Why do papillomas appear on the neck?
Contrary to many myths regarding etiotropic factors in the formation of papillomas , these skin growths are a manifestation of the presence in the patient’s blood of the human papillomavirus (HPV), which has more than 120 known strains. It is not difficult to become infected with such a viral agent, either through direct contact with a carrier or through common household items.
Quite often, papillomas appear in childhood, which is explained by the increased sensitivity of the child’s body to infections and viruses. In addition, papillomas are also characterized by a perinatal spreading factor, which involves the transmission of HPV from mother to child in the womb.
The following circumstances can remove the virus from a latent (“dormant”) state, in which it can remain indefinitely:
- Decreased immunity;
- Endocrine disorders;
- Exacerbation of chronic diseases;
- Injuries, scratches, open wounds;
- Overwork and stress;
- Poor nutrition and bad habits;
- Lack of personal hygiene;
- Weakening of the body due to an infectious or inflammatory process.
Papillomas on the neck often begin to appear during the healing period of scratches and microcracks in the skin, which can be caused by friction of a chain or clothing.
Types of warts
HPV is divided into several dozen types. They cause different types of warts:
- Anogenital warts are caused by HPV types 6 and 11. These warts are located around the anus and on the genital mucosa;
- Plantar warts resemble calluses and are caused by HPV types 1–4. They are very painful and often interfere with walking;
- Flat warts appear as flat nodules and are often located on the fingers or on the back of the hand. Most often, such warts form in children and young people, which is why they are also called juvenile warts. They are caused by HPV types 10, 28 and 40;
- vulgar (ordinary) warts are usually located on the hands, but can appear in other places. Such warts are painless and are small lumps with a diameter of 1–4 mm. They can merge into large plaques. Common warts are caused by HPV type 27.
In conclusion, we note that folk remedies for treating warts do not have proven effectiveness, and are sometimes downright dangerous.
To remove skin tumors, it is best to immediately contact a professional. July 1, 2021
Author of the article: dermatologist Mak Vladimir Fedorovich
Types and danger of cervical papillomas
You should decide how to remove papillomas on the neck only after making sure that the skin growth is actually a papilloma. For this purpose, it is best to contact a specialist who, based on the results of PCR diagnostics and a simple examination, will make a final diagnosis. In general, it is quite difficult to confuse a papilloma on the neck with any other neoplasm. Characteristic signs of the viral nature of a skin growth are painlessness and external signs.
Papillomas protrude above healthy tissues, attaching to them through a thin stalk or large base. The consistency of papilloma can be moderately dense or soft, and the color varies from light pink to dirty brown.
Neoplasms of this localization can be vulgar or flat in appearance, and can also be small papillomas on the neck that have a yellow tint. It is believed that representatives of the stronger sex are more prone to such localization of epidermal growths.
The transformation of skin papilloma into a malignant tumor is unlikely, which cannot be said about the possibility of injuring, tearing or rubbing delicate tissue. Such mechanical damage is fraught with the following consequences:
- Severe bleeding (proliferation of the capillary network is usually observed around the papilloma);
- Infection of the wound surface (skin damage is an open gate for infection and microbial contamination);
- Autoinaculation (contamination of infected blood on healthy areas of the epidermis can lead to repeated self-infection, which is manifested by multiple “warts”);
- Formation of scars (the neck is an open part of the body, the aesthetic appearance of which is important in shaping the overall image).
Treatment.
And although we have already managed to find out that there is no harm from destroying this kind of pathology, still only the doctor chooses the treatment tactics (removal or therapy). So, self-medication can lead to complex disorders, including the formation of abscesses or sepsis.
Rice. 3 Soft fibroids on the neck.
Timely contact with a specialist will help to avoid the appearance of new formations, as well as the addition of various types of infections (bacteria, fungi).
Pharmacy counters have a wide selection of drugs aimed at combating papillomas:
- ointments, creams - they are applied specifically to the affected areas;
- adhesive tape - glued to an area strewn with many foci of infection;
- essential oils are convenient for those who have allergic reactions to the chemical composition of the above proposed products.
Other methods of combating papillomas.
- Electrocoagulation method – does not leave scars on the skin, is highly effective.
- Laser removal also has a high degree of efficiency, up to 94%.
- Destruction by influence of low temperatures - the method is less effective (about 65%), there is a possibility of relapse.
