Squamous cell skin cancer is a malignant tumor that consists of atypical epithelial cells that are similar in appearance to spiny keratinocytes. The disease has a tendency to quickly metastasize to lymph nodes and internal organs. The neoplasm can develop on any part of the skin, but more often - near natural openings: on the lower lip, in the genital area.
- Causes and risk factors
- Classification
- Localization options
- Clinical manifestations
- Diagnostic methods
- Treatment
- Forecast
- Prevention
Causes and risk factors
Currently, several factors have been identified that may predispose to the development of squamous cell carcinoma. These include:
- Age. The disease almost never occurs in young people. The majority of patients are elderly people over 65 years of age.
- Light skin color and presence of freckles.
- Increased insolation. The conclusion about the influence of this factor was made due to the fact that this form of malignant tumor always appears on open areas of the body that are constantly exposed to sunlight. In addition, squamous cell skin cancer can occur at the site of severe sunburn.
- Mutation of the TP53 gene, which is responsible for suppressing tumor growth.
- The presence of precancerous formations and other pathological conditions of the skin (scar atrophy, radiation damage, tuberculous lupus, occupational diseases, lichen planus, etc.).
- The effect of carcinogens on the skin (arsenic, paraffin, kerosene, coal tar, etc.), which leads to inflammation and atrophy. As a result, the formation of focal proliferations occurs, which over time can degenerate into a malignant formation.
- Prolonged mechanical irritation or damage to the skin.
- The patient is immunosuppressed.
- Infection with human papillomavirus. The role of some of its types in the occurrence of skin cancer of the penis, anus, and vulva has been proven.
- There is scientific evidence of the development of this tumor in patients with psoriasis after receiving courses of PUVA therapy and photochemotherapy, as well as in patients after radiation therapy.
Determining the cause of squamous cell skin cancer is critical to assessing the risk of recurrence and metastatic spread. Thus, a malignant tumor that developed at the site of skin lesions by actinic keratosis metastasizes only in 0.5% of cases. At the same time, cancer that occurs on the scar has a much higher risk of spreading - up to 30%.
Book a consultation 24 hours a day
+7+7+78
Papillomas on the body
Papillomas on the body can occur in the body in various forms. Their size ranges from 1 mm to several centimeters. The rashes can be single or multiple, the color ranges from white to brown.
There are three forms of manifestation of HPV:
- Clinical – papillomas, condylomas, flat formations, warts appear on the skin.
- Subclinical - the appearance of rashes that are not noticeable during a medical examination.
- Latent – there are no symptoms or manifestations. To make a diagnosis, scraping of the epithelium is necessary.
VRF is insidious. Some papillomas can develop into malignant tumors.
Classification
There are several principles for classifying squamous cell skin cancer. According to the histological structure, there are 4 types of this neoplasm, and according to TNM staging - 4 stages, each of which reflects the prevalence of the process in the body.
According to histological classification, the following options are distinguished:
- The spindle cell type has a poor prognosis due to its rapid invasive growth as well as its tendency to metastasize and recur.
- Acantholytic type. Appears on skin affected by actinic keratosis.
- Verrucous squamous cell skin cancer is accompanied by symptoms of severe hyperkeratosis, which is clinically manifested by the formation of a horny growth (skin horn).
- The lymphoepithelial type consists of poorly differentiated cells. It is believed that this neoplasm is a tumor of the skin appendages, and not true squamous cell carcinoma.
The stage of development of this type of cancer is determined by the size of the primary tumor, the degree of invasion into the underlying tissue and the presence of distant metastases. The first stage corresponds to a formation less than 2 cm in size, the second and third - larger tumors with spread to nearby tissues, and the fourth - a lesion of any size with the presence of metastatic lesions.
Localization options
Squamous cell skin cancer most often presents as a single lesion, much less often as multiple lesions. In the vast majority of cases, the skin of the face (nose, ears, periorbital area) is affected. Favorite localization is the transitions between the mucous membrane and squamous epithelium, which are observed on the red border of the lips, in the perianal region, and on the external genitalia.
In the oral cavity, this type of cancer is often located on the mucous membrane of the palate and tongue. This tumor is characterized by a long asymptomatic course. It gradually turns into a hard nodule or over time acquires the appearance of a peritonsillar abscess.
