HPV types
The content of the article
Medical experts identify more than 100 types of HPV. However, not all types of HPV are dangerous to humans.
The development of cancerous tumors can be expected when the following types are detected: 16, 52, 18, 68, 45, 31, 58, 33, 35, 39, 59. Types 18 and 16 are considered especially dangerous among them. It is in the presence of such that high mortality is observed. Each carcinogenic type of virus can lead to cancer:
- cervix;
- penis;
- anus;
- vulva;
- larynx;
- mouth
Low chances of getting cancer if types are detected: 11, 43, 42, 6, 44. Not a single case of cancer has been identified so far in case of infection with types: 1, 3, 5, 2, 4.
The peculiarities of the human papillomavirus are such that infection with one type does not mean that a person will be protected from others.
Human papillomavirus HPV and cervical cancer
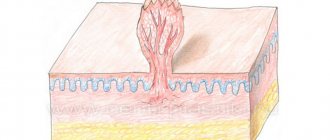
Human papillomavirus (HPV) is a DNA virus of the Papillomaviridae family. This family includes common and genetically diverse viruses that infect and damage epithelial cells (skin, mucous membranes of the anogenital area, oral cavity).
More than 130 HPV genotypes are known. According to clinical classification, they are divided into cutaneous and anogenital types of papillomaviruses. It is the anogenital types of HPV that cause damage to the mucous membranes of the vagina and cervix. The most harmless of these diseases are benign genital warts, the most dangerous is cervical cancer.
Human papillomaviruses are transmitted through sexual contact. With the onset of sexual activity, the vast majority of women become infected with this virus. It should be taken into account that the risk of HPV infection depends on the number of sexual partners and on the sexual behavior of the only partner (the prevalence of HPV in men is approximately equal to the prevalence in women).
Human papillomavirus infection itself is not a disease. After 6-18 months, in ~80% of infected women, the virus leaves the body on its own, without any treatment, without causing illness (spontaneous elimination). And only a small percentage of women with chronic (persistent) infection caused by highly oncogenic HPV genotypes may develop cervical cancer after 10-20 years. It seems that there is enough time for successful diagnosis and treatment, but there is no need to relax.
Human papillomavirus infection is very insidious, and the precancerous changes associated with it, as a rule, not only do not cause any concern or discomfort, but are often not detected during a routine gynecological examination.
Therefore, to detect human papillomavirus infection, an HPV test using the polymerase chain reaction (PCR) method is used. The HPV test is a reliable doctor’s assistant: detection of papillomavirus and determination of its genotype allows you to determine further tactics for the management and treatment of a woman.
It should be taken into account that the identification of HPV of a high carcinogenic risk group in women is not the basis for making a diagnosis of a malignant tumor, but serves as a reason for further examination, more intensive monitoring and, if necessary, treatment of precancerous changes in the cervical mucosa.
The outcome of HPV infection depends on the genotype of the virus. All papillomaviruses are divided into groups according to “harmfulness” or “oncogenicity”. HPV polymerase chain reaction (PCR) tests detect all common and clinically significant HPV genotypes.
The low carcinogenic risk group includes HPV genotypes 6 and 11: they can cause genital warts and mild dysplasia. Analysis for HPV genotypes 6 and 11 is used for differential diagnosis with diseases of non-papillomavirus etiology and when examining pregnant women to assess the risk of developing laryngeal papillomatosis in newborns.
- Human papillomavirus 6/11, qualitative DNA determination, PCR
Genotypes 16 and 18 of papillomaviruses most often lead to cervical cancer. They, together with types 31, 33, 35, 39, 45, 51, 52, 56, 58, 59 and 68, are included in the group of high carcinogenic risk. When conducting tests for human papillomavirus, it is these genotypes that you need to pay special attention to. The most important is DNA analysis of HPV types 16 and 18, especially if their con) is high. And the oncogenic potential of types 51 and 56 is not so great, so they are less dangerous, even if they are present in relatively large quantities in the HPV test.
- Human papillomavirus 16/18, qualitative DNA determination, PCR
- Human papillomavirus 16/18, DNA quantification, PCR
- Human papillomavirus of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68), total qualitative DNA determination, PCR
- Human papillomavirus of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52,56, 58, 59), qualitative determination of DNA indicating the type of virus
- Human papillomavirus of high carcinogenic risk (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68), total DNA quantification
- Extended HPV test (with determination of the amount and type of virus)
You can get tested for HPV in women using the PCR method (HPV test) yourself, without a doctor’s referral. If HPV infection is not detected (negative HPV test result), then the risk of developing cervical cancer is low. But you should remember that if you continue to be sexually active, the risk of HPV infection remains.
If the result of the HPV test is positive, HPV of high carcinogenic risk is detected, it is necessary to do an extended study to clarify the genotype of the virus (HPV analysis - typing) and the “viral load” (human papillomavirus - quantitative analysis). Then you need to contact a gynecologist for a colposcopy - an examination of the cervix under magnification using a special device - a colposcope.
