Eye tumors are a group of cancer diseases that arise and develop in various tissues of the eye. Eye tumors can be benign, malignant, or locally destructive.
Among malignant neoplasms, eye cancer is less common than other oncological tumors; such neoplasms account for no more than 5% of all.
More than half of cancerous tumors of the organs of vision are tumors of the eyelids and conjunctiva. In second place are intraocular tumors and orbital tumors.
Treatment of eye tumors
There are two approaches to the treatment of eye tumors: surgical and organ-preserving. We give preference to the organ-preserving method, offering patients modern radiosurgical treatment of eye tumors using the CyberKnife system.
The Spizhenko Clinic was one of the first in the world to perform a unique operation using the CyberKnife system for uveal melanoma of the eye, as a result of which the patient was able to preserve not only the organ itself (before this, the only treatment option for this disease was removal of the eyeball), but also vision.
Radiosurgery using CyberKnife allows you to remove a tumor without a trace in one to three sessions, without damaging healthy tissue near the tumor, and does not require anesthesia, hospital treatment or a recovery period.
Expert commentary
Chebotareva T. I.
Head of the Department of Radiosurgery Tatyana Ilyinichna Chebotareva
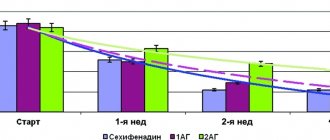
“Treatment of eye tumors using CyberKnife, which involves preserving the eye, is promising and effective. This is a painless, non-invasive treatment, in which it is possible to carry out treatment for both small and large prominences. We carry out a course of treatment in one session and achieve the death of cancer cells. According to our observations, the five-year survival rate after treatment is more than 95%, and the survival rate after all treatment methods without CyberKnife is from 56 to 90%.”
An analysis of 1099 histological reports and 350 case histories of patients with benign and malignant eye tumors operated on from 1990 to 2010 is provided. 4 main groups of the disease are identified: 1) eyelid tumors; 2) tumors of the conjunctiva, cornea and sclera; 3) intraocular tumors; 4) orbital tumors. It was noted that in the first two groups, malignant tumors were detected in approximately 10% of patients, in the group with orbital tumors - in 25.6% of patients and in the group with intraocular tumors - in 87.7%. The results of histological and clinical diagnoses in all study groups are analyzed.
Clinical histological analysis of tumors of the eye and its protective and auxiliary apparatus
We analyzed 1099 histological findings and 350 histories of the disease of patients with benign and malignant eye tumors, operated on in 1990 till 2010. Four main groups of the disease were singled out: 1) eyelid tumors; 2) conjunctival, corneal and scleral tumors; 3) intraocular tumors and 4) orbital tumors. It was noted that in the first two groups malignant tumors were revealed in approximately 10% of patients, in the group of patients with orbital tumors — in 25.6% of all cases, in the group of patients with intraocular tumors — in 87.7%. The results of histological and clinical diagnoses in all the groups were analyzed.
In the 60–70s of the twentieth century, an independent clinical direction was identified - ophthalmo-oncology, whose task was to develop and improve methods for diagnosing and treating tumors of the eye and surrounding tissues [1]. There are not so many publications on ophthalmo-oncology compared to other areas of ophthalmology, but most of them concern specific issues of diagnosis, treatment, and illustration of individual clinical observations. Perhaps, only a few works can be noted that cover the problems of ophthalmo-oncology more widely [2-5]. Without dealing specifically with this problem, we constantly had and have to observe patients with tumors and tumor-like diseases of the eye and its appendages, and operate on them, but there was no opportunity to analyze the results of our work, which is what this study is devoted to.
We conducted a retrospective analysis of 1099 histological reports of removed tissues and 350 medical records of patients with benign and malignant eye tumors treated in the branch over 21 years of work (from 1990 to 2010) (Table 1). During this time, about 250 thousand primary patients came to the branch.
Table 1.
