Patients who become infected with Demodex mites may experience unpleasant symptoms. Sometimes this disease leads to serious complications.
When a mite penetrates the eye area, it leads to increased tearing, eyelash loss, and inflammation. This parasite multiplies in the sebaceous and meibomian glands, as well as in the hair follicles of the patient. Often a tick infection is asymptomatic, that is, it does not cause any discomfort to the host. However, the activity of the tick can increase when the functioning of human internal organs is disrupted, including the immune, nervous and endocrine systems.
The size of the Demodex mite varies from 0.16 to 0.48 mm. About 25 individuals can live in one hair follicle. In a quarter of cases of tick detection on the skin of the face, damage to the sebaceous glands and meimobian ducts occurs. A number of ophthalmological problems are also caused by infection with this parasite. Thus, it is one of the leading causes of blepharitis, chalazion, blepharoconjunctivitis, episcleritis, and keratitis.
What causes demodicosis on the face
The causative agent of demodicosis is the demodex mite (Demodex folliculorum). It is also called the iron woman. This is a permanent ectoparasite of humans, that is, the tick lives in almost all people, regardless of age, gender, or attitude to hygiene. Demodex on the face parasitizes the sebaceous glands, as well as hair follicles. It is considered a physiological part of the normal human microflora of the skin. This is an opportunistic parasite, since in its presence the skin can look and be healthy. The main thing is the number of ticks. While it is relatively small, the disease does not manifest itself in any way. When there are a lot of them, it becomes noticeable on the skin, and the person gets uncomfortable sensations on the skin of the face.
Ticks begin to actively reproduce for one reason or another. The female lays eggs, the parasites develop within 15 days, after which they also continue to increase the population.
An increase in tick activity is usually caused by some reason. These could be nutritional errors, diseases of the gastrointestinal tract, nervous system - anything that upsets the balance of the skin condition.
Also, the causes of demodicosis on the skin of the face can be:
- excessive passion for decorative cosmetics;
- long-term use of hormonal ointments;
- very frequent visits to the sauna or bathhouse, solarium;
- poor hygiene, infrequent change of towels and bed linen.
Causes
Demodex is activated when the immune system is weakened, the main reasons for this are:
- Long-term course of infectious pathologies.
- Taking certain medications.
- Hormonal imbalances.
- Prolonged exposure to stress.
When a person’s immunity is strong enough, mites do not reproduce, and they produce in accordance with the balance of positive flora. In addition to a decrease in protective functions, the following can provoke the appearance of pathology:
- Violation of hygiene rules.
- Age-related teenage hormonal changes in the body, when sebaceous secretions are actively secreted, become viscous and clog pores.
- Hormonal ointments.
- Failures of metabolic processes.
- Disturbances in the digestive system.
- Poor quality cosmetics.
How the disease develops
Demodectic mange on the face can develop in several stages. Characteristic symptoms appear as follows:
- The skin on the face turns red. At the same time, the person feels irritation on the skin and heat. At first, the redness is temporary, intensifying in bright sun, after exercise, or drinking hot drinks.
- The redness becomes persistent and permanent. The face is red, especially on the cheeks, chin, nose, and in some cases on the forehead.
- Blood vessels dilate , spider veins appear on the face.
- Papules and pustules develop. These are painful ulcers, acne. They are painful, do not last long, and scars form in their place.
- Rhinophymas appear on the nose - these are compactions, small tumors on the skin. The blood vessels and sebaceous glands become inflamed, the nose enlarges and becomes shapeless. More often, this symptom is characteristic of men with demodicosis on the face.
All this is accompanied by increased sebum secretion or dryness. The skin becomes rough. The person feels burning and itching. There is a tingling sensation on the face and the skin hurts. The face becomes noticeably swollen and swollen due to impaired lymphatic drainage.
Demodicosis of the face is often, but not always, accompanied by demodicosis of the eyelids. Symptoms of eyelid damage include redness, irritation, dryness, and a feeling of a foreign object in the eyes. The eyelids become inflamed and blepharitis appears. Eyelashes stick together and fall out. The eyes are constantly inflamed and tired.
Advantages and disadvantages
Although mechanical cleaning is currently considered the most common cosmetic procedure, it has both its supporters and opponents. The latter, arguing their negative attitude towards mechanical cleaning, give the following arguments:
- This procedure is quite painful, which cannot be said about manual cleaning.
- It may leave scars and spots. That is why mechanical cleansing is most often carried out in combination with a special anti-inflammatory drug, which helps to effectively fight age spots, evens out skin color and improves the regulation of sebum secretion.
- Mechanical cleansing is contraindicated in cases where the patient has inflammation and comedones on the face. If for some reason the cosmetologist does not take these factors into account and carries out cleaning, there is a risk of developing irritation and spreading the rash.
The advantages of mechanical cleaning include high efficiency. No other drug and no other procedure will give the same results as it does.
How is demodicosis diagnosed?
Demodectic mange on the face is often confused with rosacea and acne. In fact, tick infestation is very often combined with these diseases. When a person has both demodicosis and acne, the rashes are asymmetrical, there are more of them on the cheeks and closer to the temples. Demodectic mange worsens rosacea; due to mites, redness, itching and peeling become stronger.
To understand exactly what causes redness and discomfort, a diagnosis is necessary. If mites are found in the rashes, we can talk about demodicosis, and their number should be more than 5 individuals per square centimeter of facial skin. If there are fewer of them and there are no clinical symptoms, then in this case the person is considered not sick, but a carrier of the tick. It does not require treatment. To detect mites, the skin flakes and the contents of the sebaceous ducts are examined.
Is it contagious and can it be passed on to other people?
