Human papillomavirus, commonly abbreviated as HPV.
This is the causative agent of the most common infectious pathology of mucous membranes and skin throughout the world, the so-called. papillomavirus infection.
There are about 200 types of this virus.
About a fifth of which can be transmitted through sexual contact, damaging the organs of the urogenital system.
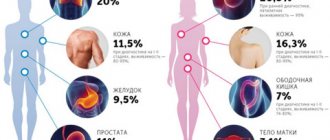
This pathogen is of particular concern due to the connection between infection and cancer pathologies.
Thus, 93% of episodes of cervical cancer in women are caused by this particular virus, of which 70% are HPV types 16 and 18.
That’s why, if a woman’s HPV 16 is detected in tests during an examination, the doctor strongly recommends additional studies.
So what is it: HPV 16 genotype in women?
All papillomaviruses are conventionally divided into three main groups depending on their oncogenic danger:
- non-oncogenic, causing flat/plantar/vulgar warts (types 1, 3, 2, 4, 41, 10, etc.), not capable of causing malignant transformations
- low risk, causing the development of anogenital warts (otherwise called genital warts), resembling characteristic cauliflower buds, epidermoplasia verrucous, laryngeal papillomatosis (types 5, 17, 12, 6, etc.), can extremely rarely, under very “favorable” conditions, cause malignant process
- high risk, capable of causing neoplastic changes in women in the area of the uterine cervix, bowenoid papulosis (HPV types 16 and 18, 33, 31, 39, 35, 58, 56, 45, 68, 59, 52, 51), have been proven to provoke the overlap of various factors oncological processes
Thus, the answer to the question of whether HPV 16 infection is dangerous for a woman’s health has been determined: it is this type of virus that poses a serious threat.
However, the presence of a pathogen does not mean the presence of a disease.
In addition, HPV infection has an interesting feature: the ability to self-heal.
That is why in a situation where a certain amount of HPV type 16 DNA is detected in women during laboratory tests, it is important not to panic.
You just need to follow your doctor's recommendations and undergo regular examinations with a gynecologist.
Where does HPV type 16 come from in women?
According to WHO, up to 80% of the population is infected with HPV.
But only about 10% of those infected have clinical manifestations.
The answer to the question of how HPV 16 is transmitted to women is well known: the main route of infection is sexual contact.
Including anal-genital and oral-genital, with an infected partner.
HPV has a very high prevalence: almost 80% of women by the age of 50 have been infected at least once.
At the same time, the virus has a tendency to self-eliminate.
So it is not possible to establish the probability of infection after a single contact.
This is why it is so important not to neglect preventive measures during casual sexual acts.
Infection of a child by the mother at the time of birth is possible with viruses of types 6 and 11 - the cause of such a disease in children as respiratory papillomatosis.
No other types of virus, including HPV type 16, usually cause problems during pregnancy in either women or newborns.
There are only isolated cases of infection of newborns by mothers with bowenoid papulosis.
Therefore, routine HPV testing is not recommended by any international/national guidelines.
The incubation period varies from three months to several years.
It is possible to become infected with several types of viruses at the same time.
After entering the body, the virus infects the tissue covering the surface of the body and organs - the epithelium, namely its inner part (basal layer).
The virus inside the cell may not affect chromosomes or integrate into the genome.
The last option, the so-called. the malignant form is manifested by the appearance of cells with altered DNA, which multiply and form a tumor.
Thus, if a woman is a carrier of HPV type 16, 18, 6, 11 or others, the following conditions are possible:
- latent course of infection, when the virus does not affect cellular DNA, women have no clinical manifestations, and infection is detected only by PCR
- the appearance of such clinical manifestations as condylomas, warts, papillomas, the virus does not change the cellular genome, but provokes increased cell proliferation (the problem is detected by the presence of symptoms, PAP test, PCR method)
- the development of neoplastic changes (dysplasia), when the virus made a change in the DNA of the cell and caused corresponding changes in the latter (such changes are called koilocytosis), the situation is confirmed by PCR, PAP test, histological and colposcopic examination
- carcinoma, when the pathogen has changed the cellular genome and caused the formation of a large number of altered (“atypical”) cells – invasive cancer (the diagnosis is confirmed by PCR, Pap test, histological and colposcopic studies)
In most situations (up to 90%), the body heals from the virus within about 2 years.
The development of symptoms is observed only in 1-5% of infected people.