Distribution of patients by tumor location (n%)
| Groups of patients by tumor location | Number of patients (abs.) | Number of patients (%) | Number of pathologies per 100,000 primary patients |
| 622 | 56,6 | 247 |
| 269 | 24,5 | 107 |
| 130 | 11,8 | 52 |
| 78 | 7,1 | 31 |
| Total | 1099 | 100 | 436 |
The largest group consisted of patients with eyelid tumors: 56.6%, or 247 per 100,000 primary patients. Among them, females predominated - 408 people. (65.6%), there were 214 men. (34.4%). Eyelid tumors were observed at any age with some predominance in groups over 40 years of age. In most cases these were benign tumors (557 people), malignant tumors were identified in 65 patients (9.8%).
Table 2.
Distribution of eyelid tumors in patients depending on gender and age
| Age | 1-9 | 10-19 | 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | 70 or more | Total |
| Husband. | 15 | 25 | 19 | 22 | 35 | 24 | 34 | 40 | 214 |
| Women | 19 | 34 | 42 | 57 | 56 | 68 | 60 | 72 | 408 |
| Total | 34 | 59 | 61 | 79 | 91 | 92 | 94 | 112 | 622 |
Among benign eyelid tumors, the most frequently identified histologically were so-called soft formations: papillomas (207), cysts (101), chalazions (73). Papillomas are tumors of the integumentary epithelium with varying degrees of dysplasia. They most often present as a slowly growing flat, round or oval formation with a loose, warty surface with a wide base or peduncle. Therefore, the clinical diagnosis of papilloma coincided with the histological diagnosis in more than 60% of cases. However, in the presence of varying degrees of dysplasia, keratopapilloma, fibropapilloma, seborrheic keratosis, hyperkeratosis and its most pronounced form, cutaneous horn, were histologically detected. In these cases, doctors diagnosed “neoplasm of the skin of the eyelid.” It is believed that the potential for malignant degeneration of keratoses is very small or equal to zero, but nevertheless, early removal of these formations is considered the most appropriate.
Cysts usually do not raise doubts among the doctor, and in half of the cases the clinical and histological diagnoses coincide. They are located, as a rule, on the anterior edge of the eyelid or at its outer and inner commissures, have the appearance of a rounded formation filled with either transparent contents (come from the sweat gland Moll), or oily contents (come from the modified sebaceous gland Zeis), or cheesy contents (come from the ordinary sebaceous gland). In the latter case, histologists call it an epidermal cyst or atheroma, and ophthalmologists often diagnose it as a neoplasm of the skin of the eyelid, lipoma, fibroma, dermoid cyst. Treatment of cysts is surgical.
Chalazion according to histological classification [6] refers to inflammatory tumor-like lesions. Chalazion (meibomian gland cyst) is a chronic aseptic lipogranulomatous inflammation caused by blockage of the gland outlets and stagnation of fatty secretion. Ophthalmologists know his clinic very well and the agreement between clinical and histological diagnoses is 88%, but in some cases doctors diagnosed a neoplasm (6 cases), papillomas, atheroma, retention cyst. In one patient with a clinical diagnosis of chalazion, histologists discovered basal cell carcinoma. This fact is well known in ophthalmological practice, therefore it is recommended to conduct a histological examination of the removed material, especially in case of relapses, which is not so rare.
Very rare eyelid tumors that we have observed are molluscum contagiosum, xanthelasma, fibroma, lipoma, syringoepithelioma, neurofibroma and a number of other lesions. I would like to say a few words about neurofibromatosis of the eyelids, which is a hereditary disease with a primary disorder in the development of nervous tissue cells. We observed three such patients and all of them had quite extensive testicular tumors of the eyelids, partially involving the adjacent tissues of the face and requiring their removal with simultaneous free skin grafting.
Among the vascular benign tumors, which occurred in both 21 adults and 6 children aged 6 months to 9 years, in most cases the histological diagnosis confirmed the clinical diagnosis (cavernous or capillary hemangioma). For small superficial formations, a fairly effective method of treatment at any age is the use of cryodestruction with a tip of the required area and with a temperature of about minus 1800; for large subcutaneous tumors, it is necessary to resort to surgical removal. Other tumors in children were histologically chalazion - in 6 cases, epidermal and dermoid cysts - in 10, papillomas - in 7, molluscum contagiosum - in 3, and in isolated cases fibroma, atheroma and inflammatory infiltration.