- Radio wave knife.
- Removal using special chemical compounds.
When choosing the optimal technique, a specialist is guided by a number of conditions: localization, appearance (shape, size).
What are warts
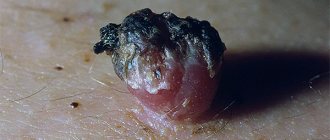
A wart is a skin disease that appears as small raised lesions about 10 millimeters in size. Less often - large size.
Warts on the neck are caused by the human papillomavirus. Symptoms: small convex formations on the skin of a normal color.
Diagnosis by examination, scraping examination. Treatment is local, using cauterizing agents, sometimes surgical.
They do not differ in color from skin, but are brown and red. The shape of the neoplasm resembles a nodule with or without a stalk. The number of warts is not limited, as is the location.
Removing warts with nitrogen
Cryodestruction is a method of removing warts by exposing them to liquid nitrogen.
Initially, they do not pose a threat to health, but they look unaesthetic. Their appearance affects the appearance of the neck and is accompanied by discomfort that occurs when it comes into contact with clothing.
Due to this, the warts are subject to friction. This provokes inflammation and pain, which leads to the need to remove them.
Attempts to cover them with clothing aggravate the situation, as they lead to injury, bleeding, and change in shape. This is unsafe, since the appearance of warts is not only a cosmetic defect, but also a threat of a benign growth developing into cancer.
Removing warts on the neck should under no circumstances be done at home, especially not with celandine.
This provokes the formation of scars and skin burns. The cause of numerous rashes in the neck area should be sought at an appointment with a dermatologist and immunologist.
Cosmetologist, dermatovenerologist, laser therapist
Nachoeva Irina Nasredinovna
7 years experience
Molluscum contagiosum or infectious molluscum
Molluscum contagiosum or infectious molluscum is a skin tumor of a viral nature, benign in nature. She's contagious. The main routes of transmission from a sick baby to a healthy one are through direct close contact. The second option for infection may be the use of shared hygiene items.
Another great place to catch this virus is swimming pools - humid air, skin contact and a large number of people contribute to this.
Not everyone is equally susceptible to the virus - usually children from the group of frequently ill people, allergy sufferers, and digestive problems are more likely to suffer. Children with skin problems are more likely to get sick when there are areas of damage - abrasions, scratches, dermatitis - then it is easier for the virus to penetrate the thickness of the skin.
Rashes can appear on any part of the body - face, arms, neck, legs, shoulders, abdomen and even genitals - they cannot only appear on the palms and soles, which is why they differ significantly from papillomas. Usually they are not complicated - but if the child picks or combs them, microbes can appear.
Of course, in the case of a typical course and manifestation in several children, there is no doubt, but sometimes the mollusk is difficult to recognize. Therefore, let a pediatric dermatologist make an accurate diagnosis and treatment.
Treatment of this viral disease consists of removing the tumors by a pediatric dermatologist (or a pediatric ophthalmologist, if the molluscum is on the eyelid) using anesthetics. Further, it is possible to prescribe antiviral agents and certain treatment of skin areas where there were previously nodules, to exclude the possible reappearance of tumors. The main preventive measures are timely diagnosis of this disease and its treatment; therefore, it is necessary to conduct preventive examinations.
Types of warts
The appearance of warts is not accompanied by significant symptoms. Initially, you can notice small spots on the skin, slightly different in color from the main skin.
The formed growths are of two types.
Flat
They can be round, oval or multifaceted. They protrude slightly above the surface of the skin (up to 2 mm). The volume reaches 2-5 mm. They are localized on the arms, legs, scalp, and less commonly on the neck. Formed singly or in groups. They differ in the possibility of new daughter growths growing directly on them. This makes their surface lumpy.
Hanging
At first it is a small knot on a thread-leg. As it grows, it looks like a tiny mushroom or flesh-colored nipple. The length of such warts ranges from 1 to 6 mm.
Their appearance does not bother a person, but causes discomfort when in contact with clothing. Most often, patients try to get rid of these papillomas for aesthetic reasons.
The absence of pain should not be a reason to ignore the appearance of warts of any kind, especially if their number is rapidly increasing. Such manifestations are a signal for examination of papillomas.
