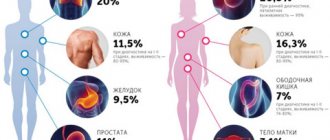
HPV occurs in men at approximately the same frequency as in women.
It is a mistake to believe that the fair sex, for some reason, becomes infected with the pathogen more often.
Infection occurs with the same frequency, it’s just that symptoms of the disease develop more often in women.
When patients see a dermatologist, they wonder what kind of disease it is, HPV, and what its features are.
How does the disease manifest itself, and how to get rid of it?
Pathogen
The human papillomavirus in men may not manifest itself in any way for many years after infection. This feature of the pathogen makes it dangerous, since a person does not know about his carriage, but at the same time spreads the disease. The virus is a DNA virus that parasitizes epithelial cells, disrupting their division cycle. Uncontrolled proliferation contributes to the formation of growths.
To date, science has identified more than 100 types of papillomavirus. A feature of the pathogen is the provocation of oncological processes, therefore all HPVs are divided into two groups:
- strains with a high risk of oncogenic complications;
- strains with a low risk of oncogenic complications.
The first group causes damage to the genital organs and promotes the formation of condylomas in the anogenital area. Growths are observed not only in the groin, but also on the penis. The second group provokes the formation of warts over the entire surface of the body.
Natural Treatment for Condyloma
- Apple Cider Vinegar – Soak a piece of cotton wool in apple cider vinegar and soak the affected area and leave it on for a while.
- Pineapple juice - apply fresh pineapple juice to cotton wool or, better yet, gauze, hold the preparation on the condyloma for about 10 minutes, then rinse. The procedure should be repeated twice a day.
- Aloe Vera – Apply a thick layer of Aloe Vera gel to the area affected by warts. Repeat the procedure 2-3 times a day for at least 2 weeks.
- Tea Tree Oil – Apply 3 drops of tea tree oil to gauze and apply to the infected area. Tea tree is known for its anti-inflammatory, antiseptic and antifungal effects.
- Eat as healthy as possible.
- Wear clean underwear.
- Pay attention to the dryness of the genital area; sweating creates conditions for the proliferation of bacteria and fungi.
- Do not touch or scratch genital warts.
- Avoid intercourse because it not only causes pain and discomfort, but can also cause more problems for your sexual partner.
- Do not try to pick or squeeze genital warts, as this may lead to a more serious infection.
Symptoms of the disease
Answering the question of how the human papillomavirus manifests itself in men, it should be noted that very often it is asymptomatic. The formation of growths is promoted by immunodeficiency conditions, stressful situations or hypothermia of the body. Doctors recommend seeking medical help if you experience the following symptoms.
- Genital condylomas. Formations on the skin that resemble cauliflower inflorescences are flesh-colored and can be located singly or in groups.
- Flat condylomas. Concentric formations that do not rise above the mucosa. They have a high cancer risk and therefore require a biopsy.
- Tissue dysplasia or disruption of their structure. The condition is dangerous due to the appearance of atypical cells and the development of oncological pathology.
How papillomavirus is transmitted, risks
Papillomavirus enters the human body in different ways, the probability of infection is 60%. You can get an infection in the following ways:
- Sexually, regardless of the type of sexual relations - oral, genital and anal. The presence of genital warts in a partner guarantees infection by 98-100%.
- Contact household - in the case of using a shared towel, washcloths, etc. The virus can also be transmitted through saliva during a kiss.
- Through wounds - a violation of the integrity of the skin and mucous membranes - an open gateway to the body.
- Infection of a child during the passage of the birth canal - children suffer from rare forms, papillomas grow in the nasopharynx and sinuses. Recent studies have shown that children born by cesarean section also become infected - this may indicate that the virus is able to penetrate the placenta.
Infection does not always guarantee the development of the disease. HPV causes disease in the body in 50% of cases, the rest are limited to carriage of the infection: a strong immune system can keep the virus in numbers that are not dangerous to the body. The incubation period ranges from a year to 20 years, with an average of 3-5 years.
The development of the disease is provoked by hormonal imbalances, immunodeficiency states, and sexually transmitted infections (STDs, STIs). Any condition that reduces immunity increases the risk - pregnancy, bad habits, chronic diseases, stress, etc.
It should be understood that infection of epithelial cells is a necessary but not sufficient factor for the development of oncology. According to Professor V.A. Molochkov, a well-known and respected scientist in the world of medicine, a number of other factors are necessary for the development of irreversible neoplasia:
- active expression of genes E6, E7 of highly oncogenic types hpv16 and hpv18;
- induction of estradiol metabolism to 16-OH;
- multiple damage to chromosomal DNA in an infected cell.
The first stage of CIN I neoplasia is expressed by active copying of the virus and its asymptomatic course. Tumor development is stimulated by the interaction of papillomavirus with cytomegaloviruses, trachomatis, mycoplasmas, ureaplasmas, and herpes simplex virus type 2.
Methods of infection
- Sexual, with vaginal or anal contact.
- Vertical, a newborn can be infected through a woman's birth canal.
- Self-infection, by transferring infection from one part of the body to another.
- A household contact virus, the virus remains active on hygiene items; it can be picked up in gyms and swimming pools.
- Contact, infection occurs through damaged skin or mucous membranes.
Synthetic antiviral topical drugs
This group of drugs can be roughly divided into drugs used for genital herpes infection and antiviral drugs prescribed for the treatment of papillomas and condylomas associated with papillomavirus infection.
Local medications for genital herpes
Several drugs registered in the Russian Federation are used for the treatment and prevention of relapses of genital herpes.