Demodicosis is a contagious disease, easily spread by contact. However, this is not a reason to panic. In fact, 97% of healthy people (this is medical statistics) are carriers of Demodex folliculorum, but in order for the mite to go on the offensive, it needs favorable conditions, which were discussed at the beginning of the article.
There are especially many carriers of the disease among older people - every two out of three people are infected with ticks. In a child, the potential danger is lower - one person out of three is infected. For middle-aged people, this statistic is 50/50.
Information for owners of cats and dogs: our pets can also suffer from demodicosis, but these forms of the disease are absolutely safe for people.
How to treat demodicosis on the face
To confirm the diagnosis and obtain an effective treatment regimen, you need to consult a dermatologist. All drugs used in the course of treatment must do the following:
- destroy parasites;
- disinfect the skin;
- remove inflammation;
- reduce lard production.
There are various ways to combat demodicosis. Treatment can take up to a year, but usually the treatment time is 2 – 3 months. It consists in applying antiparasitic and anti-inflammatory ointments, creams, and gels to the affected areas of the skin. The most common remedy is sulfur ointment. It kills adult ticks and eggs, disinfects the skin, and promotes its restoration. A wide range of acaricidal drugs are also used. Depending on the degree of damage, they are applied several times a day, and treatment takes from a couple of weeks to several months.
In some cases, topical medications are supplemented with immunostimulating agents to enhance the body's immune response and speed up recovery. If an infection is added to the skin lesions from mites, treatment with antibiotics may be required. This should only be prescribed by a doctor. Itching, burning and tingling are relieved with antihistamines.
In addition to treating the skin, it is important to identify and eliminate the causes that caused demodicosis in humans. If there are problems with the gastrointestinal tract, diet, proper nutrition, and the exclusion of fatty, salty, and sweet foods help. It is also necessary to provide a sufficient amount of water, vitamins, and minerals. Eliminate stressful situations and other circumstances that could cause an exacerbation of demodicosis.
3.Diagnosis of the disease
After a visual examination and conversation with the patient, the dermatologist prescribes a microscopic examination
.
Material for analysis is taken by scraping the epidermis from the affected areas of the skin. It is also recommended to analyze eyelashes
taken from different parts of the eyes. Express analysis makes it possible to get instant results. During the study, adult ticks, their eggs and shed chitinous shells are discovered. In order for the dermatologist to see a complete picture of the density of mite colonization of the skin, it is recommended not to wash your face for 24 hours before the examination. What is important for making a diagnosis in this case is not the fact of detecting a tick in itself, but the number and activity of the parasite, as evidenced by the number of larvae and eggs.
About our clinic Chistye Prudy metro station Medintercom page!
Facial care
For treatment to be effective and quick, it is necessary to properly care for your facial skin. It is better to use specialized lines of products, for example, STOPdemodex or Demolan Forte. They help cleanse the skin of excess sebum and remove traces of mite activity. The active ingredients penetrate into the deep layers of the skin and heal it. Series of products include scrubs, masks, soaps, lotions, creams. It is enough to apply them 1 - 2 times a day or periodically, as the manufacturer recommends, but this should be done regularly.
Specialized products improve skin condition, normalize fat metabolism, and remove dryness and discomfort. During treatment, you should avoid decorative cosmetics, and when using them, thoroughly cleanse your skin. Also, you should not visit the bathhouse, sauna, sunbathe on the beach or in the solarium. All this will increase the effect of treatment and help avoid re-infection.
In addition to using special anti-demodicosis products during treatment, you need to thoroughly wash all brushes, sponges and other tools used to apply cosmetics to the face. It is better to replace them with new ones and always keep them clean. You also need to monitor the cleanliness of towels and bed linen, change pillowcases more often, and be sure to iron them after washing. Towels can be temporarily replaced with disposable paper towels.
If demodicosis on the face is not treated, it will become chronic and the deep layers of the skin will be affected. Folliculitis will be added to the external manifestations, and painful ulcers will appear. This will significantly reduce the quality of life. It is better to prevent such development by consulting a doctor in time and choosing special products for daily skin care.
Prevention
There is no clearly developed scheme for the prevention of demodicosis and demodex with medications, since the mites that cause it are permanent inhabitants of the human body.
But there are certain recommendations that, if followed, will help you avoid getting sick when in contact with sick people and protect yourself from self-infection:
- At the slightest change in the skin, you should consult a doctor, even if you think it is a simple allergic reaction to food.
- Constantly take vitamins and other medications that increase the body’s immune defense against ticks.
- Clean animal fur with special means, as they are carriers of tick larvae.
- During treatment with medication, you need to change linen and towels daily.
- Do not use the patient’s underwear and bath accessories.
- If you wear glasses, treat them regularly with disinfectants.
- Wash with special products not only for the patient, but also for everyone who communicates with him.
- If one of the family members is sick, then everyone in contact needs to be checked by a doctor and have scrapings taken to determine the number of mites.
- During treatment, do not overstrain your eyes.
- Try to avoid stressful situations.
Life cycle
The entire life course of a worm-like mite can be divided into two periods of existence:
- intradermal (maturation and reproduction)
- extracutaneous or cutaneous
The mite, fixed on the walls of the excretory ducts, reaches a sexually mature state, is fertilized, and lays eggs. This concludes the ripening period.
Then a cutaneous, metamorphic period takes place outside. The eggs reach the surface of the dermis with a current of sebum. The larvae that emerge from them settle under the scales of the epidermis, in the mouths of the hair follicles. Molting (metamorphosis) takes place there - protonymph and teleonymph.
