The high prevalence of human papillomavirus infection (PVI) and its proven role in the development of malignant neoplasms of the genital organs indicate the relevance of this problem. Currently, more than 150 types of human papillomavirus (HPV) are known, 40 of which cause diseases of the anogenital area. According to the degree of carcinogenic risk according to the IARC (International Agency for Research on Cancer) classification, in 2012 three groups of HPV were identified: carcinogenic - 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 and 59 -th (1st group), probably carcinogenic - 26, 30, 34, 53, 66, 67, 68, 70, 73, 82, 69, 85 and 97th (2nd group: 2A, 2B), non-carcinogenic - 6, 11, etc. (3rd group). All types are divided into specific phylogenetic groups. Of greatest clinical interest is the phylogenetic group α, which includes the following types of high-oncogenic risk HPV (HR HPV): α5 (HPV 51), α6 (HPV 56), α7 (HPV 18, HPV 39, HPV 45, HPV 59), α9 (HPV 16, HPV 31, HPV 33, HPV 35, HPV 52, HPV 58) [1, 2]. Separation into groups is important for dynamic monitoring of viral infection and more accurate prediction of its development, since different types of HPV have different oncogenic potential, as well as the ability to persist [3, 4].
It is known that the prevalence of various HPV genotypes varies both in different regions of the world and in Russia. Currently, “European” (16, 18, 31, 33, 45, etc.) and “Asian” types of HPV (52, 58, 59, 65, etc.) are conventionally distinguished. HPV types 52 and 58 belong to the phylogenetic group α9, HPV type 59 belongs to the α7 group (both groups are the most virulent for the cervical epithelium), and these types of viruses are of great clinical interest [5]. It should be noted that HPV types 52 and 58 20 years ago were extremely rare or not encountered at all, while currently their share ranges from 5.7 to 30.8% [6]. It was found that the risk of developing squamous cell carcinoma according to the IARC classification is higher for HPV types 52 and 58, type 59 is 1.08, the risk of developing adenocarcinoma is higher for HPV type 59.
According to a 2012 meta-analysis, including 437 studies, the following data were obtained: for HPV type 52, the overall infection rate was 8%, the number of cases of detection of HPV type 52 in CIN I was 13.8%, in CIN II - 16, 4%, CIN III - 10.2%, with invasive cancer - 3.5%. The overall prevalence of HPV type 58 was 6.3%, for CIN I - 9.6%, CIN II - 12%, CIN III - 9%, and for invasive cancer - 4.4%. HPV type 59 has a prevalence of 3.1%, with CIN I the detection was 5%, CIN II - 4.7%, CIN III - 2.2%, with invasive cancer - 1.3% [7]. According to the literature, there are conflicting prevalence rates of “Asian” HPV types in cervical cancer (CC). Thus, the prevalence of HPV type 52 in invasive cases ranges from 2.2 to 27% [8-15], HPV type 58 was found from 1.6 to 28.5% [5, 8, 10, 11, 13, 16 , 17], HPV type 59 - in 0.5-2.2% of cases [11, 12].
The changing epidemiological situation regarding HPV, along with changes in the structure of CIN in recent years [1, 6, 18, 19], dictates the need to continue studying the prevalence and role of HPV types with high oncogenic potential in CIN. Data on the frequency of detection of “Asian” types of HR HPV, including types 52 and 58, and their role in the development of precancerous diseases of the cervix in the Russian female population are scarce. Domestic authors have shown that HPV types 52 and 58 are the cause of abnormal cytology in 22.4% [20].
The purpose of the study was to determine the characteristics of the course of cervical PVI associated with HPV types 52, 58 and 59.
Material and methods
As a result of targeted selection, the prospective study included 84 patients aged 18–58 years with cervical cancer caused by types 52, 58 and 59 of HPV, examined at a specialized appointment for cervical pathology at the Omsk antenatal clinic. The average age of infected patients was 29.9±1.0 years (median and interquartile range - 27 (23.0-32.5 years). Inclusion criteria for the study: age from 18 to 60 years, positive cervical HPV test for the presence of Types 52, 58 and 59, informed consent of the patient.Exclusion criteria: pregnancy and lactation, refusal to participate in the study.