With regard to HPV 16, causes of severe clinical symptoms in women include:
- early onset of sexual activity
- having multiple sex partners
- multiple pregnancies/births before age 20
- smoking
- chronic cervicitis
- decreased immune defense, for example, due to concomitant HIV infection (with a normal functioning immune system, cancer in an infected woman can develop in 15-20 years, while in an HIV-infected woman - in 5-10 years, while HIV also increases the likelihood HPV infection)
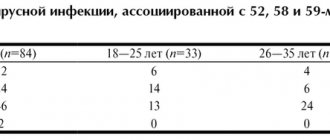
Prevalence
- 1Hapillomavirus infection is the most common sexually transmitted infection.
- 2Among the sexually active population, more than 50% are infected.
- 3The likelihood of infection with the human papillomavirus increases with the number of sexual partners.
- 4Non-genital skin warts are most common among adolescents, as well as adults working with meat products (incidence rate - 10%).
- 5 Papillomavirus most often affects women: the virus is detected in 22-35% of women and 2-35% of men. The incidence ratio among women and men is 1.4:1.
- 6Oncogenic strains cause about 5% of all cancers in the world.
Manifestations of HPV infection
In most situations, when infected with HPV in general and, in particular, HPV 16, women, as well as men, have no symptoms.
Sometimes a sign of infection can be warts and condylomas (in the case of the presence of a virus from the low-oncogenic/non-oncogenic group).
With HPV 16 infection, women may experience precancerous changes on the cervix.
This is revealed during a gynecological examination.
Or preventative, or when the patient consulted a doctor for another reason, for example, with complaints of unusual discharge.
The main diseases caused by HPV 16 are bowenoid papulosis and dysplasia of varying degrees.
With bowenoid papulosis, dense brownish, reddish or flesh-colored papules appear in the labia, pubis, inguinal and perianal areas.
They merge into large warty surfaces up to 2 cm in diameter.
The disease is characterized by a chronic, long-term course.
Malignancy develops in 3% of episodes (degenerates into squamous cell carcinoma), although self-healing is more often diagnosed.
Cervical dysplasia is a precancerous change and requires serious consideration.
Since this pathology may not be diagnosed in a timely manner due to its asymptomatic course, most countries in the world have adopted cervical cancer screening programs.
There are several classification approaches for dysplasia and cervical cancer.
They are based on the results of morphological/cytological studies (studies of cell changes).
According to the International Classification of Diseases, 10th revision, there are:
- mild dysplasia - minor proliferation and changes in epithelial cells, often a similar condition is detected during inflammatory processes in the uterine cervix and is eliminated after appropriate anti-inflammatory therapy
- moderate dysplasia - changes affect the entire lower layer of the epithelium
- severe dysplasia - the entire length of the epithelium is affected, the cell structure is noticeably changed
- cervical cancer (otherwise known as squamous cell carcinoma) – detected during colposcopic examination, confirmed cytologically and histologically
Moderate and severe dysplasia in most episodes is caused by exposure to the virus.
Signs of cervical cancer are detected only in the last stages and include:
- bleeding between menstrual periods, irregular, after sexual intercourse
- unpleasant smell of discharge
- vaginal discomfort
- pain in the pelvic area, back, legs
- weight loss
- fatigue, lack of appetite
- unilateral swelling of the legs
As the disease progresses, the severity of symptoms may increase noticeably.
Risk factors for HPV persistence and cervical cancer development
- HPV type – its carcinogenicity, or ability to cause cancer;
- immune status – people with weakened immune systems, such as people living with HIV, are more likely to have persistent HPV infections, which develop more quickly into precancer and cancer;
- co-infection with other sexually transmitted pathogens, such as herpes simplex, chlamydia and gonorrhea;
- number of births (number of children born) and early first births;
- tobacco use.
Diagnosis of HPV infection
Anogenital warts, caused by viruses type 6 and 11, are easily detected during a gynecological examination.
Identification of such formations is an indication for additional examination of the uterine cervix, and, if necessary, the urethra (urethroscopy).
The main method for detecting neoplastic changes caused by HPV is the Pap test.
It is a cytological study of smears from the uterine cervix.
In general, oncocytology is a method for detecting cancer cells in the cervix and vagina.
Samples of material for study are taken during a gynecological examination using special cyto-brushes and are absolutely painless.
A distinction is made between simple oncocytology, when the cells under study are immediately applied to slides for microscopy.
And liquid, when the cells are pre-treated with a special solution and dye.
The latter type is the PAP test.
After processing the material with two types of dyes, changes in the cell nuclei and cytoplasm are easily detected in the sample using microscopy.
The type of pathological process is preliminarily determined: inflammatory, malignant, or other.
Then, based on the severity and nature of the changes, a differential diagnosis of possible conditions is carried out.
The PAP test is included in the screening system for detecting cervical cancer in all developed countries.