Subsequently, adults roll down the excretory duct of the sebaceous glands, and the cycle begins again. Fertilization is internal; individuals mate at the mouth of the follicle. In total, the life cycle takes 15-25 days.
It is possible to defeat parasites!
Antiparasitic Complex® - Reliable and safe removal of parasites in 21 days!
- The composition includes only natural ingredients;
- Does not cause side effects;
- Absolutely safe;
- Protects the liver, heart, lungs, stomach, skin from parasites;
- Removes waste products of parasites from the body.
- Effectively destroys most types of helminths in 21 days.
There is now a preferential program for free packaging. Read expert opinion.
Read further:
Main types of streptococci: description and life cycle of development
Demodex brevis: structure of the parasite, diagnosis and how to treat
Life cycle of development of the human roundworm, stages of development of the parasite in the body
Tumbu fly (photo): description of the parasite, life cycle of larval development
Dermatobia Hominis: description, development cycle, symptoms and treatment
Taenia saginata: description of the parasite, life cycle of development, routes of infection and treatment
O.V. Kalinina, K.N. Pustovaya, V.I. Nozdrin
JSC "Retinoids", Moscow
Summary
The literature review examines the main aspects of the available information about Demodex mites in humans. The article presents data on the classification, prevalence, structure, types, life cycle, methods of their detection and diseases associated with them.
Keywords:
Demodex mites, rosacea, morbidity, diagnosis.
General information about Demodex mites
Demodex mites are small parasites belonging, according to taxonomic classification, to the phylum Arthropoda, class Arachnida, order Acariformes, family Demodicidae, genus Demodex. More than 140 species of ticks have been described, found both in humans and in various mammals (rodents, domestic animals, small and cattle). Currently, the morphology of most Demodex mites has been well studied, and the generalized damage they cause for animals is a potentially dangerous condition, if untreated, fatal, which is associated with intensive proliferation of mites and the addition of a secondary infection [2, 3]. Despite the fact that ticks are highly species-specific, there are reports in the literature of cross-infection with these ticks between humans and animals [4, 5]. Some authors are studying the issue of the relationship between mites and the host organism, although the issue of Demodex residence continues to remain unclear [6, 7]. In the specialized literature, there is a description of an increasing number of epidemiological and clinical studies that indicate the important role of Demodex mites in rosacea and pityriasis [8, 9], as well as seborrheic and perioral dermatitis, blepharitis, alopecia and other lesions of the skin and its appendages [10, 11, 12]. There are observations of an increase in the number of mites in rosacea under long-term use of glucocorticosteroids [15, 16]. It is assumed that the development of neoplasms of the skin and its appendages promotes the production of protease and cytokines, which leads to a decrease in immunoreactivity. This in turn causes an increase in the number and parasitic activity of Demodex mites [17, 18]. Thus, the presence of Demodex mites in the skin contributes to the development of skin diseases, which becomes a public health problem [19].
Demodex mites have been a topical subject for study by parasitologists, veterinarians and dermatologists for more than 180 years. They were first identified in human earwax by F. Berger in 1841 [22]. In the same year, J. Henle described mites in human skin, and G. Simon established the presence of mites in hair follicles and characterized its morphological properties, giving it the name Acarus folliculorum [11]. A little later, G. Simon (1842) and R. Owen (1843) attributed the discovered mites to the genus Demodex [22]. Half a century later, the English acarologist S. Hirst named 21 species and several subspecies of these mites in animals [20]. Subsequently, studying them in human skin, L.Kh. Akbulatova (1963) identified two forms of mites: Demodex folliculorum longus and Demodex folliculorum brevis, which differ in the structure of adults and the development cycle [21]. After this, CE Desch and WB Nutting (1972) divided Demodex mites into 2 species observed in humans according to modern scientific concepts [22].
Adult Demodex mites are divided into the head, thorax and abdomen. The entire body of the tick is covered with a translucent chitinous shell and consists of two fused segments. Four pairs of short, segmented legs are attached to the chest and end in claws. They ensure tick movement at a speed of 8–16 mm/h, mainly at night. The tick has a round mouth opening and piercing chelicerae. The digestive system of Demodex mites is greatly reduced and consists of chelicerae and a poorly developed lumen of the middle pouch, without the hindgut and anus [1, 23].
Demodex folliculorum and Demodex brevis differ in structure. Thus, the Demodex folliculorum mite has an elongated, worm-shaped body, a well-differentiated head end, and a transversely striated posterior section about 0.3–0.4 mm long. Demodex brevis is characterized by a length of about 0.15–0.2 mm, a flattened head section, a wide abdomen without setae, a cone-shaped posterior end, and short legs. The cuticle covering the abdomen is less transparent. Males are always smaller than females and die after fertilization [1, 19].
In most patients, Demodex folliculorum is more often detected, but both types of mites can be detected at the same time. Demodex folliculorum is usually found on the face and is localized in the upper part of the pilosebaceous follicle, where individuals gather in groups. Such mites are also found in the cheeks, nose, chin, forehead, temples, eyelashes, eyebrows, external auditory canals, neck and other seborrheic areas, such as the upper and medial areas of the chest and back. The head end of Demodex mites is directed towards the bottom of the follicle, where it feeds on skin cells and sebum. Demodex brevis is most often found in the eyelid area, neck and chest. The mite occupies one follicle and is found more often in the deep sections of the sebaceous glands and their ducts, as well as in the meibomian glands, so it is more difficult to detect [13, 24].
Demodex mites contain the enzyme lipase, which promotes the formation of free fatty acids from triglycerides in sebum. It has been suggested that mites may normally play a role in protecting human skin from bacteria, particularly Staphylococcus aureus and Streptococcus [25], but this issue is controversial: in the case of dermatitis associated with Demodex mites, the latter may be involved in increasing the number of microorganisms and cause an inflammatory process.
