Epididymitis and orchitis are two diseases of the male genital area; they are extremely rarely diagnosed separately. Orchitis is an inflammation of the testicle, and epididymitis is an inflammation of its appendage. Since anatomically the testicle and epididymis are one area, inflammation easily spreads to neighboring tissues.
In the vast majority of cases, the cause of inflammation is infection: influenza, chicken pox, mumps, typhus. Sometimes provocateurs can be insufficient or excessive sexual activity, prolonged abstinence, and some other urological pathologies: urethritis, vesiculitis, prostatitis.
Statistics
Due to the anatomical features of the veins in the testicular area, varicocele most often forms on the left side. 80-95% are allocated to these cases. Right-sided testicular varicose veins are not so common (up to 8%). On both sides, varicocele occurs in 2-12 cases out of a hundred. Male disease is “linked” to the age of the patients. A large percentage (19) of problems with testicular veins are noted by doctors in adolescents. If we consider the reproductive age of men, then the statistics of varicose veins reach 35%. These are sad numbers, because... Varicocele in sexually mature men can cause infertility. Treatment of the disease should begin at the earliest stages.
How does a chronic process manifest itself?
If you ignore the symptoms of an acute condition, then orchitis and epididymitis can become chronic.
Chronic orchitis can only be indicated by pain in the testicle when touched or during active movements. Chronic epididymitis manifests itself with the following symptoms:
- constant increase in temperature to subfebrile values;
- soreness of the scrotum;
- discomfort and even pain in the area of the appendage of the testicle.
In the chronic course, there are no pronounced signs; the man feels a general malaise and periodic moderate pain in the scrotum area, which subsides and then worsens again.
What does it look like
A photo of a varicocele clearly demonstrates a male problem - the scrotum on one side (usually the left) is slightly lower. The skin covering the testicle does not hide the contours of the veins. When self-palpating the venous vessels, a man can feel their expansion. The patient may not even be aware of other symptoms of the disease. Palpation of the scrotum and visual examination are necessary actions for all men who care about their health. This is especially true for males planning fatherhood. You need to be regularly examined by a urologist. Medical examinations and consultations with qualified specialists are offered by the Global Clinic Center, which has extensive experience in the treatment of varicocele.
What does a testicular examination by a doctor look like?
No special early preparation is required for testicular examination. The examination itself is painless and completed quickly.
The doctor will ask you to remove your pants and underwear and feel (with gloves) both testicles to compare them. Some doctors examine patients standing, but most recommend lying down on a bed in the waiting room to relax.
The examination takes less than 5 minutes and may cause some inconvenience. But the best thing you can do for your health is to recognize as early as possible that something is wrong.
History of the disease
Varicocele is a disease with deep historical roots. The first mention of the problem dates back to the 16th century and is associated with the name of Paré, a famous surgeon of the Renaissance. He drew attention to the pathology of the venous vessels near the male testicle. Many medical historians speak of the involvement of Hippocrates and Celsius in establishing the facts about this problem. The topic of varicocele is very closely related to infertility. In the 19th and 20th centuries, scientists confirmed the possibility of curing male infertility in direct proportion to the elimination of testicular varicose veins.
Varicocele. Symptoms
The danger of the first stages of the disease is that it is asymptomatic. The problem is discovered by chance, during medical examinations or when patients address other male issues (for example, in connection with infertility). Symptoms of varicocele characteristic of other degrees of the disease:
- nagging pain and discomfort in the left side of the scrotum, testicle and groin area;
- drooping left (mostly) testicle, interfering with walking;
- decrease in the size of the testicle on the left;
- manifestation of the contours of venous vessels;
- appearance of pain.
Varicocele is characterized by symptoms manifested in a decrease in the number of sperm and a decrease in their motility, in this case it is worth talking about male infertility. When doctors try to find out the cause of male infertility and analyze various symptoms in a patient, they often discover a varicocele, using the most modern diagnostic methods.
Symptoms of acute orchitis and epididymitis
If the testicle and its appendage become inflamed for the first time, we are talking about an acute process. The symptoms of acute orchitis and epididymitis are similar. A man may experience:
- general malaise - weakness, loss of appetite, decreased ability to work;
- headache;
- increased body temperature, sometimes to very high values;
- pain in the perineum and scrotum, which can radiate to the tailbone, groin and lower back;
- redness and swelling on the side of the affected testicle.
It is the typical symptoms of scrotal diseases, that is, changes in size, redness and pain in the organ, that can become an indicator of orchitis and epididymitis. The remaining symptoms are not specific and may indicate other diseases.