Malignant eyelid tumors were detected in 9.8% of patients in this group. Women also predominated here - 40 people (61.5%), there were 25 men (38.5%), mostly over the age of 40. The average age was 63.4 years, while in the group with benign eyelid tumors the average age of patients was 42.1 years. Clinically, a diagnosis of a malignant formation of the eyelid (basal cell carcinoma, cancer, carcinoma) was made in a third of patients, in the remaining cases - “neoplasm of the skin of the eyelid”, as well as “chalazion” in 1 case and “chondroma” in 1 case. Histological diagnosis in almost all patients in this group was "basal cell carcinoma". In principle, the clinical picture of this disease is quite recognizable and is characterized by the appearance of a dense, painless, slowly growing nodule along the edge of the eyelid (usually the lower one), sometimes with a slight ulceration in the center. It is at this stage that it is necessary to recognize and remove the tumor within healthy tissue; if this does not happen, the tumor grows and ulcerates, leading to significant defects and deformation of the eyelid. In these cases, radiation therapy with preliminary or subsequent reconstruction of the eyelid is already required. And although basal cell carcinoma is classified as locally destructive formations that do not lead to metastasis, in advanced cases the process can spread to orbital tissue. Therefore, only early detection and radical treatment of malignant eyelid tumors can preserve both the vision and the patient’s cosmetic appearance. There is another rather rare form of eyelid skin cancer, which pathologists interpret as solid cancer, and we published such a clinical case [7].
In group 2, we combined tumors of the conjunctiva, cornea and sclera, since they are interrelated with each other and, according to the modern clinical classification, are classified as diseases of the ocular surface. However, the predominant number of cases include purely conjunctival lesions (240 eyes), the remaining 29 relate to corneal and scleral lesions. As in group 1, women were more common here (60%), the distribution of tumors by age group was almost the same, and the average age of patients (44.7) ranged from 1 to 85 years. However, in contrast to group 1, where we counted about 20 different histological diagnoses, in the group with conjunctival tumors there were more than 40 of them.
Most often, papillomas (54 cases), granulomas (54), retention cysts (35), less often - formations such as pingueculae (8), capillary and cavernous hemangiomas (6), as well as single tumor formations such as proliferation of fibrous tissue, lymphocytic infiltration, the phenomenon of hyalinosis, amyloidosis, dystrophic changes with basophilic degeneration, keloid scar, a picture of hyperplastic tumor formation, a foreign body of the mucosa, an encapsulated parasite from the filaria group, Malouba epithelioma (benign necrotic tumor) and others. However, clinically, as a rule, the diagnosis was a conjunctival neoplasm. In 12 patients with a neoplasm of the lacrimal caruncle or lacrimal punctum, a retention cyst, papilloma, granulation tissue, sebaceous nevus, and hyperplasia of the sebaceous glands were histologically identified.
Malignant tumors of purely conjunctival localization that were surgically removed were rarely observed. These were melanomas (4 cases), undifferentiated sarcoma (1), suspected lymphoma (1). Most often, combined local lesions of the cornea and conjunctiva were observed, which were histologically interpreted as squamous cell carcinoma (15 eyes), melanoma (5). Those. in total, malignant lesions of the surface of the eyeball were detected in 26 patients, which amounted to 9.7%, as in the group with eyelid tumors.
It should be noted that it is almost impossible to clinically distinguish the benign or malignant nature of a tumor of the cornea and sclera, therefore, with the same clinical picture, in some cases, histological examination gives a diagnosis of squamous cell carcinoma, in others - an encapsulated formation such as osteoma, fragments of degenerative sclera with symptoms of hyalinosis, epidermoid , leukoplakia, chronic inflammation with deposition of calcium salts and others. In any case, these tumors are detected early, removed completely, covering the defect with a layer-by-layer corneal flap, and very rarely recur.
