Melanoma is a malignant tumor that develops from the transformation of melanocytes, the pigment cells of the skin. This formation occurs primarily on the skin, but can also form in the mucous membranes (oral cavity, vagina, urethra, bladder), as well as in the eyeball.
- Clark stages of melanoma
- Melanoma stages according to TNM
- Classification of melanoma according to T criterion
- Classification of melanoma according to criterion N
- Classification according to criterion M (presence of distant metastases)
- 4 clinical stages of melanoma
- Metastases
- Survival forecast by stage
Determining the stage of melanoma is crucial for determining the prognosis of the disease and choosing treatment tactics. For example, in the early stages, surgical excision of the tumor is sufficient to achieve a good result. In case of a widespread process, treatment is supplemented with immunotherapy and targeted therapy. At stage 4, when there are metastases to internal organs, chemotherapy can be used to prolong the patient’s life.
The following methods are used to determine the stage of melanoma:
- Histological verification of melanoma and determination of the degree of its invasion into the layers of the skin and subcutaneous tissue.
- Determination of the presence of regional and distant metastases. For this purpose, medical imaging methods are used (CT, MRI, PET, ultrasound), as well as biopsy of lymph nodes and suspicious lesions.
What is melanoma?
Melanoma is a malignant tumor that occurs as a result of excessive proliferation and degeneration of skin pigment cells - melanocytes (Fig. 1).
In the vast majority of cases, this tumor is located on the surface of the skin, but it can also affect the mucous membranes and some organs, such as the eyes and intestines. Melanoma is a relatively rare type of malignant neoplasm. According to statistics, in the Russian Federation it occurs in 1-3% of adults and less than 1% of children. But in recent years, the number of cases of melanoma in children has been increasing.
Cancer of this type occurs in all age groups, most often between the ages of 11 and 15 and from 40 to 60 years [1], mainly among women. People living in southern countries and regions with increased solar activity are more susceptible to the disease, since ultraviolet radiation increases the risk of skin tumors.
Melanoma has the highest mortality rate among all cancers. According to WHO, about 48,000 people die from melanoma every year worldwide.
Figure 1. Skin structure. Source: Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436 (Creative Commons Attribution 3.0 Unported license)
Table of contents
- Etiology and pathogenesis
- Clinical manifestations
- Diagnostic imaging of melanoma
Melanoma is a tumor caused by malignant transformation of pigment-producing cells (melanocytes). Melanocytes originate from the neural crest, whose cells have a high ability to migrate throughout the body. So while melanomas usually occur on the skin, they can also appear in other places where neural crest cells migrate—for example, in the gastrointestinal tract or brain.
In our company you can purchase the following equipment for diagnosing melanoma:
- FotoFinder dermoscope Vexia (FotoFinder)
- FotoFinder ATBM bodystudio (FotoFinder)
- FotoFinder (FotoFinder)
- Handyscope (FotoFinder)
Melanoma predominantly affects adults; no gender specificity has been identified for the disease. Internationally, the incidence of melanoma varies greatly. Thus, white populations in Australia, New Zealand, South Africa and the southern United States have the highest rates of this malignant tumor, while Asian populations in Hong Kong, Singapore, China, India and Japan have the lowest. This suggests that people with skin phototypes I–III who live in sunny regions of the world are at significant risk of developing this malignant tumor.
One study found that from 1995 to 2012 in Europe, the average annual incidence of invasive melanoma increased by 4.0% in men and 3.0% in women, and the incidence of in situ melanoma by 7.0%. 7% and 6.2% respectively. It is also noted that the risk of a second melanoma after the first is detected is 3–5%.
In Russia, the situation with melanoma, as well as with other malignant neoplasms of the skin, is quite complex - and from year to year it does not get easier. Thus, in 2016, skin cancer was diagnosed in 74,700 people, and melanoma in 10,500 people. Already in the next year, 2022, 78,000 cases of skin cancer and 11,200 cases of melanoma were recorded - an increase of 4.6% ( Fig. 1 ).
Interestingly, in 2016 the prevalence of melanoma was 59.3 cases per 100,000 population, but in 2006 (10 years ago) it was only 39.7 cases per 100,000 population. In total, about 500,000 people in Russia are currently diagnosed with skin cancer, which is 0.347% of the country's population.
Rice. 1. Statistics of cancer diseases in Russia as of 2022 (Ministry of Health of the Russian Federation, RBC)
Causes of melanoma
Melanoma develops as a result of atypical reproduction and malignant degeneration of melanin-producing skin cells (melanocytes), which are normally responsible for the color of the skin.