All additional tests for human papillomavirus and other studies must be carried out as prescribed and under the supervision of a physician.
If damage to the cervical mucosa is detected at an early stage, preceding cancer, then treatment is more effective and has virtually no side effects. If no pathological changes are detected in the cervical mucosa, then there is no need for treatment: most likely, the body will cope with the virus on its own.
However, after 1 year, it is necessary to undergo repeated HPV testing and, if the virus is still present, to be examined again by a gynecologist.
Analysis for human papillomavirus (HPV) by PCR and cytological studies.
In Russia, the compulsory health insurance (CHI) system includes a cytological examination - “smear for oncocytology”. Are HPV tests necessary then?
The basis of modern screening programs for the early detection of cervical cancer is the Papanicolaou cytological examination (PAP test, Papanicolaou staining). Unfortunately, not all Russian medical institutions use this technique; very often other, less advanced methods of preparing (staining) a cytological smear are used.
In addition, it is important to know that the cytological method is not an analysis for the human papillomavirus. Cytology “does not see” the virus itself, but reveals epithelial cells that have already been changed under its influence, that is, clinical and subclinical forms of HPV infection. The cytological test also has very significant disadvantages - low sensitivity, subjectivity of interpretation and dependence of the result on the quality of the cytological smear.
That is why traditional cytological screening is characterized by a large number of false-negative and indeterminate results requiring repeated studies.
To reduce the possibility of errors, cytological tests have been improved - the liquid cytology method has been introduced. Liquid-based cytology is a new technology for preparing cell samples from the cervix for cytological examination. The advantages of this method are a reduction in the number of inadequate smears and artifacts, and the ability to avoid contamination of samples with inflammatory exudate and red blood cells, which ensures high quality cytological preparations. Today, it is this method of cytological screening for cervical diseases that is recommended by WHO (World Health Organization) as the “gold standard” for the study of cervical smears.
- Pap test liquid
According to the latest international and domestic recommendations, the combined use of HPV analysis (HPV PCR test) and cytological examination (PAP test) is the preferred method for the early detection of cervical cancer in women over 29 years of age. Such screening must be carried out regularly - once every 3 years.
- HPV-PAP test (set of tests: HPV extended with determination of the amount and type of virus + PAP test)
- HPV-PAP test liquid (set of tests: HPV extended with determination of the amount and type of virus + PAP test)
Causes of papilloma virus infection
The main reason for the spread of the virus is unprotected intimate relationships. At the same time, representatives of the fair sex, as statistics show, are more susceptible to infection. Thus, the probability of infection in men through sexual contact is 25-70%. The risk of infection in women reaches 80-90%.
In addition, the virus can be transmitted in the following cases:
- blood transfusions;
- at birth - from mother to child;
- through household items - personal hygiene products;
- as a result of cuts, wounds and the like.
Patient preparation rules
urogenital smear (female)
Standard preparation conditions (unless otherwise determined by the doctor):
Abstain from sexual intercourse for 48 hours.
Stop taking intravaginal products for various purposes (suppositories, spermicides, douching, tampons, local procedures, etc.). 2 hours before, refrain from urinating. Important:
Take before treatment or 21 days after the end of antibacterial, antimycotic therapy (unless otherwise determined by the doctor).
biopsy of the placenta (chorion) Important:
Donate before treatment or 21 days after the end of antibacterial, antimycotic therapy (unless otherwise determined by the doctor).
You can add this study to your cart on this page
Screening - general examination
Many women are interested in what HPV screening is. First of all, it should be pointed out that this is a qualitative analysis that allows you to detect cervical cancer in the early stages, as well as find out about the presence of dangerous types of viruses in the body of a particular person.
In women, HPV screening is done directly during a gynecological examination. In this case, the doctor takes a smear, which is subsequently tested in a laboratory. If a human papillomavirus infection is detected as a result, the woman should undergo a more thorough examination, including to identify pathological changes in tissue.
Several other methods are actively used today to establish the diagnosis of IF.
- PCR. Its purpose is to identify the DNA of the pathogen in biological material: blood, urine, secretions. Therefore, it is possible to find out which stamp is present.
- Genotyping. Helps determine whether the infection has an initial form or a chronic one.
- Digen test. Quantitative method indicates the amount of virus.
It is up to the doctor to decide which test to use and when exactly to screen for HPV.
Is it possible to do HPV without genotyping?
Of course, such an analysis can be done.
It is also quite informative.
HPV genotyping costs are higher, and such costs are not always necessary.
In any case, as a result of the test, the type will be determined or not, the doctor will find out whether the HCV papillomavirus is present in the body.
If it is present, and if it is present in high concentrations, in any case the patient must:
- treatment;
- dynamic observation.
And this is necessary, regardless of the specific type of virus detected.
What does advanced screening show?
For a more complete examination and diagnosis, as well as in case of suspicion of several types of HPV at once, it is appropriate to ask for extended HPV screening. This one contains information about 15 types of viruses. Essentially, this is a quantitative method that makes it possible to detect DNA. The main feature that distinguishes HPV HCR screening is its 100% specificity of determination.
