return to your normal life the next day, and heavy physical activity after a week. However, to consolidate the result, physical therapy is recommended, starting from day 3.
If treatment was carried out at stages 3–4 of contracture, then consequences are possible, such as:
- worsening joint stiffness due to man-made contractures;
- loss of elasticity;
- wrinkling of the skin;
- muscle weakness due to prolonged vicious position of the fingers.
To reduce these disadvantages, hand surgeon A.V. Zhigalo recommends using paraffin therapy together with phonophoresis or electrophoresis in combination with Fermenkol products, as well as exercise therapy (physical therapy).
Treatment
Conservative therapy
Treatment of finger hygiroma at an early stage is carried out using medications and physiotherapy. The patient should refuse physical activity.
Reference. Conservative treatment is associated with frequent relapses.
Medicines are used for non-purulent inflammation:
- Nimesil is a non-steroidal anti-inflammatory drug.
- Diclofenac in the form of an ointment demonstrates a pronounced analgesic and anti-inflammatory effect.
- Clemastine in tablet form is an antihistamine that accelerates the destruction of histamine and reduces its concentration in tissues.
Physical therapy is carried out to reduce the size of the tumor, relieve or eliminate inflammation that has arisen due to compression of the surrounding tissues by the formation.
For hygroma, the following physiotherapeutic techniques are used:
- Deep heating of tissues with high frequency and intensity current. After the procedure, the inflammatory process is alleviated, blood circulation is normalized, and tissue restoration is accelerated.
- Ultrasound therapy improves blood circulation in small vessels, reduces the tone of striated and smooth muscles. Under the influence of ultrasound, more oxygen enters the tissues, and they recover faster.
- Magnetic therapy weakens the inflammatory process in cartilage and bones.
- Balneotherapy is treatment with mineral waters (sodium chloride, radon, hydrogen sulfide baths). After the procedures, adhesions and structures become softer, lengthen, and the severity of the inflammatory process decreases.
In addition, electrophoresis with glucocorticosteroids, radiotherapy, mud or paraffin wraps are used to eliminate the tumor.
To remove the tendon ganglion without surgery, a puncture is prescribed. To do this, the joint capsule is punctured, the contents of the cyst are pumped out, after which the cavity is treated with antiseptics or glucocorticosteroids (Diprospan). If the hygroma becomes infected, antibacterial drugs (Neomycin, Amicil) are injected into its cavity after aspiration (suction of the contents). The puncture is performed under local anesthesia, so the patient does not feel pain.
After the procedure, a pressure bandage and an orthosis (a medical device that relieves stress on the joints) are put on the affected area. During the rehabilitation period, it is forbidden to subject the finger to stress.
The most dangerous methods include crushing the hygroma. During the procedure, the doctor squeezes the tumor with his hands or plastic objects. When the membrane ruptures, the fluid spreads throughout the surrounding tissues, which is accompanied by intense pain.
Carefully. Crushing a hygroma is a painful method that provokes dangerous complications (inflammation, suppuration) and frequent relapses. After the procedure, the cyst shell remains inside, so the risk of new ganglia forming is high.
Surgical intervention
If conservative treatment is unsuccessful, which happens in most cases, then doctors prescribe surgery.
Bursectomy is an effective method for removing finger hygroma.
It is necessary to treat the growth surgically in the following cases:
- Education is increasing rapidly.
- Painful sensations occur that intensify during movement.
- The mobility of the joint is limited.
- Aesthetic discomfort.
Removing the growth lasts no more than 30 minutes. The area around the tumor is numbed. The surgeon excises the formation along with the membrane and fluid and carefully separates it from the joint. Then stitches are placed on the surgical wound and removed after 7–10 days.
Reference. If the tumor is large, then bursectomy is performed under general anesthesia in the hospital.
Laser treatment is an effective alternative to classical surgery. The procedure is performed under local anesthesia, so there is no pain.
Using a laser beam, the skin over the cyst is cut, and the membrane with liquid is removed. Then the cavity is treated with antiseptics, stitches are placed on the wound, and the top is covered with a sterile bandage to prevent infection.
After treatment, the affected joint is fixed with brace and immobilizing plaster orthoses. They are comfortable and do not interfere with joint mobility.
Reference. After laser removal of hygroma, there are no scars. The procedure lasts approximately 15 minutes, after which the patient can go home.
Alternative Treatment
In the early stages of development of the tendon ganglion, you can use traditional medicine (complex therapy). They will not replace traditional treatment, but can speed up recovery.
Folk remedies against synovial cysts:
- Take a copper coin, heat it on a fire, and dip it in an aqueous solution of salt. Then bandage it to the damaged area. After 3 days, remove the bandage, rinse your finger and repeat the procedure.
- Take a piece of the jellyfish’s body and secure it on your finger with a bandage. After 3 hours, remove. Repeat the procedure every day. Kombucha can be used in the same way.
- Grind the cabbage leaves using a blender or meat grinder, squeeze out the juice through cheesecloth. Drink it 200 ml per day for 4 weeks.
- Squeeze the juice from celandine leaves (25 ml), apply to the tumor, after steaming your finger in hot water. Bandage it, cover it with cling film, and then wrap it in a warm cloth. Treatment lasts about 20 days.
There are many more recipes for the treatment of pathology, but they can only be used after the approval of a doctor.