Its annual holding is recommended for all females who have reached the age of 20 years.
Cytological signs of HPV infection include:
- koilocytosis - the appearance of characteristic koilocyte cells with voluminous uneven nuclei, vacuoles (absent normally) and clearing zones near the nuclei
- dyskeratocytosis - the appearance of keracite cells with dark nucleoli and characteristically altered cytoplasm
If the PAP test reveals a change in cellular structures, the following is carried out:
- colposcopic examination with acetic acid examination and test with Lugol's solution
- histological examination – small fragments of tissue are studied under a microscope (the latter are obtained by targeted biopsy)
Colposcopic signs of infection:
- lightening of areas treated with acetic acid
- uneven staining with Lugol's solution
- the presence of characteristic outgrowths (for low-oncogenic types of the virus)
According to international recommendations, diagnostic tactics for detecting disorders using the PAP test include:
- The first option is to repeat the examination after three months, in case of normality, repeat after six months and a year, in case of abnormality - colposcopic examination
- The second option is to immediately conduct a colposcopic examination; if no abnormal abnormalities are detected, cytology is repeated six months later (for oncogenic types of the virus). If necessary, a biopsy and canal curettage are performed. In a situation with insufficient reliability of colposcopic data, anti-inflammatory, estrogen therapy is recommended, followed by repeating the study
- The third option is to determine the type of virus using the hybrid capture method (the so-called Daijin test, Digene) or PCR (polymerase chain reaction). Detection of HPV type 16 or another oncogenic virus in women (the norm is the complete absence of the pathogen) is an indication for colposcopy
Typing of papillomaviruses by PCR has a high diagnostic value in terms of determining the type of virus and its belonging to a high-risk group of oncology.
Also to predict the likelihood of developing cancer against the background of existing neoplastic changes in the cervical epithelium.
Qualitative analysis produces a result in the format “there is a virus of this type / not.”
The quantitative method (real-time PCR) allows you to detect viral DNA even in very low concentrations from 10 to 100 copies in a sample.
Can be used to track the dynamics of infection.
Due to the fact that young women have a high rate of self-healing from HPV, PCR is recommended to determine the type of virus only after the age of 30.
A blood test to determine antibodies to HPV has no diagnostic value and is carried out only for research purposes.
As for the problem of preferring the Digene test or PCR, it is important to consider that the first method determines the number of HPV type 16 and other types in women from 5000 copies.
Whereas PCR “senses” a significantly lower content.
This point is significant from the point of view that this is the number that is clinically significant.
Those. More than 5,000 copies were detected against the background of neoplastic conditions - a high risk of oncology.
And detection of a smaller amount does not allow predicting the risk of developing cancer against the background of dysplasia.
In general, the analysis data allows the doctor to decide whether to start treatment or limit himself to observation.
Therapeutic measures
Considering the high risk of developing a malignant tumor at the site of HPV 16 infection, all men with a confirmed diagnosis need to be treated.
Regardless of the concentration of pathogens.
Especially if the formation is large enough and/or located in the urethra, it interferes with urination.
The exception is when small concentrations of viral DNA are detected with small papillomas.
This gives a certain chance for independent recovery.
Moreover, it is necessary to ensure regular monitoring of the condition of papilloma.
But even here, according to individual indications, the doctor may still recommend treatment.
There are three general approaches:
- removal of external manifestations of infection - viruses are also removed along with the affected cells
- conservative treatment - the use of various types of drugs and preparations, both local and systemic
- combined approach – a balanced combination of surgical and conservative components
As a rule, the best effect is achieved using the third approach.
Therefore, it is better for a man to immediately assume that he will have to be treated in at least two institutions.
Surgical profile for the stage of papilloma removal and therapeutic profile - to consolidate the achieved results.
It will also be necessary to undergo periodic examinations to ensure the effectiveness of treatment or to detect early signs of relapse.
Everything is done on an outpatient basis, without wasting time and money.
Treatment of HPV infection
Which doctor treats HPV 16 in women?
Treatment of HPV infection can be carried out by a gynecologist, oncologist, infectious disease specialist, or venereologist.
It is important to understand that accidental detection of the virus in the absence of clinical changes is not an indication for therapy.
Only if highly oncogenic viruses (HPV 16) are detected in women, the doctor decides what to do next.
Is it necessary to undergo diagnostic examinations and examinations more frequently or to prescribe additional studies?
Only a specialist can determine whether it is necessary to treat HPV 16 in women, taking into account the presence/absence of changes induced by the virus.
In a situation with HPV, it is important to trust your health only to highly professional specialists who are familiar with international protocols for managing the infection.