Normally, skin cells develop in a controlled and orderly manner: new healthy cells push old ones to the surface, where they die and eventually slough off. But when DNA damage occurs in some cells, new cells can begin to grow uncontrollably, leading to tumor formation.
It is currently unclear what exactly damages DNA in skin cells and how exactly this leads to melanoma. This is believed to be the result of many environmental factors. However, doctors believe that exposure to ultraviolet (UV) radiation from the sun, tanning lamps and tanning beds is one of the key causes of melanoma.
However, ultraviolet rays are not a trigger for all melanomas, especially those that occur on covered areas of the body that are not exposed to sunlight. This indicates that other factors may also influence tumor development [3].
Who is at risk?
Although the exact causes and mechanisms of melanoma development are still being studied, risk factors that are associated with malignant degeneration of skin pigment cells have already been clearly identified.
Among them [3]:
- Bright skin. Less pigment (melanin) makes the skin more susceptible to ultraviolet radiation. People with blond or red hair and blue eyes are thought to be more likely to develop melanoma than people with dark skin color.
- Previous sunburn. One or more severe sunburns that cause blistering may increase the risk of melanoma.
- Excessive exposure to ultraviolet radiation. UV radiation from the sun and tanning beds increases the risk of skin cancer.
- Accommodation in the equatorial zone. People living closer to the Earth's equator receive higher doses of ultraviolet radiation than residents of northern or southern latitudes.
- A large number of moles (nevi). Having more than 50 common moles on your body indicates an increased risk of developing melanoma.
- Family history of melanoma. The likelihood of developing melanoma is higher in people who have close blood relatives who have experienced this pathology.
- Frequent traumatization of nevi. These could be injuries sustained during shaving, as a result of wearing jewelry, underwear or other items of clothing (for example, backpack harnesses). In such cases, the risk of malignant degeneration reaches 90%2.
- Weakened immune system. People with compromised immune systems have an increased risk of melanoma and other skin cancers. Most often this is associated with taking medications to suppress the immune system, for example, after organ transplantation or in autoimmune pathologies and HIV infection.
Classification and stages of melanoma development
In clinical practice, the international classification of melanomas according to the TNM system of the American Joint Commission on Malignant Neoplasms is used. It is used for many malignant tumors. The assessment takes into account the prevalence of the tumor and the presence of metastases:
- T—primary tumor. Classified depending on the thickness of the germination, the presence or absence of ulceration. It is determined after histological examination of a tumor tissue sample.
- pT—primary tumor.
- pTX—the primary tumor cannot be assessed.
- pT0—no data on the primary tumor.
- pTis - melanoma in situ (I level of invasion according to Clark) (atypical melanocytic hyperplasia, severe melanocytic dysplasia, non-invasive malignant lesion).
- pT1 is a melanoma 1 mm thick or less (pT1a is Clark grade II or III without ulceration, pT1b is Clark grade IV or V or with ulceration).
- pT2 - melanoma with a thickness of more than 1 mm, but not more than 2 mm (pT2a - without ulceration, pT2b - with ulceration).
- pT3 - melanoma more than 2 mm thick, but not exceeding 4 mm (pT3a - without ulceration, pT3b - with ulceration).
- pT4 - melanoma more than 4 mm thick (pT4a - without ulceration, pT4b - with ulceration).
- N - reflects the involvement of lymph nodes in the pathological process.
- Nx - there is no reliable data for a correct assessment.
- N0 - there are no signs of lymph node damage.
- N1 - metastases in lymph nodes up to 3 cm in size.
- N2a - metastases more than 3 cm.
- N2b - the presence of metastases in the skin or subcutaneous fat, located at a distance of more than 2 cm from the main tumor (transit metastases).
- N2c - the presence of metastases in lymph nodes larger than 3 cm in combination with transit metastases.
- M - presence of distant metastases (extending beyond the anatomical area).
- Mx - there is no data to determine the presence of distant metastases.
- M0 - distant metastases are not detected.
- M1a - distant metastases in the lymph nodes, skin or subcutaneous fat.
- M1b - presence of metastases to internal organs.
The depth of ingrowth (vertical growth) of melanoma is divided into 5 levels of invasion according to Clark:
- Level I - non-invasive tumor limited to the epidermis;
- Level II - tumor cells are located in the papillary layer of the dermis;
- Level III - tumor cells are located between the papillary and reticular layers;
- Level IV - tumor cells are found in the reticular layer of the dermis.
- Level V - tumor cells are found in subcutaneous fat.
Based on the above criteria, the clinical stage of melanoma is determined (Fig. 2).
