Many birthmarks are harmless and do not require any treatment. They either disappear as the child grows or remain on the skin, but do not pose a health hazard.
Other moles can grow very quickly. Without medical treatment, they can become large, permanent areas of discoloration that can affect the deeper layers of the skin. If the birthmark is located in a very visible location, parents may decide to keep its appearance to a minimum while the child is young.
Drug and laser therapy can be very effective in reducing the size of birthmarks and preventing them from recurring.
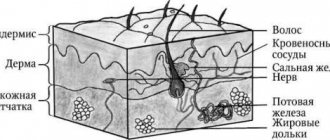
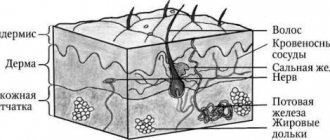
Congenital malformations of the skin and subcutaneous fat
Congenital malformations of the skin and subcutaneous fat in children have various forms of manifestation.
One of them is nevus. This is a neoplasm that appears as a result of a high concentration of nevocytes in a certain area of the skin. Normally, skin color is formed by melanocytes distributed in equal density. However, pathology may develop, due to which melanocytes degenerate into nevocytes, which, through their accumulation, form a pigmented nevus in a child. It can occur during pregnancy or appear shortly after birth.
To one degree or another, the following factors can lead to the development of pathology:
- gene breakdown;
- the presence of a genitourinary infection in the mother during pregnancy;
- heredity;
- the impact of negative external factors on the mother’s body during pregnancy;
- incorrect diet of the mother during pregnancy, the predominance of artificial colors, preservatives, and flavors;
- long-term use of hormonal contraceptives before pregnancy.
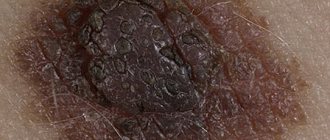
Initially, pigmented nevus in children is defined as a benign formation. However, it may have melanocytic activity, which means it can grow. As the child ages, not only the spots may grow, but also the appearance of new ones, as well as their degeneration into malignant tumors. A skin tumor - melanoma - is aggressive, as it quickly progresses and metastasizes to nearby organs and tissues.
Pigmented nevus is detected in approximately 1% of children.
Boys and girls are equally susceptible to the appearance of spots on the skin. A nevus can look different: a medium or large-sized nodule, a spot colored differently from the main skin tone, a wart. Localization is also varied: limbs, torso, head. In most cases, nevus occurs on the child's head, neck, chest or upper back.
The size of the formations varies from several mm to several cm. In approximately 5%, the number of nevi is so large that they occupy a significant proportion of the skin surface. Normally, when palpated, they can be both soft and nodular, but without pain.
Local medications
If a hemangioma develops in a sensitive area where the skin is thin, such as the eyelid, dermatologists may prescribe a topical medication called Timolol. Like propranolol, timolol causes the birthmark to shrink and disappear by preventing the formation of new blood vessels and making existing blood vessels smaller.
This medication is a gel that parents apply directly to the birthmark, usually twice daily, for the first year of the child's life. The amount of gel applied and the duration of use of the drug are determined by our dermatologists based on the size of the mole. Many people see significant improvement in the size and appearance of hemangiomas within a few weeks.
Types of nevi
The spots have clear boundaries and color from pale brown to black.
Small and medium-sized formations, due to their light tone, can be practically indistinguishable in the first 2-3 months after the birth of the child. However, as they grow, they darken and grow proportionally in size. Nevi can also be non-pigmented, then they can be identified by touch by the different structure of the skin.
Spots are divided by size into:
- small - up to 1.6 mm;
- medium - from 1.6 to 10 mm;
- large - from 10 to 20 cm;
- giant - from 20 cm.
Another criterion for classification is clinical type. According to it, nevi are:
- Adenomatous. They are located on the face and head, have a convex shape, clear boundaries, and the color varies from yellowish to dark brown.
- Warty. Located on the torso or limbs. They are characterized by uneven outlines and surface, dark color.
- Giant pigment ones. They often develop in utero and can be located on one or both sides of the body. The surface is covered with hairs, often accompanied by a scattering of small neoplasms around them.
- Blue. They are located in the upper body, on the face and hands. The color is bluish or gray-blue, the surface is dense and glossy. The nevus protrudes slightly above the surface of the skin and does not exceed 2 cm in diameter.
- Papillomatous. They are located on the head and do not have clear boundaries or outlines. The surface is heterogeneous, the color ranges from light to almost black. When injured, it becomes inflamed.
- Epidermal. They are usually located on the limbs one at a time. They have an uneven surface and color from light to dark.
A characteristic sign of a non-malignant neoplasm is the presence of hairs on the surface.
Oral therapy
Propranolol is a medication taken by mouth that can be very effective in reducing the size and lightening the color of hemangiomas, which are vascular birthmarks caused by malformed blood vessels. Propranolol inhibits the growth of new blood vessels inside hemangiomas and shrinks existing blood vessels.
Dermatologists may prescribe propranolol if the hemangioma is located in the airway or near the eyes or mouth and threatens to impair functions such as vision or breathing. Your doctor may also prescribe this medication to shrink hemangioma for cosmetic purposes.
Propranolol comes as a liquid medicine and is taken two to three times daily during the child's first year of life, when hemangiomas tend to grow more aggressively. These birthmarks often become smaller or lighter in color within a few weeks.
After the first year of treatment, dermatologists evaluate the size and color of the hemangioma before recommending additional treatment. The goal of treatment with propranolol is to continue therapy until the hemangioma no longer grows and to gradually discontinue treatment as soon as possible after one year. However, stopping treatment too early may result in regrowth.