Squamous cell carcinoma on the lower lip occurs against the background of such precancerous formations as leukoplakia, actinic and abrasive cheilitis. Initially, it appears as tightly fitting scales, under which a small growing compaction forms. Less commonly, the disease begins with erosion, which has a dense base. As the tumor grows, the lip may become deformed or thicken.
For localization of cancer in the vulva area, localization is characteristic of the transitional fold of the labia majora and minora, and the clitoris. The disease has an unfavorable prognosis and is characterized by rapid metastasis. The formation of squamous cell skin cancer of this localization may be preceded by lichen sclerosus, Bowen's disease, and erythroplakia.
Penile skin cancer usually occurs in men over 40 years of age. Its typical location is the posterior surface of the body of the penis, the area of the preputial sac and coronary sulcus. Predisposing factors to the formation of this tumor are chronic inflammatory processes, balanitis with congenital phimosis, and accumulation of smegma. This is why penile cancer almost never occurs in men who have undergone circumcision.
Symptoms
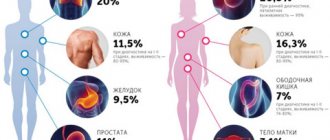
Squamous cell carcinoma can start anywhere where squamous (flat) cells are found, but most often affects a person's skin:
- face, ears, scalp (55%),
- back of hands (18%),
- legs (13%).
When cancer grows deep into tissues ( endophytic
growth form), it usually begins as a spot on the skin, which may resemble a normal pigmented one. After some time (usually we are talking about several months), the spot transforms into a dense, motionless nodule, and then (after about another six months) its surface begins to ulcerate and rapidly grow into deep tissues. You should be alerted to any non-healing cracks, erosions, or ulcers.
If the tumor grows above the surface of the tissue or into the lumen of an organ ( exophytic
growth form), it may resemble a cauliflower or a mushroom. Germination into the deep layers of the skin or surrounding tissues also occurs, so the base of the tumor will be inactive. There are frequent cases of cancer from papillomas, and over time, malignant papillomas turn into ulcers.
If the tumor is localized in the larynx, trachea, in the wall of the esophagus or intestines, in the cervix, vulva or anal canal, then symptoms may include problems with breathing/swallowing/going to the toilet, a feeling of the presence of a foreign body, pain, weakness, nausea, bleeding , the appearance of an unpleasant odor, enlarged lymph nodes.
When is it time to see an oncologist?
If you find yourself with a scaly area, or ulcer, skin growth, scab, problems with swallowing, or other unpleasant symptoms that do not go away on their own within 2 months, definitely do not wait any longer. This is already a reason to put things aside and urgently contact an oncologist
.
Residents of St. Petersburg or the Leningrad region have the opportunity to make an appointment with a medical oncologist, as well as call a doctor to their home at a place and time convenient for them. Phones:
+7 (812) 323‑07‑49 and +7 (921) 932‑14‑79
(Mon-Fri 9.00 - 21.00; Sat-Sun 10.00 - 18.00).
Clinical manifestations
There are two forms of growth of squamous cell carcinoma: exophytic and endophytic. Each of them is characterized by certain clinical manifestations.
Exophytic (papillary) form
The primary nodule in this type of tumor gradually increases in size and rises above the skin level. A large amount of horny mass accumulates on the surface of the lesion. Over time, its color becomes red or brownish with a large number of dilated vessels on the surface (telangiectasia). Sometimes retraction is detected in the center of formation.
The base of the neoplasm is wide. The lesion itself and the surrounding tissues are inactive due to tumor growth. In later stages, necrosis and ulceration occur.
A type of exophytic squamous cell skin cancer is its verrucous form, which is characterized by a yellow or red-brown color of the lesion, an uneven surface with warty growths. This type of tumor, in turn, also has several clinical variants depending on the location:
- Oral papillomatosis - neoplasms on the mucous membrane of the tongue, cheeks, and gums. Usually seen in people who chew tobacco.
- Anogenital carcinoma. It is located on the skin of the glans penis, scrotum, vulva, and perianal area.
- The plantar type is typical for older men.