Figure 2. Stages of melanoma development. Source: Alexilus / Depositphotos
How dangerous is melanoma?
Melanoma is the most dangerous type of malignant neoplasm. Without early diagnosis and treatment, this tumor quickly spreads to internal organs through the lymphatic and blood vessels.
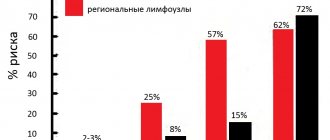
The tendency to form metastases depends on the biological characteristics of melanoma. When the tumor thickness is more than 1 mm, intradermal metastases are detected in 12.4% of cases. Moreover, a tumor larger than 4 mm is associated with a five-year survival rate of at least 50%. This means that even with full treatment in such cases, only half of the patients survive more than 5 years from the date of diagnosis. With confirmed metastatic damage to internal organs, this figure drops to 7-10%.
Metastases in melanoma occur in regional lymph nodes, liver, lungs, brain, bones, kidneys and adrenal glands. Moreover, often the reason a person seeks medical help is symptoms of damage to these organs, for example, headache or back pain, cough or shortness of breath, etc.
Liver metastases
The spread of melanoma cells to the liver leads to the formation of metastases. Changes are happening quite quickly. Secondary liver damage can be represented by a single metastatic focus, as well as multiple disseminated forms. Clinical manifestations of melanoma metastases to the liver will depend on the volume and location of the process. Symptoms are presented:
- pain in the right abdomen;
- yellowness of the skin and mucous membranes;
- tuberous compaction in the right hypochondrium;
- loss of appetite;
- significant weight loss;
- nosebleeds.
In this case, there is a significant increase in the volume of the liver and spleen, and the biochemical composition of the blood changes.
Melanoma symptoms
Melanoma can appear in different ways, depending on size, location, color and other characteristics. A common feature is a slight elevation above the level of adjacent skin areas and the formation of small satellite tumors.
Shape options vary widely: from round to triangular and irregular shapes, sizes - from a few millimeters to 2-3 centimeters. The color is in most cases red or dark brown, but black, purple, gray and pink tumors are found, as well as depigmented variations and combinations thereof. The consistency is often dense, less often elastic. Ulceration and bleeding may occur on the surface of the tumor even with the slightest external influence.
Depending on the characteristic signs, it is customary to distinguish 4 main clinical variants of melanoma (Fig. 3):
- Superficial spreading melanoma. The most common option, accounting for about 70% of all cases. It debuts as a brown spot, then gradually increases in size, loses symmetry, structure and changes color to a darker one. It has a long course with horizontal growth - up to 7 years. With vertical spread, accompanied by elevation above the adjacent skin, metastases quickly occur in the internal organs.
- Nodular melanoma. Outwardly it resembles a polyp or node, has a dense consistency and symmetrical shape, blue-red or brown, black color. It is characterized by rapid growth, during which small ulcers may appear on the surface of the tumor.
- Lentigo melanoma. It looks like a spot of irregular shape and uneven color. Occurs more often in older people. The basis for its development is the long course of lentigo maligna (precancerous melanosis of Dubreuil).
- Amelanotic or amelanotic melanoma. A characteristic feature is the lack of rich color, which is why the tumor often looks like a pink or flesh-colored papule.
Figure 3. Types of melanoma.
Sources: PLoS ONE 8 (12): e81205. DOI:10.1371/journal.pone.0081205. ISSN 1932-6203 (Creative Commons Attribution 4.0 International license), DermNetNZ / Wikipedia (Creative Commons Attribution 4.0 International license), Omar Bari, Philip R. Cohen / Cureus. DOI:10.7759/cureus.1026. ISSN 2168-8184 (Creative Commons Attribution 3.0 Unported license), Diagnostic Pathology (Creative Commons Attribution 4.0 International license), Anais brasileiros de dermatologia / Open-i (Attribution-NonCommercial 3.0 Unported). Inset header
How to distinguish melanoma from a mole?
In more than 70% of cases, melanoma develops at the site of an existing accumulation of melanocytes - moles or pigmented nevus. Malignant degeneration can be recognized in a timely manner using the ABCDE scale (Fig. 4) [2]:
- A - asymmetry, asymmetry. Normal moles, unlike melanoma, are symmetrical. This change can be determined by drawing an imaginary line between the two halves of the skin formation.
- B - border irregularity or change in edge or contour. Normally, in pigmented skin formations the edge is smooth and clearly defined. Melanoma is characterized by a lack of clarity, blurriness, and the appearance of “flames” at the borders with normal skin.
- C - color, color. Almost all moles are uniformly dark red or brown in color. Changes in the color of a mole, especially its individual parts, are often a manifestation of melanoma.
