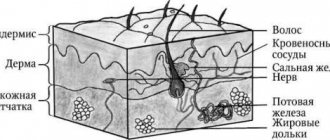
A nevus is a benign skin tumor, popularly called a mole or birthmark. The name comes from the Latin Naevus, because. the tumor consists of nevoid cells. Appearing on the human body as a result of environmental influences, such formations can be localized in any part of the body, not excluding the mucous membranes. Nevi can vary in shape and size, appear as a flat spot or pea, and their color varies from light to dark brown. The number of moles changes throughout life; they are almost never found in newborn children, but in adolescence they appear in almost everyone.
Main types of nevi
- Giant pigmented nevus is usually of congenital origin. These extensive formations can be located on the limbs, face, torso, even the smallest of them can reach a diameter of up to 20 cm.
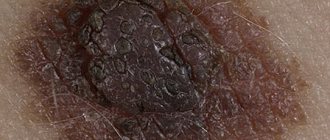
- Epidermodermal nevi are different stages of the transition of epidermal melanocytic structures into the dermis, as well as the initial stage of development of its intradermal part. This can only be determined by histological examination (see Fig. 2)
- Intradermal nevus is the most common. This form is characterized by localization at different levels of the dermis, and a combination of different stages of appearance is possible. In its development, this type of mole goes through several stages: resumption of borderline activity and transition to a complex form, spontaneous focal or complete regression, appearance of a nodular or superficially growing melanoma against the background of a nevus (see Fig. 3)
- Epidermal melanocytic nevi - differ in size, shape, degree of pigmentation, as well as the nature of the surface. The most common are flat moles, the sizes of which vary from 0.1 to 10 cm (see Fig. 4)
- Blue nevus is a melanocytic type with a rare primary localization of the process in the dermis. Most often it affects the skin of the face, limbs, and buttocks.
- Halonevus or Setton's nevus - occurs in most cases in adolescence; their appearance in a later period may indicate the presence of a serious pathology. This species is characterized by the appearance of a white corolla around a brown mole (see Fig. 5)
- Papillomatous nevus - protrudes on the surface of the skin and has an irregular shape, resembling a cauliflower in appearance. It attracts attention with its repulsive appearance (see Fig. 6).
- Fibroepithelial nevus - this type of tumor is characterized by a rounded dome-shaped shape, the size of the formation is 0.3-1.5 cm. The color is close to the color of the skin. Due to exophytic growth, they are often injured, but malignancy is extremely rare (see Fig. 7).
Borderline nevi are formations that rise slightly above the surface of the skin, but without a specific localization. Their sizes are usually 0.2-0.5 cm, the color can be from light to dark brown. Formations of this type have clear cytological, topographic and architectural features. At the level of the epidermal junction in the basal layer of the epidermis, they form spherical structures, large nests, and, less commonly, zones of diffuse melanocytic transformation (see Fig. 7-10).- Reed's nevus is very dangerous due to its possible degeneration into melanoma. A tumor of this type is characterized by a combination of signs of juvenile and dysplastic nevi (see Fig. 8).
- Dysplastic nevus or Clark's nevus is the most dangerous type of tumor. According to statistics, half of them develop into melanoma. A flat, irregularly shaped mole has an uneven color. It is characterized by three stages of dysplasia, the third being the stage preceding melanoma. The reverse process is possible, but complex forms can also appear, which means either the reversibility of the stage or incomplete completion. The development of a complex nevus is characterized by several stages: 1) transition to an intradermal form; with the activation of borderline activity, a transition to a complex form is possible; 2) spontaneous regression (reverse development); 3) transition to melanoma.
Website of dermatovenerologist Betekhtin M.S.
When examining a patient, you can often find skin changes that the patient was not aware of or that did not bother him. This accidental finding was an anemic nevus in a patient who came for an examination of melanform nevi.
Anemic nevus
Anemic nevus is a congenital vascular anomaly that clinically manifests itself as a light spot. The reason for this is the increased sensitivity of blood vessels to catecholamines, which cause vasospasm. Judging by the reports of some authors, anemic nevus is not a common condition, occurring in 1-2% of the population (1). Early publications indicated a higher incidence of such nevus among women. But a review of the literature related to anemic nevus arising from neurofibromatosis type 1 describes an equal frequency among women and men (2). Anemic nevus can be detected at birth or in early childhood.
