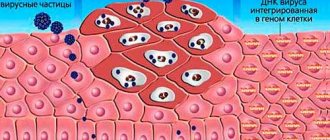
Papilloma is a formation that can appear on the skin or mucous membranes of a person and, without appropriate intervention, lead to serious consequences, including the development of cancer. Papillomas on the human body signal the presence of HPV (human papillomavirus) in the body. At the moment, a fairly large number of varieties of this virus have been identified. It has also been proven that about 70% of the sexually active population are its carriers.
Medical is a clinic that provides a wide range of medical services, including in the field of urology. The clinic’s specialists approach the treatment of each patient individually: this applies to both the timing of treatment and the treatment measures themselves, which most often allows for very effective results.
Causes of inflammation of papilloma on the neck
According to statistics, papillomatosis affects 80% of the population. The virus enters the body through hygiene items. Towels, razors, toothbrushes, and nail files must be individual.
External factors
External factors affect education:
- cut of growth when shaving;
- prolonged compression by clothing or accessories;
- hand scratch;
- negative effects of ultraviolet rays (solarium and sun rays);
- self-removal of formation at home. This applies to cauterizing substances, cutting, and ligation with threads.
Internal factors
If a papilloma on the neck becomes inflamed and red, it may be associated with a number of disorders within the body. Possible dysfunctions include:
- The presence of hormonal imbalances. Associated with pregnancy, abortion, miscarriage.
- Systematic emotional overstrain, stressful situations. With frequent nerves, the body's protective function is weakened. As a result, the immune system cannot resist viruses and infections.
- Exacerbation of chronic or congenital diseases.
- Re-entry of HPV into the body. The main sign is appearance.
The main cause of inflammation of formations on the neck is friction with clothing, long hair, and jewelry. Men often damage the growths when shaving, and women - when combing. Foreign agents easily enter the body through open wounds.
HPV in men: symptoms
Most often, HPV can be present in the human body for a long time without manifesting itself. However, the most important sign (symptom) of the possible presence of HPV in men and women is the appearance on the skin and mucous membranes, including in the groin or pubic area, of condylomas and papillomas - warts, lumps and irregularities of the skin, the color of which does not differ from the main one skin.
Condyloma is a genital type of papilloma, which looks like a small growth attached to the mucous membrane with a kind of “leg”. The size of condyloma can vary from a few millimeters to several centimeters - in the latter case we are talking about an accumulation of condylomas.
Such papillomas can appear on the head of the penis, on the foreskin, and also around the anus (then there is a high probability that condylomas may also be in the rectum). Most often they are painless, but in some cases men may experience additional symptoms of the human papillomavirus if the disease manifests itself as:
- pain when urinating, defecating, or having sex;
- bleeding of condylomas: sometimes ulcers that do not heal for a long time may form in their place;
- also sometimes condylomas can itch.
The listed symptoms usually indicate damage to the condyloma.
The appearance of papillomas, in addition to the presence of HPV in the human body, also indicates a depleted immune system and the possible presence of other sexually transmitted diseases. In addition, some types of papillomas, in particular condylomas on the head of the penis, have a high oncological potential, so when signs of the disease are first detected, you should consult a specialist. The sooner you start treating the human papillomavirus, the more chances a man has to avoid serious health consequences of condylomas. (All of the above applies to women as well.)
Initial appointment
An initial appointment with a specialist involves a thorough visual examination of the patient’s mucous membranes and skin, as well as questioning him and prescribing tests.
Although most often papillomas have a characteristic appearance, additional tests and diagnostics make it possible to absolutely accurately determine the presence of HPV in the patient’s body.
If HPV infection is suspected in men, the following tests are usually prescribed:
- blood test (for condylomas, also analysis of urethral discharge): modern diagnostic methods make it possible to isolate the DNA of the virus from the available material and thereby confirm its presence in the patient’s body;
- biopsy of papillomas (condylomas): done in order to determine the presence or absence of cancer cells in neoplasms.