Having received the results of the polymerase chain reaction PCR, the doctor has the opportunity to more successfully select a treatment regimen.
Extended testing, cervical screening is deciphered using a special parameter - control of material collection.
Why is HPV genotyping needed?
HPV is a heterogeneous virus.
This means that there are many forms of it.
In fact, this is a whole family of viruses, varying in their level of pathogenicity.
When infected with different types of HPV, the risk of cancer increases to varying degrees and different symptoms occur.
About 40 types of HPV are transmitted sexually.
Fourteen of them are viruses of high oncogenic risk.
Thus, genotyping is used to find out what type of virus persists in the patient.
This is important for assessing oncogenic risk.
Patients with different types of HPV are managed completely differently.
If with low-oncogenic viruses a person can have warts removed and sent home, then detection of highly oncogenic types requires dynamic monitoring.
The role of drug therapy is increasing.
It is important for a person to get rid of carriers of the virus as soon as possible in order to prevent precancerous processes and cancer.
Is screening reliable?
Today it is difficult to find a more reliable and affordable way to detect the HPV virus than screening. It only takes a few days for specialists to point out the presence of potentially dangerous factors.
Modern private clinics have all the necessary equipment, indicators and tools that allow the test to be carried out with the highest quality possible. For ease of use of the PCR method and ease of interpretation of the results, recalculation into Digene units occurs. Therefore, the probability of error is very low.
Why diagnose a disease?
Timely detection of the virus in women or men makes it possible to save a person from death. It is very difficult to identify the presence of carcinogenic types, because the problem may not manifest itself from the outside for a long time.
Having received accurate results, the doctor can find out whether condylomas pose a threat, whether they lead to the appearance of degenerated tumors, and whether they should be removed at all.
Timely diagnosis helps prevent the development of cancer, and if it is present, select the most effective control regimen.
Who should be screened?
All women over 30 years of age should be tested for HPV. If no carcinogenic types are found in them, then it is worth repeating such an analysis at least once every 2-3 years.
You also need to donate blood to determine the virus:
- during pregnancy;
- with severely reduced immunity;
- if a person is struggling with signs of having HPV;
- after unprotected contacts, blood transfusion.
Also, all people who have already been diagnosed with the disease should undergo such an analysis from time to time.
What will the doctor tell you before the test?
By contacting a specialist, the client receives the most complete consultation regarding screening and the specifics of its implementation. The patient will receive comprehensive information on how to undergo HPV screening. In women, material is collected in a hospital setting. The gynecologist makes a scraping from the cervical canal.
For male patients, PCR analysis is performed in the same way.
Some other methods of diagnosing the virus involve simply taking a blood test.
What do you need to do to complete the study?
Each patient should prepare before the test: before going to the doctor, you need to carry out normal hygiene procedures, but do not use too much detergent or antibacterial agents or lotions.
We will not have a successful analysis if the patient uses medications during the last three days before collecting the material.
Men are prohibited from urinating for 2 hours before the collection of material.
What are the indications for diagnosis?
Tests are required as screening for women and girls who are characterized by: an active sex life, frequent changes of partners, antisocial behavior, lifestyle, and so on.
And also to those of them who have atypical cells found in cytological smears during medical examinations.
Men should also be periodically screened for HPV infection.
And if condylomas or warts appear in the groin, anus, or perineum, it is imperative to get examined.
In order to get tested for HPV, you need to contact an experienced and professional dermatologist or venereologist.
The doctor will conduct an examination, collect diagnostic material himself and send it for examination to an accredited and certified laboratory.
How to evaluate the results of an HPV test
The first fact that the doctor pays attention to is the presence or absence of viral DNA in human biological materials. Normally, its DNA should be completely absent. At the same time, the test results are used to determine the characteristics of the course of the disease.
Thus, indicators up to the number 103 indicate a transient, that is, low-hazard current. In this case, over the course of one year, the person retakes the screening several more times. Confirmation of transientness is a decrease in indicators several times.
If the results indicate a figure of more than 103, the doctor can conclude that the disease is chronic. The likelihood of developing cancer is then very significant.
Indicators of more than 105 indicate the onset of cervical cancer development.
HPV genotyping: what does this analysis provide?
This is the process of determining the type of virus.
It is based on determining a section of DNA, that is, the genotype of the pathogen.
Research objectives:
- determination of oncogenic types of virus;
- establishing the degree of oncogenic risk for a particular patient (the virus is determined in combination with other research methods);
- determination of therapeutic tactics.
As a result of the test, the doctor receives the following information:
- whether the virus that persists in the human body is highly oncogenic;
- what type of virus it is (even within the group of oncogenic HPVs there are viruses that, to a greater or lesser extent, increase the likelihood of cancer);
- in what concentration it is contained (if there are few viruses, it is likely that the body will soon get rid of them on its own).