Flat warts: features and treatment options
In their clinical practice, doctors of various specialties often encounter human papillomavirus (HPV) - associated diseases of the skin and mucous membranes. The sharp increase in the infection rate of the population, the diversity of clinical pictures, and the characteristics of the course of these conditions arouse interest and active discussion about the tactics of managing such patients among a large number of clinicians. The relevance of the problem of HPV infection, along with the negative trend of spread, is associated with a significantly pronounced negative effect of the virus on the immune system, which leads to its long-term persistence, reluctance to therapy and frequent recurrence of the disease.
Papillomaviruses were allocated to a separate family Papovaviridae, which, according to modern concepts, consists of 16 genera, representatives of five of which are pathogenic for humans [1, 2]. Virions do not have an envelope; their diameter is 50–55 mm. The capsid has the shape of an icosahedron and consists of 72 capsomeres. The genome is represented by double-stranded circularly twisted DNA and includes about 8000 base pairs [3]. During the replication cycle, the viral genome expresses 8 to 10 protein products. Early proteins that control viral replication, transcription and cellular transformation are represented by oncoproteins E6 and E7. The E1 and E2 proteins regulate viral DNA replication and gene expression. Late proteins L1 and L2 are structural proteins of the virion. Protein L1 forms capsomeres [4]. Invasion of the virus occurs through microdamage to the skin and mucous membranes with infection of predominantly immature, dividing cells of the basal layer, followed by replication of the virus and assembly of viral particles in the differentiated cells of the surface layer of the epidermis/epithelium. The entire development cycle of the infectious process is closely associated with the division of cells of the integumentary epithelium of the skin and mucous membranes and is not accompanied by signs of inflammation. In this case, HPV can have a productive or transformative effect on the epithelium. With productive exposure, benign neoplasms arise - papillomas, warts and condylomas of the skin and mucous membranes. The result of the transformative effect is dysplasia of varying severity, the progressive development of which leads to cancer [5].
Currently, more than 100 types of HPV have been identified that can infect the skin and mucous membranes and provoke the development of changes characterized by papillomatous growths. The human papillomavirus has tissue specificity—the ability of certain types of HPV to infect tissue specific to their localization. In this case, the type of virus determines the clinical features of the infectious process.
One of the most common pathologies resulting from infection of the skin and mucous membranes with papillomaviruses are warts, which are benign epithelial tumors.
Among warts, there are 8 clinical varieties, each of them is associated with certain HPVs: vulgar warts (1–4, 27th, 29th, 57th HPV genotypes); deep palmoplantar warts (1st, 3rd, 27th, 29th, 57th); mosaic plantar warts (2nd, 4th); cystic warts (60th); flat warts (3rd, 10th, 28th); “butcher’s” warts (7th); focal epithelial hyperplasia (13th, 32nd); verruciform epidermodysplasia (5th, 8–10, 12th, 15th, 19th, 36th) [1].
The group spread of warts, as a result of direct and indirect contact with patients, is characterized by a high incidence rate, amounting to 7–12% in adults, and up to 10–20% in school-age children [1]. The incubation period varies from 1 to 6 months, but can be over three years. Within two years, up to 40–65% of warts regress on their own. In other cases, they continue to increase in size and over time may become more resistant to therapeutic effects [1, 6].
The most common types of warts encountered in clinical practice are vulgar and flat warts. Vulgar warts, which are predominantly caused by HPV types 2 and 4, clinically present as multiple painless dense round gray papules with a diameter of 0.2–0.5 cm with an uneven, keratinized surface of flesh-colored or yellow-brown color, most often located on dorsum of the hands. However, rashes can also be located on other areas of the skin [7].
Flat warts, most often localized on the back of the hands, forearms, face and mucous membranes, are clinically presented as small multiple papules the color of normal skin. They occur in any age category, but are especially common in children and adolescents.
Currently, there are quite a lot of methods for treating warts; they are divided into destructive, chemical, and immunotropic. Depending on the specific clinical situation, preference is given to a certain method of therapy.
The most common methods for removing warts are the use of salicylic acid and cryotherapy with liquid nitrogen. The manual by J. Sterling et al. salicylic acid has been named the drug of choice for the treatment of flat warts on the face, as well as flat and common warts on the hands. Over-the-counter medications contain less than 20% salicylic acid, while prescription medications may contain up to 70% salicylic acid. However, 15–20% salicylic acid is usually sufficient to cure a wart. The use of salicylic acid preparations is considered first-line therapy in the treatment of common non-genital warts [1]. The effectiveness of this effect is quite high; cure is observed in 70–80% of patients [1, 8].