- D - diameter, diameter. Moles can vary in size, but usually they are no more than 5-6 mm in diameter. Exceeding these values, especially if it occurs over a relatively short period of time, is regarded as a sign of melanoma.
- E - elevation, elevation. Developing melanoma in most cases is slightly raised above the surrounding skin.
Figure 4. Mole or melanoma?
Source: NCI / Wikipedia In addition to melanoma, there are other, non-melanoma types of skin cancer. They may be accompanied by the following symptoms, which do not go away for at least 4 weeks:
- White, red or pink space-occupying formation.
- Discolored spots on the skin.
- Scaly skin or thickening of the skin.
- Scabs or sores that bleed, hurt, or itch.
Symptoms
In most cases, melanoma develops from a mole (nevus). Early signs of a tumor include:
- horizontal increase in size of moles - growth in width over the surface of the skin;
- changes in the boundaries of the nevus - they become uneven, blurred, asymmetrical;
- change in the color of the mole, the appearance of heterogeneity (black, brown and other areas on one nevus), light spots in and around it.
These signs do not always indicate the development of skin melanoma. On the other hand, at a very early stage, the symptoms of the disease are easy to miss with the naked eye. Therefore, it is important to consult a doctor when the first signs or even suspicions appear. Timely treatment can save the patient's life.
Late symptoms:
- vertical growth - the formation rises above the surface of the skin;
- peeling, itching, pain, bleeding of the surface of the nevus;
- enlargement of regional and distant lymph nodes.
Sometimes people, especially those who are characterized by increased anxiety, begin to suspect melanoma, mistaking it for ordinary moles. There is another extreme - patients ignore the initial signs of melanoma, considering them a newly appeared or injured nevus, age-related pigmentation. It is important to distinguish a mole from a malignant formation.
Moles usually have a smooth surface and even, symmetrical edges. Their color varies from light brown to dark brown, it is uniform, without light or dark inclusions. The normal size of a mole is considered to be up to 6 mm in diameter (you can use a pencil eraser as a guide). Moles extremely rarely change their size, and they are not characterized by unpleasant or painful sensations.
Diagnostics
Diagnosis of melanoma is based on the collection of medical history, examination of the skin, histological examination and, if necessary, additional diagnostic diagnostic methods.
The key test for detecting melanoma is dermatoscopy, performed using a dermatoscope that magnifies the suspicious skin lesion many times over. It allows you to identify the earliest signs of a malignant tumor and determine further tactics for managing the patient.
A tissue biopsy is required to confirm the diagnosis. The sample can be taken using a fingerprint smear or complete removal of the lesion within healthy tissue, which depends on the specific situation. In this case, partial tissue sampling is contraindicated, as this can cause tumor metastasis.
Also, depending on the characteristics of the identified tumor, the following may additionally be carried out:
- Ultrasound examination (ultrasound) of nearby lymph nodes.
- Computed tomography (CT) of the brain, abdominal and/or thoracic organs with intravenous administration of a radiocontrast agent, positron emission tomography (PET).
- Serological diagnosis: determination of the level of tumor marker S-100, lactate dehydrogenase (LDH).
- Genetic research: detection of mutations in the BRAF, CKIT genes.
Treatment of melanoma
The goal of the treatment is to remove the skin tumor and regional metastatically affected lymph nodes (if any). For this purpose, both surgical and medicinal methods are used, less often - radiation therapy.
The main treatment method for melanoma is surgical removal of the tumor. At stage I it is enough for complete cure. The peculiarity of operations for oncological pathologies is the removal of tumors within healthy tissues. Depending on the overall size of the tumor, the excision margin can range from 1 to 3 centimeters. The removed tissue is then sent for biopsy.
Drug treatment for melanoma is represented by immunotherapy. It is indicated for tumors more than 2 mm thick with ulceration, which corresponds to stages IIB and IIC, III and IV. For stages IIB and IIC, recombinant interferon alpha-2a,b (IFN-alpha) preparations are more often used. In stages III and IV, BRAF inhibitors (vemurafenib, dabrafenib), CTLA4 receptor blockers (ipilimumab), and anti-PD1 therapy are indicated. However, the treatment regimen is selected individually, depending on the patient’s condition, tumor characteristics and other parameters [1].
One of the modern options for drug treatment is targeted therapy. This is the targeted introduction of drugs into the tumor, due to which the death of cancer cells occurs with a minimum number of side effects. This approach may be recommended for melanoma if the cancer has spread to lymph nodes or other areas of the body.