Is inflammation of papilloma on the neck dangerous?
Inflammation of papilloma on the neck has a number of signs that you should know. If characteristic symptoms appear, you should consult a doctor. Important criteria of the pathological process:
- increase in size of the growth (shape changes);
- deformation of the top layer. Leads to the formation of cracks;
- change in the shade of the formation - may turn red or black;
- presence of severe itching and pain. Often a person complains of burning, bleeding;
- discharge of pus with an unpleasant odor;
- slight increase in the patient's body temperature.
Removal of genital papillomas
Where can you go in Moscow if a gynecologist has discovered papillomas on the genitals? Doctors at our clinic remove condylomas from women and teenage girls using the most modern, best method - radio waves. At your service are delicate gynecologists with extensive experience and positive reviews, good imported local anesthesia, which allows you to remove genital papillomas quickly and painlessly!
Prices for services
How much does it cost to remove papilloma on the genitals - the clinic’s basic range of services for women:
✘ Doctor’s appointment with examination - 2500 ₽; ✘ Consultation with a teenage doctor - 2500 ₽; ✘ High-risk HPV types - from 650 ₽; ✘ Colposcopy/vulvoscopy - 1500 0 ₽; ✘ Removal of genital papillomatosis - from 5000 ₽; ✘ Panavir dropper (with placement) - 5500 ₽; ✘ Allokin Alpha injection (with injection) - 3500 ₽; ✘ Taking a smear for viruses - 450 rubles.
Considering the widespread prevalence of genital papillomas and the various possible methods of their transmission, doctors recommend that both sexually active women, girls and adolescents undergo a medical examination and be examined for their presence (read more about condylomas in virgins).
Features of the treatment of inflamed papilloma
If the formation hurts, oozes blood on the neck, or is covered with a hard crust, then it cannot be ignored.
Need advice from an experienced doctor?
Get a doctor's consultation online. Ask your question right now.
Ask a free question
Treat the inflamed area with an antiseptic (Chlorhexidine, Septomirin). Apply in such a way as to prevent suppuration and dead skin. It needs to be covered with a band-aid to prevent additional infection from entering the body.
After protective measures, visit a dermatologist.
The specialist will conduct a comprehensive diagnosis of the patient’s body. After deciphering the tests, the doctor will select the optimal treatment option.
If healing occurs according to plan, then the person will get away with systematic treatment of the papilloma with an antiseptic.
If the inflammation has deepened, then the formation must be removed.
Antiseptic treatment
Antiseptic treatment is a conservative method. For the procedure to be high-quality and useful, you will need to follow the rules:
- The antiseptic must be colorless. Chlorhexidine, Miramistin or hydrogen peroxide are suitable for disinfecting a wound on the neck. After treatment, the problem area of the skin is sealed with a band-aid to prevent secondary infection from entering the body. Dermatologists prohibit the use of brilliant green or iodine.
- To eliminate bleeding, the papilloma is treated with hydrogen peroxide or a weakly concentrated solution of Miramistin. Education is bandaged. The cotton wool must be sterile to prevent additional infection.
- If the inflamed growth is very painful and burns, you cannot treat it with an antiseptic. Otherwise, you risk developing additional complications and disorders.
Sometimes, when treated with an antiseptic, part of the papilloma may fall off. A piece of growth must be placed in a sodium chloride solution to show the biomaterial to a dermatologist. The specialist will conduct a histological examination and determine the likelihood of developing oncology.
Lotion with ointment
Ointment or lotion cream is less aggressive than a solution. You will have to wait longer to achieve results. Effective options for neutralizing the inflammatory process in the neck:
- Oksolin. The substance has an antiviral spectrum of action and is easily absorbed by the body. The ointment is suitable for treating children. Lubricate every 8 hours until the condition improves;
- Fiferon. Cream lotions relieve redness. The medicine activates the immune system. Treat formations every 6 hours for 7 days;
- Panavir is a biologically active drug that has a static effect against papillomavirus. The cream is spread on cotton wool and applied to the problematic growth every 4.5 hours. The total duration of the procedure is 10 days;
- Zinc-salicylic mixture. The compound softens, dries tissues, and relieves inflammation. An increase in the size of rashes is excluded. Do not use lotions more than 2 times in 24 hours. The treatment period is a week. The effects will be visible in a few days.