Given the ability of retinoids to influence keratinization processes, accelerating wart removal, some authors recommend their use orally and topically as a second line in the treatment of flat warts [6, 9].
Of the destructive methods in practice, cryotherapy using liquid nitrogen applications is the most widely used. The method is based on rapid freezing of intra- and extracellular fluid, which is subsequently accompanied by cell death and lysis during thawing. Most researchers estimate its effectiveness at 70–75% and recommend its use in the treatment of flat and simple warts as first-line therapy. The method does not require anesthesia or special equipment, large material costs, and is quite simple to implement, which greatly facilitates its use.
Laser therapy, which leads to necrotization of the tissue area with the wart as a result of coagulation of blood vessels, according to some authors, leads to a positive result in up to 50–80% of cases, but the recurrence rate is quite high and amounts to 4–22% [10]. At the same time, it should be remembered that long-term non-healing wounds are fraught with the addition of a secondary infection and the formation of scars at the site of removal. Therefore, it is recommended to use laser for plantar warts as a second-line therapy, and for common and flat warts as a third-line therapy [9].
The ability of HPV to persist in the human body and the formation of secondary immunodeficiency makes it advisable to include in the complex of treatment of patients drugs that disrupt viral replication and improve regeneration. Therefore, in world practice, local agents with antiviral and immunomodulatory effects are widely used to treat warts, the effectiveness of which increases significantly when used sequentially or in parallel in combination with methods of destruction.
At the same time, despite the seemingly wide variety of methods for treating warts, none of them provides a one hundred percent guarantee of a complete cure for the patient. Until now, despite the fundamental discoveries and achievements of modern medicine, for papillomavirus infection, unlike other viral lesions of the skin and mucous membranes, there are no specific treatment methods with an almost complete absence of systemic therapy. Every year, the statistics of HPV-related diseases are steadily worsening, the frequency of recurrence of the pathological process remains high, which dictates the need to search for drugs and new techniques that increase the effectiveness of therapy. This problem becomes especially relevant when it comes to young patients, where it is necessary to eliminate the risk of unwanted drug reactions and complications as much as possible. According to many studies, the most effective method of treating HPV-induced skin tumors is a combination one, combining the simultaneous or phased use of local destructive effects and the systemic use of antiviral and immunoprotective agents. Since only destruction, according to a number of authors, gives a high percentage of relapses within six months, and warts in most cases appear on the same areas of the skin as before. This is probably explained both by the stages of the HPV life cycle, the DNA of which can be detected at a distance of up to 1 cm from the visible boundaries of the tumor, and by a violation of general and local immunity [4].
The purpose of this study was to evaluate the effectiveness and safety of combination therapy for flat warts in children, including the interferon drug Genferon Light and cryodestruction with liquid nitrogen.
Material and research methods
We observed 73 children aged 2 to 9 years with a diagnosis of human papillomavirus infection of the skin, with clinical manifestations in the form of HPV-induced flat warts. The duration of the disease varied from two months to 2.5 years. Almost 90% of children (65 patients) had previously been treated for this disease with local antiviral drugs for 2–3 months, without effect. Warts were localized mainly on the face and the back of the hands. The number of elements on the skin ranged from 2 to 9. All patients were divided into two groups, 35 and 38 children in the first and second, respectively.
In the first group, patients were treated with a destructive method using liquid nitrogen in the form of cryomassage. The applicator with a cotton swab was placed parallel to the surface of the skin and moved with rapid rotational movements with slight pressure over the treated area until the skin became slightly pale. The procedure was repeated 3–5 times depending on the patient’s skin reaction at short intervals (1–2 minutes). More pronounced, raised warts were frozen additionally, with the applicator positioned perpendicular to the lesion, without pressure, for 10–15 seconds, without affecting the surrounding skin. The number of procedures varied from 4 to 5–6. A repeat session was carried out after the reaction (hyperemia) caused by the procedure disappeared. The interval between procedures was 3–4 days.