The group of patients with intraocular tumors accounted for, according to our data, 11.8% of the entire group examined, or 52 people per 100,000 primary patients. There were 78 (60%) women, 52 (40%) men. Their distribution by age groups is presented in Table 3.
Table 3.
Distribution of patients with intraocular tumors by age group (n)
| Age (years) | 1-9 | 10-19 | 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | 70-80 | Total |
| Husband. | 5 | — | 1 | — | 6 | 13 | 9 | 18 | 52 |
| Women | 2 | — | 1 | 1 | 10 | 16 | 24 | 24 | 78 |
| Total | 7 | — | 2 | 1 | 16 | 29 | 33 | 42 | 130 |
The largest group consisted of patients with tumors of the choroid - 109 people, with tumors of the iris - 12, with tumors of the ciliary body - 9 people.
Clinically, in most cases, iris tumors were represented by pigmented or weakly pigmented formations, slowly progressing, located in the peripheral parts of the iris and occupying no more than one sector. The indication for their removal was usually progression of tumor growth towards the anterior chamber angle. Histological examination revealed a diagnosis of melanoma in two patients, suspicion of melanoma in another two, and in other cases no evidence of a malignant process was identified. Cysts (4 cases), pigmented nevus (3) and verrucous papilloma were detected.
All tumors of the ciliary body were malignant in nature with a histological diagnosis of pigment epithelioid melanoma, which is considered the most malignant. In all cases with a clinically visible tumor node, the eyes were removed; in 3 cases with small tumors of the ciliary body, iridocyclectomy was performed.
In 109 patients in whom a detailed clinical examination revealed large space-occupying formations inside the eye, confirmed by ultrasound B-scanning, accompanied by a sharp decrease in vision, increased intraocular pressure, sometimes with pain symptoms, and suspected extraocular tumor growth, enucleation was performed. Histological examination of 101 patients confirmed the malignant nature of the tumor, with 40% diagnosed with spindle cell melanoma, which is considered more favorable in terms of prognosis for life than epithelioid type melanomas or mixed melanomas, which occurred in the remaining patients. In one case, a diagnosis of a malignant tumor of unknown origin was made; in 2 cases, tumor growth along the optic nerve into the orbital cavity was detected. Three children with retinoblastoma aged 1, 4 and 4 years, sent to Moscow oncology centers for consultation, had their eyes removed on their recommendation. All had a histological diagnosis of differentiated or undifferentiated retinoblastoma. Retinoblastoma is the result of transformation of retinal cells that occurs before their final differentiation. It can be hereditary and non-hereditary. In the first case, both eyes are usually affected; in the second, one eye is typically affected. These tumors easily undergo necrosis, so when they are detected in the initial stages, radiation therapy followed by chemotherapy is effective. If there is no effect of treatment for a large tumor, enucleation is performed.
In 8 adult patients, histological examination of the enucleated eye did not reveal a malignant process, and diagnoses were made: leiomyoma, schwannoma, cavernous hemangioma, capillary hemangioma with a focus of chronic inflammation, proliferation of granulation tissue, anthrocosis, keratotic hemangioma, and in one conclusion, “signs of a tumor process” No". In all these cases, the eye was removed according to clinical indications: lack of visual function, severe uveitis, secondary painful glaucoma, the presence of a tumor-like formation in the eye according to ultrasound and computed tomography. This discrepancy between clinical and histological diagnoses is well known, therefore, even with residual, low vision, you should always remember this and decide on the need for enucleation strictly individually.
Orbital tumors were detected in 78 patients, which was 7.1% of the entire study group, or 31 cases per 100,000 primary patients. As in all other groups, they were more often observed in women (70%), occurring at any age (Table 4), with an average of 48.9 years, ranging from 1 year to 84 years.
Table 4.