Comprehensive diagnostics included liquid-based cytology (Bethesda, 2001); colposcopic examination; histological examination of cervical biopsies and endocervical samples and advanced screening for differential detection of HPV DNA, including determination of HPV HR types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58 and 59 by polymerase chain reaction (PCR) in real time (RealBest DNA test system HPV HCR genotype) [1]. When interpreting the HPV viral load, we took into account the threshold of clinical significance - 3 lg per 105 cells, the threshold of progression (more than 5 lg per 105 cells) [21].
Statistical analysis of the data was carried out using the Statistica 6 package and MS Excel capabilities. In all statistical analysis procedures, the critical significance level p
was taken equal to 0.05.
The normality of the distribution was checked using the Shapiro-Wilkie test, and the hypothesis about the equality of general variances was tested using F
test.
Average sample values of quantitative characteristics are given in the text as M±SE
, where
M
is the sample mean,
SE
is the standard error of the mean. When values were distributed in a series other than normal, the median (P 0.5), 25th percentile (P 0.25), and 75th percentile (P 0.75) were indicated. When analyzing contingency tables, the values of Kullback's information statistics were assessed (statistics 2I).
Treatment of papillomavirus
Unfortunately, medicine is not yet able to completely rid the body of the virus. Therefore, the task of the doctor and the patient is to deal with the consequences in a timely manner. It is recommended to remove all warts and treat precancer and cancer stages. According to recent studies in the USA, the human immune system is able to cope with HPV on its own within 2 years after infection in 90% of cases. If this does not happen, treatment is strictly necessary. Papillomas are removed using the following methods:
- Surgical removal
is an outdated but effective method. Recommended in exceptional cases. - Electrocoagulation
– cauterization of affected areas with electric current. Not everyone likes the method, as it can also affect healthy tissue. - Laser coagulation
- laser cauterization - is the most modern and effective method that gives a minimum of complications. - Cryodestruction with liquid nitrogen
differs from other methods in that the pathological growth is affected by cold. Requires a lot of experience from the doctor. - Chemical cauterization
- the doctor acts on the diseased area with concentrated acids or alkalis. The method can also affect healthy skin - the chemical will leave a scar. - The radio wave method
is the most expensive, but the best. Does not cause pain, complications, bleeding. Does not leave scars.
You can read more about methods for removing tumors in the “Low-traumatic operations” section.
After removal, antiviral treatment and means to restore and strengthen the immune system are prescribed.
results
79.8±4.4% of patients in the observation group were under the age of 35 years (inclusive). The distribution of cervical infection with HPV types 52, 58 and 59 depending on age was as follows: early reproductive age (18-25 years) - 33 patients, middle age (26-35 years) - 34, over 36 years - 17.
An analysis was carried out of the frequency of HPV-associated lesions of the cervix, which are divided into clinical (exophytic condyloma), latent (lack of clinical, morphological changes when HPV DNA is detected), subclinical form (invisible to the naked eye, asymptomatic, detected only by colposcopy and/or morphologically) , CIN I-III degrees and cervical cancer [1]. There were no cases of clinical PVI. Among the infected women, there were patients with CIN (46-54.8%), a relatively latent form of infection without clinical manifestations (12-14.3%), a subclinical form of infection (24-28.6%) and cervical cancer (2-2 ,4%).
Depending on the severity of the histologically verified precancer, CIN I was detected in 51.2%, CIN II in 32.5%, and CIN III in 16.3% of cases.
When analyzing the frequency of forms of PVI associated with the types studied depending on age, attention was drawn to the absence of significant differences in the latent form in all age groups ( p
>0.05) (Table 1).
In turn, in the presence of cervical pathology, the influence of the age factor is clearly manifested. Thus, the subclinical form of PVI was dominant in patients of early reproductive age compared to that in patients aged 26–35 years ( p
= 0.05), in whom a predominance of CIN was noted (
p
= 0.02).
There were no significant differences in the severity of CIN (grades I–III) depending on age. Two cases of cervical cancer associated with HPV type 58 were observed in a group of women over 36 years of age. A direct, weak, statistically significant correlation between the form of PVI and age was established (rS=+0.21; p
=0.0517).