Causes and risk factors for the disease
In the veins surrounding the spermatic cord, a malfunction of the valve occurs, which prevents blood from flowing back. Instead of rising upward, the blood stagnates, because... is transmitted in the opposite direction. Because of this, the venous vessels become dilated and weak. The causes and risk factors of varicocele are associated with the appearance of primary and secondary reflux. The abnormal structure of the veins associated with congenital pathology leads to the complete absence of valves for the reverse outflow of blood or their atypical operation. During puberty, blood pressure on the vessels increases, and varicose changes occur in the veins near the spermatic cord. The weak walls of blood vessels inherited from birth by boys cannot cope with the flow of blood during physiological changes. As a rule, varicocele is inherited, so this should be taken into account in case of male infertility and comprehensive treatment of testicular varicose veins should be carried out. Secondary reflux occurs when the blood outflow valves stop functioning normally due to problems in the renal or vena cava. Varicose veins most often occur on the left side, because it is on the left that the venous vessels meet the renal vein. Narrowing of the lumen in the latter structure can cause varicocele. Unfavorable factors for testicular varicose veins:
- haemorrhoids;
- phlebeurysm.
The following are considered as a trigger for the appearance of varicocele:
- Hard physical labor.
- Extreme loads in sports or weight lifting.
- Lack of normal sex life.
- Professions that require long periods of standing.
- Chronic constipation.
The most common diseases affecting the testicles
The content of the article
Epididymitis
Epididymitis is an inflammation of the epididymis, a long tube located along the edge of the testicles. Its function is to store sperm until they mature. Epididymitis can be caused by a sexually transmitted disease, injury, or the result of a vasectomy.
Symptoms:
- mild irritation or severe pain in the testicles;
- edema;
- increase in body temperature.
Treated with antibiotics. Rest, ice to reduce swelling, and anti-inflammatory medications such as ibuprofen are recommended.
It is recommended to use condoms during sexual intercourse to prevent inflammation. If left untreated, sperm may be blocked from the testicles, leading to problems with decreased fertility.
Hydrocele (hydrocele)
This is an accumulation of fluid in the space between the testicles and scrotum. Dropsy can affect one or both testicles, causing swelling but no pain. It is usually not harmful and does not require treatment, but if you notice a lump in the scrotum, see your doctor to confirm the diagnosis.
It is more common in infants and young children, and in adult men as a result of injury.
Testicular torsion
Inside the scrotum, the testicles can rotate around their axis and pinch the spermatic cord. As a result, the blood supply to this testicle is disrupted. It most often occurs in young men between the ages of 12 and 18 as a result of injury or heavy physical activity.
Symptoms of testicular torsion:
- sudden and severe pain;
- enlargement of the affected testicle;
- sensory sensitivity;
- the appearance of swelling.
This is an emergency disease. It is treated surgically to preserve the function of the affected testicle. If it takes too long to see a doctor or if the blood supply is cut off for too long, the testicle will be permanently damaged and will need to be removed.
Testicular cancer
Testicular cancer is the appearance of abnormal cells in the testicle that divide and grow uncontrollably in one or both testicles in young men, usually between the ages of 15 and 35.
Typical symptoms include:
- the appearance of compaction;
- unevenness;
- enlargement of one testicle;
- feeling of isolation;
- a dull ache that may come and go.
The exact cause is unknown, but some risk factors are known:
- undescended testicles (cryptorchidism);
- presence of testicular cancer in the family.
It is rare and responds well to therapy with a high cure rate. The first line of treatment is surgical removal of the cancerous testicle through an incision in the scrotum. In some cases, local lymph node removal and radiation or chemotherapy are required.
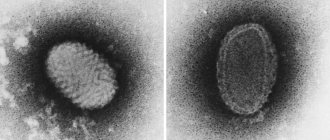
Orchitis or inflammation of the testicles
Testicular inflammation can affect one or both testicles. Mainly caused by bacterial or viral infection.
Causes:
- Mumps (mumps) is one of the most common causes of testicular inflammation, but fortunately it is being reduced today due to childhood vaccinations.
- Sexually transmitted diseases such as gonorrhea or chlamydia, which first cause epididymitis and then inflammation spreads to the testicles (epididymo-orchitis).
Symptoms:
- testicular pain;
- sensitivity;
- subsequent infertility if left untreated.
Treat with antibiotics if the cause is bacterial and rest is recommended.
Varicocele
Varicocele –
This is an enlargement of the veins in the scrotum. This is usually painless and harmless, but can still affect sperm production and quality. May sometimes cause mild pain and swelling. Although most cases of varicocele do not require treatment, some need to be treated with surgery.
Hypogonadism
A disease in which the testicles do not produce enough of the male sex hormone testosterone.
Types of hypogonadism:
- Primary – the problem is in the testicles themselves.