A comparative study of tick nucleotides revealed their sequence similarity, which was more than 67%, and the homology of the A/C nucleotide sequence was 99.7% [26]. Genetic differences in the mitochondrial CO1 gene have been established in populations of mites living on human eyelashes and skin. Four mite phenotypes have been identified; the similarity of Demodex folliculorum is closer to Demodex canis than to Demodex brevis. [27].
Demodex mites reproduce sexually. In the male, the copulatory organs are located on the back between the limbs of the second pair; in the female, the genital opening is located ventrally at the level of the fourth pair of legs. Mating occurs at the mouth of the pilosebaceous canal. The female lays eggs inside the hair follicles and sebaceous glands; after 3–4 days, larvae appear, which mature and crawl to the surface of the skin, turning into a nymph. Then they again penetrate the hair follicle, where within 7 days they grow into sexually mature individuals. Dead mites decompose in the hair follicles or sebaceous glands. The total life cycle of Demodex is 2–3 weeks [13, 19].
Demodex mites have been found in all races and age groups. Their detection in people without signs of skin pathology ranges from 17 to 72%. In patients with rosacea, the detection of Demodex mites, especially when using highly sensitive methods (polymerase chain reaction and confocal microscopy), reaches 88%, and in perioral dermatitis - up to 58%. During therapy, a decrease in mite density was noted, which correlated with an improvement in clinical condition [28, 30]. Cases of detection of Demodex in newborns due to close contact with mite-infected mother's skin have been described. Due to the infants' low sebum production, they did not develop significant mite colonization. In children with various immunodeficiency conditions and during fasting, Demodex is detected more often [33]. The detection rate of ticks increases with age. In patients under 20 years of age, the prevalence of Demodex is 13–20%, increasing to 95–100% by age 70 years. According to D. Czepita et al. (2007), Demodex mites were detected in 13% of children aged 3 to 15 years, in 34% of adults aged 19 to 25 years, in 69% from 31 to 50 years, in 87% of subjects aged from 51 to 50 years. 70 years and in 95% of people aged 71 to 96 years [14]. It is assumed that in people over 45 years of age, mite activity is maintained by age-related changes in the skin and its glands, hormonal changes, and somatic pathology [29, 34].
Research by C. Casas et al. (2012) indicate a correlation between mite density and markers of skin immune system activation [28]. An increase in the amount of Demodex is noted in patients with chronic renal failure, diabetes mellitus, Behcet's disease, cancer, and HIV infection [35, 36, 37]. The density of mites in the skin can increase in unfavorable social and living conditions [38].
According to available data, with a decrease in immune reactivity caused by both natural (age and gender characteristics) and pathological (primary and secondary immunodeficiency states, oncological processes) changes in a person’s immune status [61, 62], the risk of developing mite-associated dermatitis increases genus Demodex. This may be due to both an imbalance in the production of various immune factors and severe immunosuppression. All of the above factors influence the reduction of local tissue immunity and the immunoreactivity of skin structures. The relationship between T and B cells is disrupted, as well as the production of immunoactive substances (cytokine cascade and interleukins production), and a decrease in CD4+ cell populations [63, 64, 65]. One or more of the factors described above significantly increase the risk of developing diseases associated with the activity of parasitic Demodex mites.
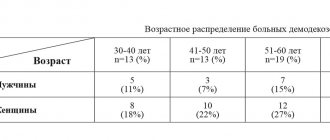
The results of studies on the extent of damage to men and women by Demodex mites are controversial. According to some data, contamination predominates in men, according to others – in women; in a number of studies, statistical differences were not established. Demodex folliculorum is detected more often than Demodex brevis; the ratio of their detection in men is 4:1, in women – 10:1 [1, 19].
The influence of the environment on the viability of Demodex mites has been studied. Their activity depends on the amount of light and heat. The favorable temperature for their development is 16–22 °C. In laboratory conditions, ticks are resistant to a wide range of antiseptic solutions for several hours, as well as to 10% povidone-iodine and 4% pilocarpine solution, and in 100% alcohol they die within a minute [39].
Diagnosis of Demodex mites
The use of modern sensitive diagnostic methods makes it possible to detect Demodex mites in almost 100% of patients, but their presence does not always indicate disease. To prescribe treatment, they are guided by the presence of more than 5 adult mites, larvae or eggs per 1 cm2 of skin surface and the corresponding clinical picture [38, 40]. There are various methods for detecting them:
- Standardized skin surface biopsy method.
The face is cleansed with water and a mild cleanser. After the skin has dried, about 0.05 ml of cyanoacrylate glue is applied to an area of 1 cm2 on a glass slide and distributed evenly. The slide is applied to the skin for 1–3 minutes (until the glue dries completely). A drop of immersion oil is added, covered with a coverslip and examined under a microscope at standard (10x10) magnification [41, 42]. - Direct microscopy method.
The face is cleansed with water and a mild cleanser. Mites are identified using light microscopy of native material obtained by scraping the contents of the sebaceous glands with a disposable scalpel or by extracting comedones. To examine eyelashes, they are epilated (10–15 pieces). The material is placed on a glass slide, a drop of 10–20% alkali solution (KOH) or glycerol is added, covered with a coverslip and examined under a microscope at standard magnification [43, 49]. - Examination of fingerprints using adhesive tape.