In the second group, in addition to cryomassage (cryodestruction), an immunomodulatory drug with an antiviral effect, Genferon Light, was simultaneously prescribed according to the following regimen: 1 suppository rectally 2 times a day with a 12-hour break for 10 days before destruction and for 10 days after destruction, in appropriate cases age doses (a single dose for children under 7 years old was 125,000 IU, for children over 7 years old - 250,000 IU). Genferon light, specially created for a special category of patients (pregnant women and children), contains a reduced dose of active ingredients (interferon α-2b (IFNα-2b) at a dose of 250,000 IU and taurine at a dose of 0.005 g). IFNα-2 has pronounced antiviral, immunomodulatory and anti-inflammatory activity. The amino acid taurine has antioxidant and membrane-stabilizing properties, which significantly increases the biological activity of IFNα. All patients were recommended to wipe their skin with a 2% solution of salicylic alcohol as skin care during the treatment period. To prevent the occurrence of hyperpigmentation at the site of removed warts, it was recommended to avoid active insolation for 5–6 months and use sunscreen. The effectiveness of the treatment was assessed by the absence of clinical manifestations of the disease during the year.
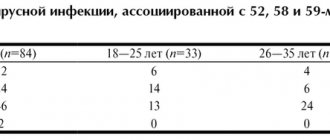
results
At the end of therapy, a complete absence of skin rashes (as a result of exfoliation of the stratum corneum along with warts) in the first group was observed in 23 children, which amounted to 65.7%. In 2 (5.7%) patients in this group, flat warts were partially preserved, in 6 (17.1%) children there was a relapse within 1–2 months, in 4 (11.5%) there was a relapse within six months, which required in the future, additional therapy will be prescribed in the form of a combination of cryodestruction with the immunomodulatory drug Genferon light.
In patients of the second group, who received Genferon Light in addition to cryomassage, the effectiveness of therapy was 92.1% (35 children), relapse was recorded in 3 (7.9%) children by the end of the year of clinical observation, and reinfection could not be excluded.
Tolerability of Genferon Light was good in all children. No side effects from the therapy were recorded.
Thus, the inclusion of the immunomodulatory drug with antiviral effect Genferon Light in the complex treatment of flat warts in children can significantly increase the effectiveness of therapy, avoid complications and unwanted drug reactions, which is extremely important in this category of patients.
Literature
- Khlebnikov A.N., Selezneva E.V., Dorokhina O.V. // Bulletin of Dermatology and Venereology. 2015. No. 1. pp. 122–128.
- Manykin AA Papillomavirusa // Medical virology under editions Lvova DK 2008. P. 269–276.
- Kungurov N.V., Kuznetsova Yu.N., Gorbunov A.P., Tolstaya A.I. Combined method of treatment of palmoplantar warts // Pharmacotherapy in dermatovenerology. 2011. No. 2. P. 62–69.
- Molochkov A.V., Khlebnikova A.N., Lavrov D.V., Gureeva M.A. Genital papillomavirus infection. Tutorial. 2010. 10 p.
- Rogovskaya S.I. Human papillomavirus infection in women and cervical pathology. M.: GEOTAR-Media, 2005. pp. 15–17.
- Belyaev V.V., Myasnikov L.L. Plantar, flat, vulgar warts: modern approaches to treatment // Clinical dermatology and venereology. 2012. No. 6. P. 55–58.
- Stirschneider Yu. Yu., Volnukhin V. A. // Vest. dermatology and venereology. 2013. pp. 65–70.
- Cockayne S., Hewitt C., Hicks K. et al. EVerT Team. Cryotherapy versus salicylic acid for the treatment of plantar warts (verrucae): a randomized controlled trial // Br. Med. J. 2011: 342: d3271.
- Bacelieri R., Johnson S. Cutaneous Warts: An Evidence-Based Approach to Therapy // Am Fam Physician. 2005, Aug 15; 72(4):647–652.
- Mavrov G.I., Shcherbakova Yu.V., Chinov G.P., Nagorny A.E. Methods for diagnosing and treating skin lesions caused by the human papillomavirus // Dermatology and Venereology. 2010. No. 2. P. 49–60.
E. I. Yunusova1, Candidate of Medical Sciences L. A. Yusupova, Doctor of Medical Sciences, Professor G. I. Mavlyutova, Candidate of Medical Sciences Z. Sh. Garayeva, Candidate of Medical Sciences
GBOU DPO KSMA Ministry of Health of the Russian Federation, Kazan
1 Contact information