Evidence of vasospasm, the main cause of the appearance of nevus, is a number of the following observations. In anemic nevus, intralesional administration of bradykinin, acetylcholine, serotonin, nicotine, 5-hydroxytryptamine and histamine does not cause the expected vasodilation or redness in the affected area. If the nevus is located on the arm, sympathetic axillary blockade of the affected arm or intradermal administration of an alpha-blocker (pilocarpine) causes erythema to appear at the site of the nevus. It is also assumed that in the pathogenesis of nevus there is an abnormality in the production of endothelial adhesion molecule (expression of E selectin).
Clinically, an anemic nevus appears as an oval or linear pale spot with clear, irregular borders, which may be surrounded by satellite spots. The rashes can be single or multiple and can be located on any part of the skin, but most often they are located on the upper chest. Friction or other mechanical stress on the surrounding skin may make the stain more noticeable. Clinical manifestations of an anemic nevus usually exist without changes throughout life, and in the absence of the syndromes described below do not affect the state of health and life expectancy. If you have an anemic nevus in a child with multiple “coffee spots,” you should remember about neurofibromatosis type 1. Two prospective studies reported a 50% incidence of anemic nevus in neurofibromatosis type 1 (1,2). Anemic nevus, occupying large areas, is usually observed in close association with capillary malformations of the port-wine stain type, a phenomenon attributed to somatic recombination. Anemic nevus in combination with telangiectatic nevus may be associated with abnormalities in the development of cerebral vessels - cerebral hemiatrophy (Dyke-Davydov-Masson syndrome) (4). Anemic nevi have also been described in patients with pigmentovascular phakomatosis, a syndrome characterized by vascular and melanoform nevi (5,6). Pigmented vascular phakomatosis type IIa (according to Hazegawa and Yasuhara) is associated with primary choroidal melanoma (7).
Differential diagnosis should be made with achromic nevus, pityriasis versicolor, vitiligo, post-inflammatory hypopigmentation, tuberous sclerosis (ash leaf spots), progressive macular hypomelanosis and scars. A number of simple diagnostic procedures can clarify the diagnosis of anemic nevus. With diascopy, the nevus becomes indistinguishable from the surrounding skin, which turns pale when pressed with glass. Because There is no loss of melanin in an anemic nevus, then examination under a Wood’s lamp makes the nevus invisible, unlike true depigmenting conditions. Friction, cold or heat do not cause changes in these nevi. When attempting to induce dermatographism by drawing a line through the nevus and surrounding skin, erythema occurs only on the surrounding skin and not on the nevus itself.
Treatment for anemic nevus is not required. If necessary, the patient can apply camouflage agents. There is no cure.
1. Marque M, Roubertie A, Jaussent A, Carneiro M, Meunier L, Guillot B, et al. Nevus anemicus in neurofibromatosis type 1: a potential new diagnostic criterion. J Am Acad Dermatol. 2013 Nov. 69(5):768-75. [Medline].
2. Hernández-Martín A, García-Martínez FJ, Duat A, López-Martín I, Noguera-Morel L, Torrelo A. Nevus anemicus: a distinctive cutaneous finding in neurofibromatosis type 1. Pediatr Dermatol. 2015 May-Jun. 32 (3):342-7. [Medline].
3. Ferrari F, Masurel A, Olivier-Faivre L, Vabres P. Juvenile xanthogranuloma and nevus anemicus in the diagnosis of neurofibromatosis type 1. JAMA Dermatol. 2014 Jan. 150(1):42-6. [Medline].
4. Ruggieri M, Polizzi A, Strano S, Schepis C, Morano M, Belfiore G, et al. Mixed vascular nevus syndrome: a report of four new cases and a literature review. Quant Imaging Med Surg. 2016 Oct. 6(5):515-524. [Medline].