- Squamous cell verrucous cancer of other areas of the skin (extremities, torso).
The verrucous form is characterized by slow growth and a low risk of metastasis. On the skin, this type of cancer forms most often in places that are subject to constant mechanical stress and may have the appearance of a cutaneous horn.
Book a consultation 24 hours a day
+7+7+78
Endophytic (ulcerative-infiltrative) form
With endophytic tumor growth, the primary element is a nodule, which over time turns into a dense node. The lesion is closely fused with the underlying tissues. After a few months, it ulcerates. The ulcer has an irregular shape, a dense bottom, a whitish film on the surface and crater-shaped edges. It may be covered with a brownish crust, which, when removed, releases a bloody exudate. The ulcer increases in depth and to the sides, quickly spreading to the underlying tissue. This form of squamous cell skin cancer is characterized by frequent recurrence and the formation of metastases.
Stages of squamous cell skin cancer
The incidence of local metastases is 2-6%. Metastasis from SCC of the forehead, temples, eyelids, cheeks and ears occurs in the lymph nodes near the salivary glands, from the lips and perioral region - in the submental and submandibular (upper cervical) lymph nodes.
Conjunctival RCC
A special form of this tumor is SCC of the conjunctiva of the eye, which manifests itself as a chronic, unilateral, limited area of redness or diffuse conjunctivitis. It can also be in the form of a formation on the inner corner of the eye in the commissure between the eyelids or as a formation with a terry red or flat white surface.
Diagnostics
For diagnosis, as with any other skin tumor, a biopsy must be performed. The type of biopsy depends on the size of the formation. For most tumors, this can be done on an outpatient basis under local anesthesia.
Diagnostic methods
Since the direct dependence of the effectiveness of the treatment on the stage of the malignant neoplasm at which it was discovered has long been proven, there are two levels of diagnosis of squamous cell skin cancer: early and late.
An early diagnosis is considered to be made at stages I-II. In this case, complete recovery of the patient is possible, provided that the correct treatment tactics are chosen. Late detection means diagnosis at stages III and IV. The prognosis is usually unfavorable due to the complexity or impossibility of surgical treatment.
The “gold standard” for diagnosing squamous cell skin cancer is a biopsy followed by histological examination. The immunohistochemical method is considered especially informative. Since the tumor is external and it is not difficult to obtain biomaterial for histology, the tumor is verified in 99% of cases.
The dermatoscopy method is also widely used. In this case, the presence of central keratin plugs, dilated and branched vessels on the surface speaks in favor of skin cancer.
For any form of squamous cell carcinoma, along with a thorough history and physical examination, a specialist must evaluate the condition of the lymph nodes. If the presence of metastatic foci is suspected, the main diagnostic method is fine-needle aspiration. It is also possible to prescribe additional imaging methods (ultrasound, radiography, CT, angiography) to identify regional and distant metastases.
Treatment
Today, there are many ways to help patients with squamous cell skin cancer. These include both classical methods (removal with a scalpel, cryodestruction, laser therapy) and modern technologies, for example, photodynamic therapy.
Surgical removal
Surgical treatment consists of removing the tumor with an indentation of 1-2 cm towards healthy tissue. Surgical excision is indicated for low-risk skin cancer and a low probability of tumor recurrence.
Low risk criteria:
- Localization of cancer in open areas of the body (excluding lips and ears).
- Size up to 2 cm.
- There is no invasion into the dermis.
- Highly differentiated tumor.
- The immune status is normal.
Surgical treatment is not used in the following cases:
- High-risk squamous cell skin cancer (localized on the lips, ears, closed areas; development against the background of precancer; large tumor).
- Multiple metastases.
- Increased operational risk (drug intolerance, advanced age of the patient).
- Localization in which complete removal of the lesion is impossible (periorbital region, nose).
Surgical removal of cancer in the early stages in a large percentage of cases leads to the patient’s recovery. However, the disadvantage of this method is that it is not always possible to achieve a satisfactory aesthetic and functional result.
An effective option for surgical treatment of squamous cell skin cancer is the Mosch operation, during which the tumor is removed layer by layer with immediate histological examination of each layer. This approach allows for maximum preservation of healthy tissue.