Distribution of patients with orbital tumors by age groups
| Age (years) | 1-9 | 10-19 | 20-29 | 30-39 | 40-49 | 50-59 | 60-69 | 70 and > | Total |
| Husband. | 1 | 4 | 1 | 4 | 2 | 7 | 7 | 3 | 29 |
| Women | 2 | 5 | 1 | 9 | 6 | 10 | 9 | 7 | 49 |
| Total | 3 | 9 | 2 | 13 | 8 | 17 | 16 | 10 | 78 |
Benign tumors were found in 58 people (74.4%), among them 36 women and 22 men, malignant tumors - in 20 patients (25.6%), including 11 men and 9 women.
The most common tumors observed were lacrimal gland tumors (12 cases). Clinically, the presence of a tumor-like dense formation located in the upper-outer part of the orbit and a downward and inward displacement of the eyeball are noted. The tumor grows slowly, sometimes accompanied by hyperemia of the eyelid. It is believed that the most common pleomorphic adenoma of the lacrimal gland is an epithelial tumor that arises from the ducts, stroma and muscular-epithelial elements of the gland. In our material, such a histological diagnosis was encountered only once; in other cases, the diagnosis was made of chronic dacryoadenitis (in 2 eyes), hyperplasia of the lacrimal gland, granulomatous inflammation, but most often the histological conclusion sounded like this: benign lymphoepithelial lesion, infiltration of small lymphocytes (lymphoma ), chronic inflammatory process with lymphoid infiltration, MALT lymphoma. We never encountered lacrimal gland cancer, but two patients were diagnosed with lymphocytic lymphosarcoma.
Another fairly common cause of exophthalmos are dermoid and epidermoid cysts - benign cavity formations from the group of teratomas (choristomes), formed when the ectoderm is displaced under the skin along the line of the embryonic junction. We observed 10 such patients, among them a 3-year-old girl. These formations are often located in the outer parts of the orbit, are often fused with the surrounding tissues and cannot always be removed in the capsule, so relapses are possible. Clinically, the diagnosis of a cyst is made in most cases using computed tomography or magnetic resonance imaging. Clinical and histological diagnoses almost always coincide.
The next fairly common finding during orbitotomy is vascular tumors - capillary and cavernous hemangiomas, which we observed in 11 patients. The first is most often located at the entrance to the orbit, the second - anywhere in the orbit within the muscular funnel. Hemangiomas located in the area of the orbital apex are very difficult to remove. Unfortunately, removal of such tumors can lead to vision loss due to their close connection to the optic nerve. Among other causes of a benign process in the orbit, histological studies indicate inflammation of the orbital tissue (pseudotumors), tumors arising from nervous tissue (neurofibromas, neurolemmomas, meningiomas, gliomas) and tumors of glial origin.
The clinical picture of a malignant tumor of the orbit manifests itself in the form of rapidly developing exophthalmos, although in some cases the picture is similar to the course of a benign process. Most often, histologically detected tumors associated with damage to lymphoid tissue (lymphoma, malignant lymphoma, lymphosarcoma, prelymphocytic sarcoma, lymphogranulomatosis), as well as embryonal rhabdomyosarcoma, pigmented melanoma, squamous cell carcinoma, sweat gland cancer and others.
In case of a malignant process associated with damage to lymphoid tissue, patients were sent for treatment to an oncology clinic, where radiation and chemotherapy were carried out. It should be noted that rhabdomyosarcoma is considered a tumor characteristic of childhood, but in our material this histological diagnosis was made to patients aged 41 and 69 years. Treatment was also carried out in the oncology clinic as for lymphomas. For pigmented melanomas and carcinomas in which neither radiation nor chemotherapy is effective, the only method is orbital exenteration.
Conclusion. The analysis showed that, despite the predominantly benign nature of tumors of the eyelids, conjunctiva and anterior surface of the eyeball, approximately 10% of those examined with this pathology were diagnosed with a malignant lesion, radical treatment of which is possible only in the initial stages. In advanced stages, treatment can result not only in large cosmetic defects, but also in loss of vision and death of the patient. Tumors of the choroid and ciliary body are distinguished by a high degree of malignancy. Unfortunately, early detection of these tumors is not carried out properly. Over the entire period of our work, you can count on your fingers the number of patients whom we sent to Moscow ophthalmic-oncology centers for radical treatment.