Table 1. Forms of human papillomavirus infection associated with types 52, 58 and 59, depending on age
When studying the nature of infection (mono-, combined), it was found that infection of the cervix with the participation of one of the studied types of HPV was observed in 37 (44 %) of patients: type 52 - in 19, type 58 - in 13, type 59 - in 5 (Table 2). In 44 (52.4%) women there was a combination with other types of HR HPV 16, 18, 31, 33, 35, 39, 45, 51 and 56 (the most common types were 16, 31 and 56), in In three cases, a combination of two of the 52, 58 and 59 types was noted.
Table 2. Frequency of detection of HPV types 52, 58 and 59 in women with PVI
Particular attention was paid to monoinfection of the studied HPV types. Among 37 women in whom one of the types was identified (52, 58, 59), the distribution of forms of the disease was as follows: latent - in 5 patients, subclinical - in 12, CIN - in 19, cancer - in 1. Cervical neoplasia (CIN and cervical cancer) amounted to 20 (54%) cases with monoinfection, and 28 (59.6%) cases with the combined form, which did not have statistically significant differences ( p
=0.3973). Frequency of CIN with monoinfection of type 52 - 6 observations out of 19 of this type, with monoinfection with HPV type 58 - 10 out of 13, with monoinfection with HPV type 59 - 3 out of 5 observations, CC (1 case) - with monoinfection with HPV 58 type (Fig. 1).
Rice.
1. Distribution of HPV-associated lesions of the cervix in mono- and combined forms of infection. The viral load of HPV types 52, 58 and 59 was assessed among 84 infected women (including mono- and co-infection) (Table 3). In 30 cases, its level was below the threshold of clinical significance, in 30 cases the viral load of HPV types 52, 58 and 59 was in the range from 3 to 5 lg per 105 cells, in 33 cases the viral load was above the progression threshold. Exceeding the progression threshold varied in the range of 25–46.7% depending on the HPV type (Fig. 2).
Table 3. Distribution of viral load levels by HPV type in the group of examined patients (mono- and combined infection) Note. *Here and in the table. 4: the number of viral load observations did not coincide with the number of patients examined due to co-infection.
Rice. 2. Viral load of HPV types 52, 58 and 59 in women with PVI.
When analyzing the relationship between clinical forms of PVI and the level of viral load, a twofold excess of cases with a load exceeding 5 lg per 105 cells was found in women with CIN: 25 versus 10 (less than 3 lg per 105 cells) and 11 (from 3 to 5 lg per 105 cells) cases, p
=0.0091 (Table 4).
Table 4. Dependence of the form of PVI in HPV types 52, 58 and 59 (mono- and combined infection) on the viral load.
In the case of monoinfection, the latent form was not accompanied by a load above the progression threshold, the subclinical form occurred against the background of exceeding the progression threshold in 1 case against the remaining 11, while CIN and CC - in 13 versus 7 cases with a lower viral load (Table 5). A statistically significant relationship was established between the severity of PVI and the level of viral load of types 52, 58 and 59 (2I=16.29; p
<0,05).
Table 5. Forms of PVI in monoinfection with HPV types 52, 58 and 59
According to studies based on large clinical material, among various age groups, an increase in the level of viral load increases the severity of HPV cervical damage [5, 20, 22-24]. According to a study by G. Shen et al. [25], a positive correlation was noted between the level of viral load and the degree of cervical lesions. Our data proves the influence of the viral load for HPV types 52, 58 and 59 on the progression of cervical neoplasia.
Papilloma virus - diagnosis
Human papillomavirus can be detected in its early stages only by laboratory methods. The infection can be detected visually only when condylomas or papillomas appear. If HPV is suspected, the following are prescribed:
- Gynecological examination
or examination by a urologist with taking smears for an HPV test. If condylomas are detected, urethroscopy is performed. In case of cervical erosion, the gynecologist must take a smear for oncocytology. - If HPV is detected, a colposcopy is required - examination of the vagina and cervix with a gynecological microscope - colposcope. The doctor uses special tests to exclude hidden pathologies.
- Colposcopy with biopsy.