Before going to bed at night, cleanse your face with water. After the skin has dried, cellophane adhesive tape (2x5 cm) is applied to the forehead, cheeks, nose and chin. In the morning, the tape is removed and pressed against a glass slide. The drug is examined under a microscope at standard magnification. The degree of infestation is classified as weak when 1 to 10 ticks are detected, moderate when 11–30 ticks are found, or strong when more than 31 ticks are found in each zone [44]. - biopsy
using a punch or scalpel is performed according to a standard technique with sections stained with hematoxylin and eosin and subsequent histological examination. Perivascular and perifollicular lymphomacrophagic infiltrates, often with large numbers of neutrophils, sometimes with multinucleated macrophages, may be observed in the obtained samples. The pilosebaceous infundibulum and perifollicular infiltrate usually contain significant amounts of Demodex [30, 45]. - Dermatoscopy
allows visualization of Demodex on the surface of the skin. During dermatoscopy, so-called “mite tails” can be observed in the form of follicular and perifollicular yellowish threads [46, 47].
For diagnostic purposes, methods of electron microscopy, confocal laser scanning microscopy and high-definition optical coherence tomography, PCR are also used [28, 31, 32].
Clinical conditions associated with Demodex mites
Most people carry Demodex but do not develop clinical symptoms. One of the factors in the transition from clinically invisible colonization by mites to the development of dermatoses may be a state of primary or secondary immunosuppression. The development of the disease may be facilitated by a genetic predisposition; there may be a connection with special types of human leukocyte antigens [50, 52, 53].
Staphylococcus albus, Proteobacteria, Firmicutes, and Actinobacteria were found in the microenvironment of Demodex mites. Of interest are works that examine the association of Demodex mites with Bacillus oleronius. A study using skin testing showed that Demodex mites cause increased expression of the genes for interleukin IL-8, IL-1β, tumor necrosis factor-α, cyclooxygenase-1, etc. The immune status in response to the invasion of these mites remains poorly understood [51, 54, 55].
Skin lesions associated with Demodex mites are characterized by clustered, inflammatory papules and pustules, scaling, and a burning and itching sensation. The rashes are more often located within one anatomical region and have an irregular shape [56].
Various classifications of skin lesions caused by Demodex mites have been proposed. O.E. Akilov et al. (2005) proposed a classification of skin lesions from mites, taking into account their shape, location of the lesions and seasonality of exacerbations [57]. CH Yun et al. (2017) used a classification based on the area, shape and localization of lesions: diffuse lesions, when the rashes are located evenly over the entire surface of the facial skin; U-shaped arrangement - rashes are localized on the cheeks, chin and along the lower jaw line; T-shaped location - the rash is located predominantly on the forehead, nose and central part of the chin [42]. Many researchers divide demodicosis into primary, in which there are no symptoms of other inflammatory dermatoses, and secondary, in which excessive proliferation of Demodex mites is associated with other dermatoses, systemic diseases or due to treatment with calcineurin inhibitors, topical glucocorticosteroids, epidermal growth factor receptor inhibitors, etc. [48 , 57]. W. Chen and G. Plewig (2014) consider four types of facial skin lesions in primary demodicosis: 1 – pityriasis folliculorum with the participation of sebaceous and hair follicles without visible inflammation; 2 – papulopustular inflammatory elements localized in the perioral and periorbital areas; 3 – eye damage causing chronic blepharitis, chalazion or keratoconjunctivitis; 4 – damage to the skin of the ear canal, causing otitis externa [11].
Directions of therapy
The literature describes various groups of drugs that are used to eliminate Demodex mites: these are insecticides and anti-scabies (permethrin, crotamiton, lindane, benzyl benzoate), antiprotozoal and antimicrobial agents (ivermectin, metronidazole), as well as products containing salicylic acid and sulfur [58 , 59, 60]. It is important to note that in the instructions for use of the above products, only ivermectin contains instructions on the effect on Demodex mites.
Literature
- Litwin D., Chen W., Dzika E., Korycinska J. Human Permanent Ectoparasites; Recent Advances on Biology and Clinical Significance of Demodex Mites: Narrative Review Article. Iran J Parasitol 2017;12(1):12–21.
- Gross TL, Ihrke PJ, Walder EJ, & Affolter VK Skin diseases of the dog and cat: clinical and histopathologic diagnosis. Oxford: Blackwell Science Ltd; 2008. https://doi.org/10.1002/9780470752487
- Singh SK, Dimri U. The immuno-pathological conversions of canine demodicosis. Vet Parasitol. 2014;203(1–2):1–5. https://doi.org/10.1016/j.vetpar.2014.03.008
- Esenkaya Tasbent F., Dik B. A dog related Demodex spp. Infestation in a student: a rare Demodex case. Mikrobiyol Bul. 2018;52(2):214–220. https://doi.org/10.5578/mb.66410
- Zhao YE, Xu JR, Hu L., Wu LP, Wang ZP Complete sequence analysis of 18S rDNA based on genomic DNA extraction from individual Demodex mites (Acari: Demodicidae). Exp Parasitol. 2012;132(1):45–51. https://doi.org/10.1016/j.exppara.2012.02.025
- Lacey N., Ní Raghallaigh S., Powell F.C. Demodex mites-commensals, parasites or mutualistic organisms? Dermatology. 2011;222:128–130. https://doi.org/10.1159/000323009
- Schommer NN, Gallo RL Structure and function of the human skin microbiome Trends Microbiol. 2013;21(12):660–668. https://doi.org/10.1016/j.tim.2013.10.001
- Potekaev N.N., Arabian E.R., Sokolovsky E.V. and others. Acne and rosacea. M.; SPb.: BINOM; 2007.