- Secondary is a problem with the pituitary gland in the brain, which normally sends signals to the testicles to stimulate production.
In adult men, hypogonadism has the following symptoms:
- erectile disfunction;
- infertility;
- decreased sex drive;
- decreased hair growth;
- reduction of testicles and their elasticity;
- decrease in muscle mass and increase in fat;
- breast enlargement;
- depression;
- fatigue;
- hot flashes.
First, they try to find a possible treatable cause, but if this is not possible, testosterone replacement therapy is prescribed.
If you notice any symptoms of the above conditions, you should immediately consult a doctor. The vast majority of these diseases are curable if detected in time.
Complications
The main thing that patients suffering from testicular varicose veins need to understand is the serious situation with the appearance of offspring. Infertility can become a sad complication of varicocele, so you should not delay going to the clinic for diagnosis and treatment. Doctors from the Global Clinic Center can provide qualified assistance. Statistics show that patients diagnosed with varicocele in 60 cases out of a hundred are faced with the problem of sperm dysfunction. 40% of men with testicular varicose veins become infertile.
Diagnostics
To effectively treat the disease, you need to use all diagnostic methods. To detect varicocele, experienced specialists only need to visually examine the patient and palpate the plexus of testicular venous vessels in the form of a cluster. The man is examined in a standing position, in a calm state. To clarify the results of palpation, the patient is asked to tense the abdominal muscles (Valsalva maneuver) to improve the filling of testicular vessels with blood. In this case, the study of the enlarged area will be more complete. This will help in diagnosing grade 2-3 varicocele; if the problem is not expressed, you will need the help of modern equipment. Ultrasound and doplegraphic examination of the scrotum is necessary to clarify the diagnosis. The patient must be examined in two positions - standing and sitting. To rule out infertility, a man needs to have a spermogram. One semen examination is not enough; examination in the interval from 4 to 12 weeks will make the diagnosis more accurate. This diagnosis is very informative; it can be used to determine the type of varicocele, obtain data on the size of the testicle, the location of diseased veins, and thickening of the spermatic cord.
Classification
The degrees of the disease are classified based on the dilation of the veins of the spermatic cord and testicle. The development of varicocele is divided into 4 degrees. They speak of zero degree if the symptoms of the disease cannot be determined visually or by manual palpation. Only instrumental examination (most often when diagnosing other problems) reveals varicocele. Grade 1 is diagnosed when the dilation of the veins cannot be palpated with the patient lying down, only standing. In patients with the 2nd degree of the disease, the doctor feels with his hands an increase in the venous vessels of the spermatic cord and testicle in men who are sitting and standing. To determine the third degree of varicocele, a visual examination of the patient is sufficient. If we consider testicular varicose veins from the point of view of the location of the pathology, then we distinguish left-, right- and bilateral varicoceles. Subclinical and clinical types of the disease are classified depending on physical examination methods.
Causes of testicular inflammation
The content of the article
Men over 45 who have a urinary tract infection or who have a catheter are at increased risk.
Known causes of orchitis:
- Bacteria - most often Escherichia coli, staphylococcus, streptococcus and Klebsiella pneumoniae. Prostate infection and epididymitis (inflammation of the testicles) may occur.
- Viruses - in almost 70% of cases, the cause is mumps - this is an infectious viral inflammation of the parotid glands that swell on one or both sides of the face.
- Sexually transmitted diseases: gonorrhea, chlamydia.
Treatment
The problem of varicose veins in the vessels of the spermatic cord and testicle cannot be eliminated. Improper operation of the blood outflow valves can be corrected through surgery. Surgical treatment of varicocele is the main method. The effectiveness of medication use is insignificant. Only the first stages of the disease can be treated conservatively. Consultation with a doctor and a joint decision on surgery for varicocele are mandatory. Surgical intervention is not always necessary for the patient. If the disease does not bother the man too much, or the patient is of advanced age, then doctors advise not to undergo surgery. A variety of surgical methods helps doctors find the only correct method. The essence of the operation for varicocele is to ligate the venous pathological vessels and normalize the outflow of blood. To save the results obtained during the operation, you should:
- limit physical and sexual stress;
- come to your doctor for examination.
Treatment of testicular inflammation
If these symptoms are noticeable, you should consult a urologist who will do a history, physical examination, urine culture, blood tests, and ultrasound.
If orchitis is bacterial in nature, treatment is carried out with antibiotics for 10 to 14 days.
On the other hand, if the cause is mumps (a virus), then analgesics and nonsteroidal pain relievers (ibuprofen, naproxen, or acetaminophen) are taken. The resulting inflammation will subside within 1 to 3 weeks.
If fever, nausea, and vomiting occur, the patient may be admitted to the hospital for intravenous antibiotics.