Methods for treating nevi
Treatment is allowed only in patients over 2 years of age. Therapy has 4 main directions:
- surgical removal;
- laser excision;
- cryodestruction;
- electrocoagulation.
As a rule, nevi that have grown deeply into the tissue are surgically removed. Giant neoplasms are removed in several stages, but the disadvantage of this method is the formation of scars at the site of the nevi.
Laser coagulation is used to remove dysplastic pigmented nevi and other clinical types of spots. The method allows removal of the formation without pain and without subsequent scarring.
Cryodestruction involves exposing the affected area of skin to very low temperatures. As a result, the altered cells die and are replaced by healthy ones. After cryodestruction, a small crust appears, which quickly disappears.
Electrocoagulation affects the nevus with high temperatures. Typically this method is used to remove small and medium-sized stains.
Laser treatment
Laser treatment uses highly focused beams of light to reduce the size and color of birthmarks. This includes red birthmarks such as strawberry hemangiomas and port wine stains; brown birthmarks, such as café au lait spots; and blue birthmarks such as facial skin melanocytosis.
When the laser beam enters the skin tissue, it is converted into heat and eliminates blood vessels. For birthmarks that are brown or blue, laser is used to target and reduce melanin, the substance responsible for skin pigment.
It may take several treatment sessions to lighten birthmarks that are larger or darker in color. Recovery after laser therapy is minimal. Your child may have some slight bruising after treatment, but it is not painful and will go away within a few days.
Particular attention should be paid to protecting your child's skin from sun damage after laser therapy sessions. Dermatologists may recommend covering the affected area with sunscreen with SPF 30 or higher. They may also suggest covering the area with a bandage.
Diagnosis of blue nevus
In most cases, one visual examination by a dermatologist is sufficient to accurately verify the diagnosis. In unclear and controversial clinical cases, the following examination is recommended:
- dermatoscopy (under magnification, the boundaries, depth and structure of pigment formation are studied more carefully);
- siascopy (assessment of the structure and distribution of melanin);
- ultrasonography of the nevus (to exclude infiltrative growth of a malignant nevus);
- histological examination of biopsy specimens (rarely) or surgical material (detects characteristic accumulations of melanocytes in the deep layers of the dermis; with a simple blue nevus, the cells are rich in melanin, and with a cellular nevus, islands of large cells with a small amount of pigment are observed);
- determination of tumor markers SU100 and TA90 (to exclude the development of melanoma).
Symptoms of blue nevus
Blue nevus can appear in people of any age group, but most often it is first discovered in middle age. It usually does not cause patients any particular discomfort (except for a cosmetic defect when it is localized on the face and is large in size). Blue nevus has the following clinical characteristics:
- intradermal nodule;
- round, spindle-shaped or elliptical shape;
- light gray, dark blue, blue-black or blue color;
- uneven color;
- clear contours;
- smooth, hairless surface;
- the size rarely exceeds a centimeter (although there are blue nevi larger than 3 cm);
- protrudes slightly above the skin or does not rise above it at all;
- the consistency is elastic and dense;
- most often localized on the buttocks and limbs;
- can form on the mucous membranes of the mouth, vagina, and cervix.
Choosing a mole removal method
In specialized departments of the NEARMEDIC clinic network, removal is carried out only by certified specialists in the field of dermato-oncology and dermatocosmetology, who have appropriate certificates certifying their high qualifications in dermatological surgery, laser, radio wave and other modern technologies in the removal of tumors.
Surgical method
The traditional method of surgical excision in the case of diagnosing a low-quality degeneration of a mole is carried out with a mandatory subsequent histological examination of the excised neoplasm tissue. The disadvantage is the risk of formation of postoperative scars, since the neoplasm, when removed by this method, is excised along with the surrounding tissues. This method is preferable when identifying melanoma-dangerous tumors that are localized in areas of the body hidden by clothing.
Radio wave surgery
When removing a tumor in a non-contact manner using a radioknife (radioscalpel), the surrounding tissues are not affected - the effect is aimed exclusively at the pigmented formation. Radio wave radiation is tuned to destroy cells containing melanin. Radio wave surgery does not leave burns or scars. Coagulation of capillaries prevents bleeding. It is used to eliminate benign (for cosmetic and preventive purposes) and malignant pigmented formations.
Cryodestruction
If the pigmented formation does not rise above the level of the skin, liquid nitrogen treatment - cryodestruction - can be used to eliminate it.
Laser mole removal
Laser removal of moles is one of the most progressive and effective methods. In NEARMEDIC clinics, the procedure is performed with a new generation carbon dioxide CO2 laser using local anesthesia. The laser beam is adjusted to vaporize (evaporate) cells containing melanin, after which the pigmented formation is removed layer-by-layer. The procedure is absolutely sterile due to the sealing of capillaries and the absence of bleeding, leaves no scars or cicatrices, eliminates relapse, stimulates the regenerative abilities of skin cells - the production of collagen, hyaluronic acid, elastin, which renew the skin.
You can make an appointment with a dermatologist-oncologist or dermatologist-cosmetologist of the NEARMEDIC clinic network by calling the single telephone number of the contact center or through the contact form on the website. You can find out the cost of treatment on the prices page.
Treatment of blue nevus
As a rule, doctors choose a wait-and-see approach. Patients only need to visit a dermatologist or oncologist regularly for examination. Removal of a blue nevus is necessary only if localization is unsuccessful, causing permanent injury to the formation, and if a number of alarming signs appear:
- a significant increase in its value;
- color change;
- blurred contours;
- the appearance of itching or pain.
To remove a blue nevus use:
- electrocoagulation
- cryodestruction;
- laser;
- radio wave method;
- traditional surgical excision (the nevus is removed along with 5–8 mm of intact skin surrounding it and subcutaneous fat).