For melanomas that cannot be completely removed by surgery, radiation therapy is additionally used. It is used for damage to lymph nodes and internal organs and allows you to destroy cancer cells.
Living with melanoma
Treatment of cancer, including melanoma, leaves a serious imprint on the patient’s life. Patients need to be prepared for various scenarios.
- Melanoma cannot always be cured. In some cases, it is impossible to completely get rid of a malignant tumor, then the main treatment tactic is to prevent its further spread in the body.
- Follow-up visits to the doctor and repeated examinations. Even after complete recovery from melanoma, regular visits to the oncologist every six months to a year are recommended. Along with the risk of recurrence, people who have had melanoma have a high risk of developing other types of cancer. Also, some treatment side effects may last a long time or may not even appear for several years after treatment ends.
- The need to store all medical records. Not only during treatment, but also after recovery. This can help cope with the delayed consequences of a particular treatment, as well as quickly select therapy in case of relapse.
Factors influencing survival
The 5-year and 10-year survival rates for different stages of melanoma are based on data obtained from patients who survived at least 5 or 10 years from the date of diagnosis.
The following factors influence survival:
- new developments in cancer treatment;
- the body's response to treatment;
- age of the patient (regardless of the stage of the disease, older patients live shorter than others).
Prognosis and prevention
The prognosis directly depends on the stage at which the tumor was detected. When skin melanoma less than 1 mm thick is removed, the survival rate is more than 90%, and only a small number of patients subsequently experience relapses [2]. At the same time, with large cancer tumors and metastases in internal organs, more than half of the patients die within a few years.
To prevent melanoma, it is recommended to follow the following recommendations:
- Avoid sunlight during the middle of the day. This is a risk of burns and sunburn, which causes skin damage and increases the risk of developing melanoma. Ultraviolet radiation is most intense from 10 a.m. to 4 p.m.
- Use sunscreen. Choose a product with SPF of at least 30 even on cloudy days, and in summer in the sun - SPF 40-50. Apply the cream generously to your body and repeat every two hours, or more often if you swim or sweat heavily.
- Don't forget about clothes. Cover your skin with dark, thick fabric that covers your arms and legs, and wear wide-brimmed hats. Wear sunglasses.
- Avoid tanning lamps and tanning beds, they emit ultraviolet rays and may increase the risk of skin cancer.
- Examine your body. Check your skin regularly to see if new formations have appeared, moles, freckles, or birthmarks have changed.
- Remove moles that are often injured. At the site of the removed mole, only a barely noticeable scar remains. The greatest risk of developing melanoma is in nevi that are regularly touched by underwear, backpack harnesses or a blade during shaving or haircuts.
Sunscreen as a means of preventing melanoma
Sunscreens help prevent skin cancer.
Photo: zefart / Depositphotos Before going outside on a hot sunny day, it is recommended to apply sunscreen to exposed areas of the body to block ultraviolet rays. However, not all products are suitable for children aged 6 months and younger. Sunscreen has varying degrees of sun protection. Sun protection factor, SPF, shows how well UV rays are blocked. To prevent melanoma, it is recommended to use products with SPF 30 or higher.
It is important to remember that sunscreen wears off or loses its protective properties over time. It should be reapplied if the skin remains exposed to the sun for more than 2 hours, after swimming, when sweating heavily, or after drying with a towel [4].
Conclusion
Melanoma is one of the most dangerous types of cancer. At the same time, due to the fact that it is usually located on the surface of the skin, it is easy to identify and remove in time. This will prevent the tumor from spreading to the internal organs.
The story of Christina from St. Petersburg, a patient at the Ichilov Cancer Center:
– While vacationing in Israel, I discovered a lump on the top of my foot. Then I didn’t even think that it could turn out to be cancerous. I decided that the bump looked unsightly and went to a dermatologist to have it removed. The doctor removed the lump and sent it for examination. It turned out that I had melanoma. I decided to play it safe and here, in Israel, I turned for advice to the Ichilov Oncology Center.
Before the diagnosis, of course, I knew that anyone can get cancer, but I didn’t worry about it. I went to the beach with my friends. I often neglected sunscreen because I wanted to have a beautiful tan. I like it when my skin feels like it's been kissed by the sun. I visited solariums and didn’t even think about the danger.
When I found out that I had melanoma, I decided: okay, it’s just a spot on the skin. It will be removed and everything will be fine. As it turns out, I am now in a high-risk group. Since I already had melanoma, the tumor may appear again.
I didn’t understand how serious it was until I talked to an oncodermatologist. Only then did I realize that this disease greatly affects the patient’s life. And I’m glad that I contacted the cancer center on time.