Indicated for all women with neoplasia. At the same time, coloring and exposure to suspicious areas is carried out. A sign of APC may be whitish areas formed after treatment with vinegar, uneven accumulation of iodine when exposed to Lugol's solution, a mosaic pattern, and protrusions of the epithelium. - Histological and cytological examination
- assessment of the cellular composition, and the cells themselves, for atypicality (cancer). - PCR – search for traces of papillomavirus DNA. This is the most accurate and diagnostically informative analysis that detects the papilloma virus in men and women and specifies its type.
To assess the viral load, a quantitative HPV test is recommended, which determines the critical concentration of the virus associated with the risk of malignancy of tumors. The analysis is also carried out to assess the effectiveness of treatment.
conclusions
1. Among the cohort of women with human papillomavirus infection of the cervix associated with HPV types 52, 58 and 59, a significant proportion of women are under 35 years of age (79.8%).
2. The age-dependent nature of the frequency of subclinical infection and cervical neoplasia in infected women has been established.
3. Human papillomavirus infection associated with HPV types 52, 58 and 59 was accompanied by the presence of CIN and cervical cancer in 57.1% of cases.
4. High frequency of cervical neoplasia during monoinfection (54%), comparable to its frequency when combined with other types of HR HPV (59.6%; p
>0.05), as well as the relationship between the severity of the lesion and the level of viral load, confirm the high risk of the formation of precancer and cervical cancer in the presence of monoinfection with HPV types 52, 58 and 59.
Symptoms of papillomavirus
HPV infection can be asymptomatic or give the following symptoms:
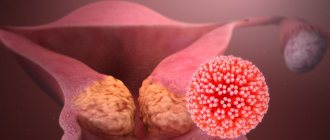
Genital warts (genital warts)
Fibroepithelial (skin) neoplasms with a thin stalk or a broad base. They can be single or merge, forming a growth that looks like a cauliflower head. Condylomas can become inflamed and bleed when injured, as they contain blood vessels that feed them.
Condylomas can be found on the clitoris, labia minora, urethra, vagina, cervix, around the anus and in the anus. Exophytic forms of OC are a consequence of the activity of benign types of the HPV virus - 6, 11. Endophytic condylomas (flat and inverted) grow on the cervix and initially do not give symptoms. Detected during extended colposcopy. Genital warts affecting the lips, tongue and palate are visible during routine examination.
People with HIV and during pregnancy develop very large genital warts. Giant Buschke-Levenshtein condyloma is not uncommon.
- Anal warts.
Anal warts can be found up to the dentate line of the rectum. At first they do not cause discomfort, but over time they itch, hurt, and smell unpleasant. - Urethral warts.
In women, the external urethral opening is affected in no more than 8%. Such warts are easily identified by a gynecologist. Deep damage to the urethra (urethra) cannot be determined visually, but the disease gives symptoms of sluggish urethritis. Urethral warts in men cause a split urine stream associated with a narrowing of the urethral opening.
Flat condylomas
Flat condylomas do not protrude above the surface of the mucous membranes, which is why they got their name. These formations have a high oncogenic potential. Most often, flat condylomas are located on the cervix and vaginal mucosa. Flat condylomas can only be detected by colposcopy.
Dysplasia, cervical cancer
Dysplasia is a tissue pathology associated with the modification and degeneration of cells. This is a precancerous condition. There are 3 degrees of the disease, all of which are detected by colposcopy. Stages 2 and 3 require surgical treatment. Cervical dysplasia is preceded by cervical erosion.
Cervical cancer is a consequence of dysplasia. It is the most common tumor of the female reproductive organs. It may be asymptomatic or cause pain, bleeding and other symptoms characteristic of problems with the female reproductive system.
Where is papillomavirus treated in St. Petersburg, prices
You can contact the Diana private clinic in St. Petersburg for diagnosis and treatment of papillomavirus. We use modern methods approved in the best European clinics, and the prices for specialist services are quite affordable.
Here you can get tested for the human papillomavirus and remove any tumors. Removal of formations associated with HPV is carried out using the latest Fotek radioknife with a coagulator that prevents bleeding. Price for removal of condylomas, papillomas, etc. — from 500 rub. We also offer the HPV vaccine with Gardasil.