5. Ahkami RN, Schwartz RA. Nevus anemicus. Dermatology. 1999. 198(4):327-9. [Medline].
6. Castori M, Rinaldi R, Angelo C, Zambruno G, Grammatico P, Happle R. Phacomatosis cesioflammea with unilateral lipohypoplasia. Am J Med Genet A. 2008 Feb 15. 146A(4):492-5. [Medline].
7. Tran HV, Zografos L. Primary choroidal melanoma in phakomatosis pigmentovascularis IIa. Ophthalmology. 2005 Jul. 112(7):1232-5. [Medline].
Treatment
Treatment of nevi is indicated only in cases where there are signs of transition to a malignant formation. However, in cases where there is a high probability of injury to the mole, its removal is recommended. To select the appropriate method, the size of the tumor is taken into account, as well as its condition and the presence of signs of malignancy. Among the most commonly used treatment methods are:
- Destruction using a laser or electrocoagulator - excision under the influence of high temperatures or a laser. With the electrocoagulation method, the vessels are cauterized during the procedure, so the risk of bleeding is eliminated. The laser affects the deep layers of the skin, but healthy areas are not affected. This method is recommended for removing small moles.
- Chemical destruction - based on the destructive action of chemicals. It should be taken into account that incomplete removal of a mole threatens the development of a malignant process. Therefore, the most effective method is still surgery.
Surgical operations
Large papillomatous nevus undergoes surgical excision. The application of small cosmetic stitches after the removal operation guarantees minimal cosmetic defects. The possibility of relapse is excluded, since along with the nevus, the doctor also captures part of the healthy tissue when removing it. Giant nevi are also treated surgically. They are rare, but the risk of developing cancer in them is very high. Treatment of giant pigmented nevus is carried out in stages, with the involvement of plastic surgeons for further cosmetic operations.
Currently, there is no method that can prevent the appearance of a nevus. The only thing that can be avoided is the transformation of a nevus into melanoma. To do this, you just need to make sure that the nevus is not injured. Under no circumstances should you engage in self-extraction and self-diagnosis of nevi, as this may lead to undesirable consequences. Do not neglect your health, and if a large mole appears or damages an existing one, consult a doctor immediately.
Popular methods for removing nevi
Removal of nevi in Moscow involves the possibility of using a number of minimally invasive methods; the most popular are:
- cryodestruction, that is, exposure to very low temperatures (freezing), the conductor is liquid nitrogen, which allows you to remove nevi in the epidermis and dermis, but does not make it possible to control the depth of exposure; in addition, there is a certain risk of affecting nearby tissues, which can lead to burns and scars;
- laser, or gentle selective exposure to laser radiation exclusively on pathological tissues at different depths (can be set by settings); does not cause skin burns, does not leave scars;
- cauterization with current, or electrocoagulation, when pathological tissues are destroyed under the influence of high-frequency current, suitable only for superficial (epidermal) neoplasms;
- chemical cauterization, which is used less and less due to the high risk of damage to healthy skin.
When it comes to eliminating a malignant nevus, only surgical excision
. Any minimally invasive method can provoke rapid tumor development. If they are benign in nature, it is preferable to remove nevi with a laser. It is fast, safe, does not cause side effects or scars on the skin. At DECA, the procedure is carried out using high-tech Italian equipment.
Do you need a consultation with a dermato-oncologist? Do you want to get rid of nevi? Call!
When does a nevus need to be removed?
Of course, it is better to remove all melanoma-dangerous nevi before they begin to malignize. As for melanoma-free moles, most often they are removed for the following reasons:
- a person wants to get rid of a noticeable defect on the skin;
- the nevus can be accidentally damaged by rubbing body parts or during hygiene procedures, which is dangerous due to possible malignancy caused by damage;
- the process of malignancy began, and the nevus began to transform into a malignant tumor.
All nevi that are on a person’s body and face should be under constant observation. The slightest changes may indicate the beginning of the process of malignancy. We strongly recommend that you do not hesitate to contact a dermato-oncologist if you notice:
- growth (increase in size);
- color change;
- hair loss from the surface;
- bleeding;
- itching or burning;
- change in shape, “blurring” of edges.
The dermato-oncologist will prescribe a histological examination, which will confirm or not confirm your suspicions. In any case, such a nevus must be removed.