Removal of papilloma
What to anoint
The treatment process for papillomatosis is based on the complex effects of immunostimulants and minimally invasive procedures. The appointment is made by a qualified doctor after a thorough examination of the patient’s body. The active components of the ointment can cause serious disorders and additional complications.
Homemade ointments
It is better to smear the inflamed papilloma with pharmacological agents prescribed by the doctor. Folk wisdom should not be ignored. Using the recipes of “grandmothers”, you can make high-quality consistencies for the treatment of formations. The total treatment period in this case is 14-20 days. In order for the therapeutic effect to be as beneficial as possible, it is necessary to observe the preparation proportions and lubricate daily.
Effective creams for inflammation are:
- garlic 5 cloves of the vegetable are crushed to a porridge state. The ingredient is mixed with Vaseline or cream until smooth. After cooling, the ointment is applied to the damaged area of skin. It is not recommended to visit baths and saunas;
- flour + vinegar (in equal parts) are stirred. Egg shells and pork fat are added. The resulting consistency should be like a paste;
- walnuts (4 fruits) + apple cider vinegar (100 ml). The ingredients are mixed together until smooth. Sometimes iodine is added. The product is placed on a sterile bandage. Leave the cream on the skin for 12 hours.
Pharmacy drugs
Pharmacological agents deeply freeze the formations, causing necrosis of papilloma tissue. As a result, after 5-7 days the growth disappears on its own. The most popular drugs are Cryopharm and Wartner Cryo. The active ingredient is dimethyl ether. Application to the inflammation is done using a special applicator.
Plant-based substances are no less in demand:
- celandine / super celandine. Fat cream contains alkali made of sodium and potassium. A burn sometimes leaves a small scar;
- Castor oil. The compound has natural castor beans. Before applying the liquid, it is necessary to steam the skin. After treatment, the area is sealed with adhesive tape. The procedure includes 10 sessions;
- Sleigh Skin. The drug includes tea tree extract, salicyl, castor oil, which reduce inflammation;
- Condilin. Podophyllotoxin is available in solution form. The substance is applied using a special applicator. The general course of treatment is 4 times. After treatment, the structure turns black over time and disappears (a common consequence);
- Feresol medicine contains tricresol and phenol. Among the side effects of the drug are burns. The cover may become swollen;
- Verrucacid. The liquid cauterizing agent is diluted with ethanol (1:20). To avoid damage to healthy tissue, zinc paste is used;
- Solcoderm includes nitric acid, causing damage to formations. For use only in hospital settings.
Observation
- After the disappearance of genital warts, women continue to undergo regular cytological examinations of smears from the cervix (possibly with virus typing) annually.
- If changes are detected in cytological smears from the cervix, patients should be observed once every 6-12 months, depending on the situation, until the process is completely resolved.
- Women with oncogenic types of HPV must undergo cytological and colposcopic examination (if indicated, consultation with appropriate specialists and additional examination).
How are papillomas removed?
Currently, there are a number of effective methods for removing skin tumors:
- using a laser - effectively, quickly and accurately, no scars remain.
- using liquid nitrogen - rapid freezing of tissues causes their necrosis and death, no defects remain, and recovery occurs quite quickly.
- using current - quickly and effectively, but in some cases, when removing large papillomas, small scars may remain.
- using a radio knife - the advantages of the method are rapid healing of the skin, absence of scars and pain during the procedure.
Details about methods for removing tumors
After removing the papillomas, the doctor gives recommendations on caring for the wound. When they are performed, healing occurs quickly and without complications.
Routes of infection
In most cases, the cause of infection is unprotected sexual intercourse.