In orbital pathology, a malignant process occurred in 25.6% of all cases, but even with benign tumors, untimely treatment can lead to loss of visual function.
V.A. Machekhin
Tambov branch of the MNTK "Eye Microsurgery" named after. acad. S.N. Fedorov" of the Ministry of Health of the Russian Federation
Machekhin Vladimir Aleksandrovich - Doctor of Medical Sciences, Professor, Chief Scientific Consultant
Literature:
1. Brovkina A.F. Diseases of the orbit // Eye diseases: textbook / ed. V.G. Kopaeva. - M.: Medicine, 2002. - P. 411-449.
2. Brovkina A.F. New formation of the orbit // M.: Medicine, 1974. - 256 p.
3. Brovkina A.F. Orbital diseases. - M., 2008. - 251 p.
4. Voino-Yasenetsky V.V., Panfilova G.V., Terentyeva L.S. and others // Tumors of the eye, its appendages and orbit / ed. ON THE. Puchkovskaya. - Kyiv, 1978. - 230 p.
5. Vazhenin A.V., Panova I.E. Selected issues of onco-ophthalmology. - M.: publishing house of the Russian Academy of Medical Sciences. - 2006. - 154 p.
6. Zimmerman L.E., Sobin L.G. Histological classification of tumors of the eye and its appendages. - Geneva, 1984. - 80 p.
7. Machekhin V.A. An atypical case of a tumor of the upper eyelid // Ophthalmosurgery. - 2011. - No. 3. - P. 68-71.
What is radiosurgical treatment for eye cancer?
Radiosurgical treatment using the CyberKnife system consists of two stages: preparation for treatment and the radiosurgery itself. Based on CT and MRI diagnostic images, computer planning is created for the delivery of multiple microbeams of radiation into the tumor, taking into account the location of healthy tissues and critical structures (optic nerve, salivary glands, brain, etc.).
Choroidal melanoma. Radiosurgical treatment plan using the CyberKnife system
The treatment is carried out in just one fraction (session), after which the patient leaves the clinic independently. During radiosurgery, the patient sits comfortably on the CyberKnife treatment table while a compact linear accelerator moves around him, delivering high doses of ionizing radiation precisely into the eye tumor volume.
A single ablative dose on CyberKnife of 22-27 Gy and hypofractionated irradiation of 3-5 fr. (30 Gy) causes destruction of tumor tissue.
| Positioning the patient before treatment on the CyberKnife | Control of the treatment process on CyberKnife |
Symptoms of pathology
In the early stages of development of retinal cysts, cystic degeneration develops in its peripheral zone. The transparency of the retina decreases with the appearance of a grayish tint. As the process of degenerative cystoid changes intensifies, retinal tissue separation occurs. With the progression of the detachment process, the area and height of the existing cellular changes increases. As a rule, such changes occur in the lower outer quadrant of the fundus, then spreading to the entire periphery (the changes are circular in nature). Less commonly, the lesion begins in the outer quadrant, gradually moving into the macular zone.
The progression of retinal detachment in height also occurs gradually. At the initial stage, the changes are almost flat, with the affected area colored gray and the course of the vessels unchanged. Then the height of tissue splitting increases with the movement of vessels into the affected area. This becomes the impetus for the development of secondary dystrophic processes: disorganization of pigment deposition in the layers of the retina and focal atrophy of the pigment epithelium occurs. In some cases, at this stage, tears occur in the outer or inner layers of the retina. At the same time, tears in the outer layer are usually larger and irregular in shape. When internal layers rupture, the size of the defects is usually smaller and its shape is correct. The bullous stage of cystoid degeneration is characterized by significant changes in the retina. It begins to resemble a prominent transparent formation with clear contours. If there are ruptures at this stage, in most cases retinal detachment occurs.
Diagnosis of eye cancer tumors
A preliminary diagnosis of eye cancer can be made after an ophthalmoscopy.