Tromantadine
An antiviral drug for herpes, an adamantane derivative (similar to the well-known antiviral drugs rimantadine and amantadine). Inhibits the attachment of the virus to the surface of the cell membrane, preventing the pathogen from penetrating into the cell. Prevents cell fusion and makes it difficult for the virus to spread by changing the synthesis of glycoproteins [5]. Available in the form of a gel for external use, which can be applied to mucous membranes during exacerbation of HSV infection [5].
Vacation: without prescription.
!
There is evidence of the development of a contact allergic reaction when using the drug [7].
Sodium aminodihydrophthalazindione
An immunomodulator capable of regulating the activity of innate and acquired immune cells, including macrophages, neutrophils and natural killer cells. At the same time, this antiviral drug against herpes increases the body's resistance to bacterial, viral and fungal infections, reducing their frequency, severity and duration (5). In addition, the drug normalizes the formation of antibodies and regulates the production of interferons, and also blocks the excessive synthesis of pro-inflammatory cytokines and reduces the level of oxidative stress (5).
Vacation: Without prescription
+
High safety profile (5).
Azoximer bromide
A Russian drug supposedly exhibiting an immunostimulating effect. According to the instructions [5], it directly affects phagocytes and natural killer cells, stimulates the formation of antibodies and the synthesis of interferon, and exhibits antioxidant and detoxifying properties. In domestic practice, it is used for a wide range of diseases - from influenza to malignant neoplasms.
Azoximer bromide vaginal suppositories are used to prevent recurrence of genital herpes.
Vacation: without prescription.
+
High safety profile. According to the manufacturer [5], no side effects have been reported.
!
Azoximer bromide suppositories are not indicated for the treatment of active herpes!
Establishing diagnosis
Before treating human papillomavirus in men, the pathology must be confirmed by laboratory tests. After the examination, the doctor may prescribe the following tests:
- urethroscopy;
- urethral smear;
- PCR;
- biopsy of growths.
Since condylomas have an oncological risk, you should not delay your visit to the doctor. Timely treatment allows you to stop the disease and minimize its consequences.
Clinical manifestations
Patients with condylomatosis may experience discomfort in the lower abdomen.
They are short-term, mild in nature.
Men rarely attach importance to them, citing other possible problems.
There are burning and itching sensations in the places where condylomas form.
Pain during intercourse is often noted.
The general condition may be accompanied by discharge from the urethra.
Delaying going to the doctor can lead to the development of new symptoms.
Their appearance indicates the involvement of other organs in the process.
Patients begin to complain of weakness, apathy, and lack of physical strength.
Headaches develop, and body temperature may increase.
It is often accompanied by chills and lethargy.
Therapy
When figuring out how to cure the papilloma virus in men, it is worth understanding that it will not be possible to completely get rid of the pathogen. Modern means can only stop the development of the process and remove the consequences of the pathogen’s activity.
There are general and local therapy. General assumes the following appointments:
- antiviral drugs;
- immunomodulators.
Local treatment of human papillomavirus in men involves removing growths. This can be done using the following methods:
- cryodestruction;
- electrocoagulation;
- cauterization with chemicals;
- thermal exposure by laser;
- electrosurgical method.
The procedure to remove growths is either painless or performed under local anesthesia. Timely therapy can significantly reduce the severity of symptoms and prevent HPV damage to large areas.
Local immunomodulators for HPV and HSV
Among the “universal” drugs that can be prescribed for various viral infections - from common respiratory infections to herpes and human papillomavirus - are interferons. In particular, preparations of human recombinant interferon alpha-2b.
Interferon alpha-2b has antiviral, immunomodulatory and antiproliferative properties. It suppresses the replication of RNA and DNA viruses, enhances the activity of macrophages, and increases the cytotoxicity of lymphocytes to target cells. The use of drugs containing interferon alpha-2b is accompanied by an increase in the level of immunoglobulins type A and normalization of IgE [5]. However, these therapeutic effects are fully manifested when the drug is administered systemically.
when its high concentration in the blood is reached. It should be noted that quite powerful side effects can develop, including fever, loss of appetite, headaches, muscle pain, joint pain and many other adverse reactions.
Due to the specific safety profile, injectable interferon preparations are prescribed only in very serious cases, when the risk of side effects is justified - for example, in the treatment of hepatitis, a number of oncological diseases, etc. HSV and HPV infections do not apply to such situations and are not indications for systemic interferon administration. At the same time, the Russian Federation has registered a very impressive list of local forms of interferon alpha-2b, including ointments/creams for treating mucous membranes with genital herpes.
Theoretically, local interferon preparations should have all the advantages of injectable ones and not have their side effects, since local forms are either very slightly absorbed into the systemic circulation or do not penetrate into the blood at all. However, today there is no sufficiently reliable evidence of the effectiveness of interferons when applied topically. However, in domestic practice they are quite often prescribed as part of the complex treatment of recurrent genital herpetic infections.
Along with local forms containing only interferon alpha-2b, several combination drugs are also registered in the Russian Federation:
- Interferon alpha-2b + acyclovir + lidocaine, ointment. Indications: HSV.
- Interferon alpha-2b + taurine + benzocaine, vaginal and rectal suppositories, prescription. Indications: HSV, HPV. Taurine, according to the instructions, acts in combination as a reparative, antioxidant and anti-inflammatory component.
+
High safety profile.
!
The feasibility of using local forms of acyclovir for genital herpes is subject to serious doubts due to insufficient activity, which is confirmed in Western recommendations [3]. Interferon alpha-2b preparations, both mono- and combined, are available with or without a prescription, depending on the indications of the dispensing rules in the instructions for a particular drug. It is important to draw the visitor’s attention to the fact that the first-line treatment for HPV - oral forms of acyclovir and valacyclovir - must be prescribed by a doctor, so you should be advised to immediately consult a doctor.