The household method of infection with HPV is not relevant; in rare cases, risks are possible with a pronounced decrease in immunity and severe stress.
Dangers of infection
It may seem that papillomas are purely an aesthetic defect. However, it is not. Unfortunately, a number of HPV strains are a predisposing factor for the development of cervical cancer. These types of infections require careful attention from specialists, comprehensive treatment and observation.
Clinical picture
It is believed that the incubation period before the clinical manifestation of HPV-associated diseases can be 1-8 months. Condylomas are exophytic formations, sometimes resembling cauliflower, on the skin, perineal and perianal mucosa, as well as on the mucous membranes. They can be multiple, asymmetrical and polymorphic. It is possible to change the size and number of genital warts, often resulting in the disappearance of the rash. In women, HPV most often affects the cervix, vagina, vulva and perianal area.
The classification of HPV-associated diseases is presented as follows:
- changes in the squamous epithelium of low malignancy (anogenital condylomas of the cervix, mild dysplasia);
- changes in the squamous epithelium of a high degree of malignancy (moderate and severe dysplasia and cancer);
- invasive cancer.
Subjective symptoms of HPV infection of the genitals and anal canal are usually absent. Characterized by a rapid increase in the size and number of genital warts, especially during pregnancy. Occasionally, patient problems such as bleeding, discharge and itching in the affected areas are identified.
What are papillomas?
Vulgar warts
The most common variant is vulgar warts, which are located on the palms and soles.
Most often they appear at the site of skin trauma due to decreased immunity, excessive sweating and contact with chemicals.
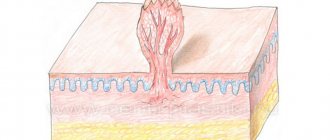
Externally, the wart has a round shape and a deep root, which provides nutrition and growth of the tumor.
Filiform papillomas
Formations that have a long stalk and are located on thin skin ( chest area, armpits, eyelids, etc.)
Most often they grow in length and appear in older people.
Flat warts
This form of neoplasm consists of small flat plaques that rise above the surface of the skin, located in the area of the labia, scrotum and labia.
Quite often, such papillomas are accompanied by itching, which in turn creates an increased risk of bacterial infection.
Thanks to the deep root, such a formation has good nutrition and quickly increases in size.
Condylomas acuminata
Formations located on the skin and mucous membranes of the groin area. quite often such papillomas are injured, which is accompanied by secondary infection and inflammation.
Outwardly, they look like a single growth, which grows over time and becomes shaped like a cauliflower or a rooster's comb.
Lewandowski-Lutz papillomas
A rare type of papillomas that are located on the feet, palms and face. Such formations have a variety of colors from light pink to brown and uneven edges. In some cases they may have a tendency to become malignant.
Plantar warts
Most often they occur in childhood and adolescence on the feet as a result of trauma to the skin on the soles, wearing tight shoes made of non-natural materials, excessive sweating and decreased immunity.
With this type of disease, small rough spots appear on the soles, growing not only outward, but also deeper. In addition to being an aesthetic defect, such warts cause discomfort and pain while walking.
Papillomatosis
A dangerous form of papillomas, manifested by the appearance of a large number of formations on the skin and mucous membranes.
Possible complications
Sometimes situations arise when the hanging papilloma is greatly inflated. This indicates pathological changes and activity of the virus in the patient’s body. The most common complications with the development of skin growths are:
- the appearance of bleeding that occurs as a result of surgery;
- infection of a damaged surface with a virus;
- development of benign tumors (hanging wart, papillomas);
- the formation of malignant structures with pus, blood, which can swell and dry out;
- diseases of the lungs, stomach and intestines (consultation with an oncologist);
- danger of sespis;
- suppuration of the inflamed areas, which may darken, swell or turn black.
Comprehensive diagnostics of the human body allows us to determine the degree of activity of the virus. The specialist identifies the level of oncogenicity and selects the optimal treatment tactics. The effectiveness of therapy depends on the quality of the systemic effect on the body.
The article has been reviewed by the site editors