- Hasan M., Siddiqui FA, Naim M. Human demodicidosis. Ann Trop Med Public Health 2008;1:70–71. https://doi.org/10.4103/1755-6783.50690
- Sędzikowska A., Osęka M., Skopiński P. The impact of age, sex, blepharitis, rosacea and rheumatoid arthritis on Demodex mite infection. Arch Med Sci. 2018;14(2):353–356. https://doi.org/10.5114/aoms.2016.60663
- Chen W., Plewig G. Human demodicosis: revisited and a proposed classification. Br J Dermatol 2014;170:1219–1225. https://doi.org/10.1111/bjd.12850
- Bikowski JB, Del Rosso JQ, Demodex dermatitis: a retrospective analysis of clinical diagnosis and successful treatment with topical crotamiton. J Clin Aesthet Dermatol 2(1); 2009; 20–25.
- Lacey N., Kavanagh K., Tseng SC Under the lash: Demodex mites in human diseases. Biochem (Lond) 2009;31(4):2–6.
- Czepita D., Kuźna-Grygiel W., Czepita M., Grobelny A. Demodex folliculorum and Demodex brevis as a cause of chronic marginal blepharitis. Ann Acad Med Stetin 2007;53(1):63–67.
- Rathi SK, Kumrah L. Topical corticosteroid-induced rosacea-like dermatitis: A clinical study of 110 cases. Indian J Dermatol Venereol Leprol 2011;77(1):42–46. https://doi.org//10.4103/0378-6323.74974
- Saraswat A., Lahiri K., Chatterjee M., Barua S., Coondoo A., Mittal A. et al. Topical corticosteroid abuse on the face: A prospective, multicenter study of dermatology outpatients. Indian J Dermatol Venereol Leprol 2011;77:160–166. https://doi.org//10.4103/0378-6323.77455
- Dhingra KK, Saroha V., Gupta P., Khurana N. Demodex-associated dermatologic conditions a coincidence or an etiological correlate. Review with a report of a rare case of sebaceous adenoma. Pathol Res Pract. 2009;205(6):423–426. https://doi.org//10.1016/j.prp.2008.11.013
- Sönmez O.U., Yalçın ZG, Karakeçe E., Çiftci I.H., Erdem T. Associations between Demodex species infestation and various types of cancer. Acta Parasitol. 2013;58(4):551–555. https://doi.org//10.2478/s11686-013-0178-y
- Sharma YK, Gupta A. Human Demodex mite: The versatile mite of dermatological importance. Indian J Dermatol 2014;59(3):302. https://doi.org//10.4103/0019-5154.131416
- Desch CE, Nutting WB Morphology and functional anatomy of Demodex folliculorum (Simon) of man. Acarologia 1978;19:422–462.
- Akbulatova L.K. Pathogenetic role of the Demodex mite and the clinical form of demodicosis in humans. Vestn dermatovener. 1963;40:57–61. .
- Ya-e Zhao, Jun-xian Ma, Li Hu, Li-ping Wu, Manuel De Rojas Discrimination between Demodex folliculorum (Acari: Demodicidae) isolates from China and Spain based on mitochondrial cox1 sequences. J Zhejiang Univ Sci B. 2013 Sep; 14(9): 829–836.
- Jing X, Shuling G, Ying L. Environmental scanning electron microscopy observation of the ultrastructure of Demodex. Microsc Res Tech. 2005; 68(5):284–289. https://doi.org//10.1002/jemt.20253
- Forton F., Germaux MA, Brasseur T., De Liever A., Laporte M., Mathys C., Sass U., Stene JJ, Thibaut S., Tytgat M., Seys B. Demodicosis and rosacea: epidemiology and significance in daily dermatologic practice. J Am Acad Dermatol. 2005;52:74–87. https://doi.org//10.1016/j.jaad.2004.05.034
- Namazi MR A possible role for human follicle mites in skin's defense against bacteria. Indian J Dermatol Venereol Leprol 2007;73:270.
- de Rojas M., Riazzo C., Callejón R., Guevara D., Cutillas C. Morphobiometrical and molecular study of two populations of Demodex folliculorum from humans. Parasitol. Res 2012;110(1):227–233. https://doi.org//10.1007/s00436-011-2476-3
- Hu L., Zhao YE, Cheng J., Ma JX Molecular identification of four phenotypes of human Demodex in China. Exp. Parasitol. 2014;142:38–42. https://doi.org//10.1016/j.exppara.2014.04.003
- Casas C., Paul C., Lahfa M., Livideanu B., Lejeune O., Alvarez-Georges S., Saint-Martory C., Degouy A., Mengeaud V., Ginisty H., Durbise E., Schmitt AM , Redoulès D. Quantification of Demodex folliculorum by PCR in rosacea and its relationship to skin innate immune activation. Exp Dermatol. 2012;21(12):906–910. https://doi.org//10.1111/exd.12030
- Yücel A., Yilmaz M. Investigation of the prevalence of Demodex folliculorum and Demodex brevis in rosacea patients. Turkiye Parazitol Derg. 2013; 37(3):195–198. https://doi.org//10.5152/tpd.2013.43
- Ríos-Yuil JM, Mercadillo-Perez P. Evaluation of Demodex folliculorum as a Risk Factor for the Diagnosis of Rosacea in Skin Biopsies. Mexico's General Hospital (1975-2010). Indian J Dermatol. 2013; 58(2):157. https://doi.org//10.4103/0019-5154.108069
- Turgut Erdemir A., Gurel MS, Koku Aksu AE et al. Demodex mites in acne rosacea: Reflectance confocal microscopic study. Australas J Dermatol. 2017;58(2):e26–e30. https://doi.org//10.1111/ajd.12452
- Sattler EC, Hoffmann VS, Ruzicka T. et al. Reflectance confocal microscopy for monitoring the density of Demodex mites in patients with rosacea before and after treatment. Br J Dermatol. 2015; 173(1):69–75. https://doi.org//10.1111/bjd.13783
- Kaya S., Selimoglu MA, Kaya OA, Ozgen U. Prevalence of Demodex folliculorum and Demodex brevis in childhood malnutrition and malignancy. Pediatric Int. 2013;55(1):85–89. https://doi.org//10.1111/j.1442-200X.2012.03740.x
- Zomorodian K., Geramishoar M., Saadat F., Tarazoie B., Norouzi M., Rezaie S. Facial demodicosis. Eur J Dermatol. 2004;14:121–122.