Computed tomography is performed on a high-precision 32-slice spiral tomograph Siemens SOMATOM go.Up
To confirm an oncological tumor, the patient will need to undergo a series of procedures that will give an idea of the nature of the tumor. Patients undergo ultrasound of the eyeball, CT, MRI and fluorescein angiography. Also, if necessary, a biopsy of the tumor is prescribed for histological examination of the tissue. All diagnostic methods and laboratory tests are available.
Diabetic retinopathy
Eye changes in diabetes mellitus cause disruption of oxygen delivery to the retina and lead to the development of diabetic retinopathy. The disease does not develop immediately, but 5–10 years after the onset of diabetes.
Depending on the form of the disease (diabetes type 1 or 2), retinal lesions will differ. A patient with type 2 diabetes often exhibits signs of diabetic maculopathy, leading to decreased visual acuity. In the insulin-dependent form of diabetes, changes in the retina are much more pronounced and are manifested by proliferative changes: the growth of new defective vessels (retinal neovascularization), hemorrhages and scarring of the retina, macular edema.
To treat diabetic retinopathy, laser coagulation of the retina, intravitreal injections of anti-VEGF drugs, and in severe cases, surgical treatment (vitrectomy surgery) are used.
Read more about the treatment of diabetic retinopathy >>>
Symptoms of eye cancer
Eye tumors have a number of symptoms that are regarded as potentially developing into cancer. This:
- vision decreases
- spots appear on the iris of the eye
- blurred visions, spots, light flashes appear in the eye
- the eyeball is clearly moving
- squint appears
- Severe pain appears in the eye or area around it
- growths and thickenings form on the eyelid
- with tumors of the conjunctiva, pronounced nodules appear; a dense whitish film with a bright vascular pattern is also possible
- if a tumor appears in the lacrimal gland, then pain and profuse lacrimation begin
- With retinoblastoma, photophobia and possibly severe strabismus are manifested.
The appearance of each of the above symptoms is a reason to contact a specialist, preferably an oncologist.
Major retinal diseases
- Retinal angiopathy;
- retinal detachment;
- retinal dystrophy;
- diabetic retinopathy;
- retinal tear;
- retinal degeneration;
- macular degeneration and macular degeneration;
- retinitis;
- hypertensive retinopathy;
- retinal tumor;
- retinal hemorrhage.
Retinal pathologies can occur with various general and systemic diseases - hypertension, diabetes mellitus, kidney and adrenal gland diseases, as well as with eye injuries and traumatic brain injuries. Some infectious diseases (flu, etc.) can be complicated by retinal diseases.
Causes of eye cancer
Scientists are not yet able to establish the exact causes of oncological tumors of the organs of vision. Research results indicate the existence of a number of factors that provoke cancer.
Metastases of other oncological tumors also often provoke vision cancer.
Common factors for the development of eye cancer:
- one of the important factors is heredity;
- The disease can manifest itself in those who live in poor environmental conditions or work in hazardous industries.
- Ultraviolet rays are dangerous to the eyes.
- Among the common causes of eye cancer are nevi (pigment spots) on the iris of the eye.
- The cause of eye cancer may be HIV infection.
Age-related macular degeneration (AMD)
The disease is most often detected in people over 50 years of age and is the main cause of irreversible vision loss. The risk of the disease increases with a genetic predisposition, as well as in patients with diabetes mellitus, hypertension, and atherosclerosis. Symptoms of the disease are associated with damage to the macula area of the retina.
The initial manifestations of AMD do not have any clinical manifestations and can only be detected during an examination by an ophthalmologist. As the disease progresses, symptoms such as distorted outlines of objects, blurred vision, and blurred vision appear.
The dry form of AMD does not require special treatment. To treat the wet form of age-related macular degeneration, intravitreal injections (injections into the vitreous cavity) of drugs that block the growth of defective vessels under the retina (anti-VEGF drugs) are used. In addition, photodynamic therapy and laser photocoagulation of the retina are indicated.
Read more about AMD treatment >>>