This is especially important when infected with HPV 16, which provokes malignant pathologies in women (reviews on the Internet or from friends will help you decide on an institution and a doctor).
Today, in women, treatment for HPV 16 is based on the removal of atypically changed epithelium.
It should be understood that if women have an infection, there are currently no drugs that destroy the virus itself.
Any international treatment regimen for HPV 16 does not include any antiviral agents.
At the same time, specific treatment for HPV 16 is carried out, in which it is recommended that women take drugs with immunomodulatory and antiviral activity.
It is believed that such drugs mobilize the immune system to fight the virus.
Such products have not been sufficiently tested for effectiveness in clinical trials.
Accordingly, there is no reliable data on the cure rate.
Despite this, many patients note a significant improvement in their well-being after using them.
Immunocorrective therapy for HPV 16 in women includes:
- with human recombinant interferon or its inducers, suppositories (Viferon, Genferon), Isoprinosine, Cycloferon, etc.
- with an immunostimulating effect - Lykopid, Polyoxidonium, etc.
- B vitamins, omega acids and dietary supplements
Often, before prescribing a drug treatment regimen, an analysis of the immune status (immunogram) is recommended.
With determination of indicators of the activity of monocytes, neutrophils, lymphocyte function, levels of immunoglobulins, CD16+, CD8+, CD4+ and others.
Unfortunately, for many drugs, data on the safety of use, complications and relapses after use have not been obtained.
Therefore, it is recommended to refrain from using them for people with:
- autoimmune diseases
- malignant formations (for cervical cancer can be prescribed only after completion of surgical treatment)
- allergic reactions
- bronchial asthma, etc.
As for the generally accepted approach to the management of HPV infection in the international medical community, the following points are positioned here:
- There is no medicine to remove the virus from the body, but the likelihood of self-healing is very high, especially at a young age
- If there are no changes in cellular structures and a virus from a high oncogenic risk group is identified, more frequent and careful monitoring of the patient is carried out
- If changes caused by the activity of the virus are detected, therapy is carried out aimed at eliminating pathological changes
For bowenoid papulosis caused by HPV type 16, tumors are removed using the following methods:
- Mohs excision
- laser therapy
- cryodestruction
- electrocoagulation
- local application of ointments with cytostatics (5-fluorourocil, prospidin, fluorofur)
- intralesional administration of interferon
- oral administration of Neotigazon capsules
Precancerous conditions and the first stages of cervical cancer are highly treatable.
The changed cells are removed using cryotherapy.
For dysplasia, organ-preserving operations are performed: conization of the cervix with a scalpel, electrosurgically, laser with preliminary canal curettage.
For localized forms of the tumor, surgical treatment is carried out, for a widespread process - radiation and chemotherapy.
Taking into account the fact that eliminating the result of virus activity does not remove the infectious agent itself.
The risk of recurrence of pathological changes remains, which, in turn, requires further monitoring of the patient.
In addition, the possibility of HPV reinfection cannot be excluded.
After implementing any treatment option, follow-up tests are recommended.
Since there is a possibility of spontaneous elimination of the virus within 2 years from the moment of infection.
A separate problem is presented by persons with HPV against the background of HIV infection.
It has been proven that the risk of developing cancer in such women is higher, as is the risk of HPV infection itself.
Although primary HPV infection was detected more often, which is associated with the greater prevalence of this virus.
Moreover, the worse the patient’s immune status, the higher the likelihood of her developing HPV-induced cancer.
Therefore, people with HIV status are recommended to undergo HPV testing more frequently.
Treatment is carried out using the same methods as for those uninfected with HIV, with additional specific therapy aimed at suppressing the activity of the immunodeficiency virus.
WHO activities
The World Health Assembly adopted a global strategy to accelerate the elimination of cervical cancer as a public health problem and its goals and targets for the period 2020–2030. (WHA73.2) (4). The global strategy sets goals to accelerate the elimination of cervical cancer:
- the threshold for elimination as a public health concern is set at 4 per 100,000 women per year;
- For countries to be on track to eliminate cervical cancer by 2030, the 90-70-90 targets below must be achieved;
- 90% of girls should be fully vaccinated against HPV by age 15;
- 70% of women should be screened with a high performance test at age 35 and again at age 45;
- 90% of women with diagnosed cervical disease should receive treatment (provide treatment for 90% of women with precancer; provide treatment for 90% of women with invasive cancer).
WHO has developed guidance and tools for preventing and controlling cervical cancer through vaccination, screening and treatment of invasive cancer, which are available in the Knowledge Repository. WHO works with countries and partners to develop and implement comprehensive programs in line with the global strategy.