- Karincaoglu Y., Esrefoglu Seyhan M., Bayram N., Aycan O., Taskapan H. Incidence of Demodex folliculorum in patients with end stage chronic renal failure. Ren Fail. 2005;27(5):495–499.
- Emre S., Aycan OM, Atambay M., Bilak S., Daldal N., Karincaoglu Y. What is the importance of Demodex folliculorum in Behçet's disease? Turkiye Parazitol. Derg. 2009;33(2):158–161.
- Inci M., Kaya OA, Inci M. Yula E., Gökçe H., Rifaioğlu MM, Demirtaş O., Yengil E. Investigating Demodex folliculorum in patients with urological cancer. Turkiye Parazitol Derg 2012;36(4):208–210. https://doi.org//10.5152/tpd.2012.50
- Zeytun E., Tilki E., Doğan S., Mumcuoğlu KY The effect of skin mois-ture, pH, and temperature on the density of Demodex folliculorum and Demodex brevis (Acari: Demodicidae) in students and staff of the Erzincan University, Turkey . Int J Dermatol. 2017; 56(7):762–766. https://doi.org//10.1111/ijd.13600
- Zhao YE, Guo N., Wu LP Influence of temperature and medium on viability of Demodex folliculorum and Demodex brevis (Acari: Demodicidae). Exp Appl Acarol. 2011;54(4):421–425. https://doi.org//10.1007/s10493-011-9445-5
- Sirmais N.S., Abesadze G.A., Ustinov M.V. Demodicosis: pathogenetic aspects for various facial dermatoses. Pos. method M: 2013; 26 p.m. .
- Forton F. Standardized skin surface biopsy: method to estimate the Demodex folliculorum density, not to study the Demodex folliculorum prevalence. J Eur Acad Dermatol Venereol. 2007;21:1301–1302.
- Yun CH, Yun JH, Baek JO, Roh JY, Lee JR Demodex mite density determinations by standardized skin surface biopsy and direct microscopic examination and their relations with clinical types and distribution patterns. Ann Dermatol. 2017;29(2):137–142. https://doi.org//10.5021/ad.2017.29.2.137
- Aşkin U., Seçkin D. Comparison of the two techniques for measurement of the density of Demodex folliculorum: standardized skin surface biopsy and direct microscopic examination. Br J Dermatol. 2010;162(5):1124–1126. https://doi.org//10.1111/j.1365-2133.2010.09645.x
- Zhao YE, Guo N., Xun M., Wang M., Wang DL Sociodemographic characteristics and risk factor analysis of Demodex infestation (Acari: Demodicidae) J Zhejiang Univ-Sci B (Biomed & Biotechnol) 2011;12(12):998 –1007. https://doi.org//10.1631/jzus.B1100079
- Hsu CK, Hsu MM, Lee JY Demodicosis: a clinicopathological study. J Am Acad Dermatol. 2009;60:453–462. https://doi.org//10.1016/j.jaad.2008.10.058
- Segal R., Mimouni D., Feuerman H. Dermoscopy as a diagnostic tool in demodicidosis. Int J Dermatol. 2010;49(9):1018–1023.
- Errichetti E., Stinco G. Dermoscopy in general dermatology: a practical overview. Dermatol Ther (Heidelb). 2016;6(4):471–507. https://doi.org//10.1007/s13555-016-0141-6
- Friedman P., Sabban EC, Cabo H. Usefulness of dermoscopy in the diagnosis and monitoring treatment of demodicidosis. Dermatol Pract Concept. 2017;7(1):35–38. https://doi.org//10.5826/dpc.0701a06
- Gutova V.P., Nozdrin V.I., Guzev K.S., Ganushkina L.A. A method for assessing the lifespan of Demodex folliculorum mites in vitro. M., JSC "Retinoids" 2015;34:62–64.
- Mumcuoglu KY, Akilov OE The role of HLA A2 and Cw2 in the pathogenesis of human demodicosis. Dermatology. 2005;210(2):109–114. https://doi.org//10.1159/000082565
- Murillo N., Aubert J., Raoult D. Microbiota of Demodex mites from rosacea patients and controls. Microb Pathog. 2014;71-72:37–40. https://doi.org//10.1016/j.micpath.2014.04.002
- O'Reilly N., Bergin D., Reeves EP, McElvaney NG, Kavanagh K. Demodex-associated bacterial proteins induce neutrophil activation. Br J Dermatol. 2012;166:753–760. https://doi.org//10.1111/j.1365-2133.2011.10746.x
- O'Reilly N., Gallagher C., Reddy Katikireddy K., Clynes M., O'Sullivan F., Kavanagh K. Demodex-associated Bacillus proteins induce an aberrant wound healing response in a corneal epithelial cell line: possible implications for corneal ulcer formation in ocular rosacea. Invest Ophthalmol Vis Sci. 2012;53(6):3250-3259. https://doi.org//10.1167/iovs.11-9295
- McMahon F., Banville N., Bergin DA, Smedman C., Paulie S., Reeves E., Kavanagh K. Activation of neutrophils via IP3 pathway following exposure to Demodex-associated bacterial proteins. Inflammation. 2016;39:425–433. https://doi.org//10.1007/s10753-015-0264-4
- Koller B., Muller-Wiefel AS, Rupec R., Korting HC, Ruzicka T. Chitin modulates innate immune responses of keratinocytes. PLoS ONE. 2011;6:1562. https://doi.org//10.1371/journal.pone.0016594
- Reken M., Schaller M., Sattler E., Burgdorf W. Atlas of dermatology. M.: Medpress-inform, 2018; 408 p.
- Akilov OE, Butov YS, Mamcuoglu KY A clinicpathological approach to the classification of human demodicosis. J Dtsch Dermatol Ges. 2005; 3:607–614. https://doi.org//10.1111/j.1610-0387.2005.05725.x
- Cardwell LA, Alinia H., Moradi Tuchayi S., Feldman SR New developments in the treatment of rosacea – role of once-daily ivermectin cream Clin Cosmet Investig Dermatol. 2016; 9: 71–77. https://doi.org//10.2147/CCID.S98091
- Abokwidir M., Feldman S.R. Rosacea Management. Skin Appendage Disord. 2016;2(1-2):26–34. https://doi.org//10.1159/000446215
- Jarmuda S., O'Reilly N., Zaba R., Jakubowicz O., Szkaradkiewicz A., Kavanagh K. Potential role of Demodex mites and bacteria in the induction of rosacea. J Med Microbiol. 2012;61(Pt 11):1504–1510. https://doi.org//10.1099/jmm.0.048090-0
- Nakagawa T., Sasaki M., Fujita K., Nishimoto M., Takaiwa T. Demodex folliculitis on the trunk of a patient with mycosis fungoides // Clin Exp Dermatol. 1996; 21: 148–150. [PubMed: 8759206].
- Gothe R. Demodicosis of dogs — a factorial disease? // Berl Munch TierarztlWochenschr. 1989; 102:293–297. [PubMed: 2679540].
- Butov Yu.S., Akilov O.E. Factors for successful colonization by Demodex spp. human skin // Vestn. postgraduate honey. image. 2002; 1:87.
- Butov Yu.S., Akilov O.E. The role of immune disorders in the pathogenesis of skin demodicosis // Ros. magazine skin and venereal bol. 2003; No. 3, p. 65–68.
- Rufli T., Buchner SA T-cell subsets in acne rosacea lesions and the possible role of Demodex folliculorum // Dermatologica. 1984; 169:1–5.
Seal
Folk remedies
For the combined treatment of diseases caused by glandular fever, not only medications are used, but also folk remedies.
It is important to understand that they will not help without comprehensive treatment, because the tick has great survival and adaptability.
Folk remedies are mainly herbal treatments; they may also have contraindications, so before using any treatment, carefully study its effect.
Wormwood decoction
Prepare as follows: 2 tbsp. spoons of dry herb are poured with boiling water and boiled for five minutes, then infused for three hours. The drug is taken orally.
It helps not only to cope with ticks, but also to cleanse the body. Every day you need to prepare a fresh decoction. You can combine it with honey to improve the taste.
Blackcurrant decoction
The recipe is very simple: 4 tbsp. Boil tablespoons of dried black currants in two glasses of water for 10 minutes, then leave for half an hour. Gauze soaked in the broth is applied to the face.
Tansy tincture
Tansy is known for its anti-inflammatory properties. With demodicosis, it relieves inflammation of the eyelids and blocks the reproduction of mites.
To prepare the infusion, take 1 tbsp. spoon of tansy flowers, pour a glass of boiling water and leave for 1.5 hours. The infusion is used to make lotions on inflamed areas for 1.5 months.
Propolis has antibacterial and anti-inflammatory properties. Therefore, before applying acaricidal ointments, you can wipe your face with an alcoholic infusion of propolis. This helps the facial skin heal quickly.
Celandine ointment
A glass of fresh washed celandine roots is poured with a glass of sunflower oil and left in the sun for two weeks. Then filter into a dark glass bottle and store in the refrigerator. Before applying to the face, mix with sour cream.
Tea tree oil
This remedy is successfully used to treat demodicosis as a strong natural antiseptic. It is safe for humans, but ticks cannot tolerate it.
The oil normalizes the activity of the sebaceous glands, dries the skin, and penetrates deep into the pores of the skin. Ticks die from it. Important: avoid getting oil in your eyes!
Treatment
Demodicosis rarely occurs as a separate, independent disease. More often, parasitism of iron mites in the skin of the face accompanies other skin diseases: various forms of rosacea, perioral dermatitis, acne, etc. Apparently, the intensive reproduction of mites in the host’s skin reflects some complex, systemic problems of the body, and primarily its immune system. Therefore, it is first necessary to treat the underlying skin disease, as well as organize a comprehensive examination.
Often, when the number of iron mites is high, local acaricidal preparations are prescribed, the active ingredients of which are benzyl benzoate and pyrethroids.
One of the first and most important stages of treatment is carrying out sanitary and hygienic measures in the immediate environment of the patient. Personal items (towels, pillowcases, etc.) must be washed at a water temperature of at least 75 °C; replace feather pillows with pillows with synthetic filling, use anti-allergenic protective covers to be able to wash them. But such pillows, as a rule, are recommended to be washed at a temperature no higher than 40–45 ° C, as a result of which it is necessary to use special acaricidal additives in the wash (for example, Akaril, Allergoff), which allow the destruction of mites at a lower washing temperature.