Surgical removal according to Mosch can be used for high-risk skin cancer, multiple lesions, and tumor localization in cosmetically important areas. However, applying this method requires a lot of time and money.
Small tumors can be removed using curettage or electrocoagulation, including 5-6 mm of healthy skin. These methods are simple, but long-term results are disappointing: the risk of cancer recurrence is high.
Cryodestruction
For squamous cell skin cancer, cryodestruction is carried out in several cycles. Depending on the location and clinical signs of the lesion, the exposure time is selected. The procedure is performed by capturing 2-2.5 cm of healthy skin around the tumor. Removal using cryodestruction is possible only for low-risk tumors.
This method is good because it can be performed on an outpatient basis. In addition, it is characterized by low pain. The main disadvantage is the impossibility of histological control.
Laser therapy
This type of treatment uses a carbon or neodymium laser. The use of this method leads to good cosmetic results.
Laser therapy is indicated for patients who suffer from bleeding disorders or are taking anticoagulants. The disadvantages of this method are limited indications (can only be used for low-risk cancer) and the lack of the possibility of histological examination of a remote lesion.
Radiation therapy
Due to the fact that squamous cell skin cancer is a tumor with a relatively high sensitivity to radiation therapy, it is widely used as monotherapy and in combination with other methods. Small lesions are treated using close-focus X-ray radiation, large tumors without metastasis are treated with external gamma therapy. In the presence of regional metastases, combined treatment is performed, which includes the use of preoperative radiation therapy and excision of the formation along with the affected lymph nodes.
At the first and second stages of skin cancer, this method can be used as an independent method, at the third and fourth stages it can be used as pre- and postoperative treatment. For inoperable forms, it is an option for palliative care for patients.
The use of radiation therapy is contraindicated for recurrent cancer, verrucous carcinoma, connective tissue diseases (scleroderma, lupus erythematosus). Negative consequences of the method may be the development of periostitis, perichondritis, cataracts, and serious cicatricial deformities on the skin.
Book a consultation 24 hours a day
+7+7+78
Chemotherapy
Local and systemic chemotherapy can be used to treat squamous cell carcinoma. Fluorouracil, prospidin, and glyciphone ointments are used as local remedies. It should be noted that this type of therapy is rather low in effectiveness, and the risk of tumor recurrence with external treatment is high. In addition, such ointments can cause intoxication, which interferes with healing.
Also, cytostatic drugs (5-fluorouracil) are introduced into the lesion using intradermal or subcutaneous injections. Systemic chemotherapy with cisplatin, bleomycin, carboplatin is used in the presence of inoperable formation, metastatic tumor, or as preoperative preparation.
Thus, the indications for chemotherapy are:
- Recurrent skin cancer.
- Multiple lesions.
- Impossibility of surgical removal.
- Metastatic tumor.
- Squamous cell skin cancer in elderly patients who have contraindications to the use of other methods.
The use of cytotoxic drugs is contraindicated in case of severe concomitant pathology. This method is also not suitable for treating weakened patients with immunodeficiency conditions.
Interferon therapy
Local and systemic immunomodulators can be used to treat skin cancer. These include: imiquimod (cream), Viferon, intron A.
The indication for using the method is the presence of a large inoperable tumor. Treatment with interferons is contraindicated for autoimmune diseases, leukopenia, severe concomitant diseases in the stage of decompensation.
The frequent development of side symptoms is a significant drawback of immunomodulator therapy. In addition, the cost of the course of treatment is quite high with its relatively low effectiveness.
Photodynamic therapy
This method is a modern minimally invasive method for treating squamous cell skin cancer. It is based on the introduction of a photosensitizer into the body, followed by irradiation with a laser with a certain wavelength, resulting in the destruction of tumor cell membranes without damaging healthy tissue.
The photosensitizer can be administered systemically (intravenously, orally) or locally (by application). As a rule, the intravenous route of administration is used. Our clinic uses the drug Photoditazine.
Indications for systemic photodynamic therapy:
- Initial stages of squamous cell carcinoma without tissue invasion.
- Resistance to standard treatments.
- Severe concomitant pathology, which makes surgery impossible.
- Hard-to-reach localization of formation.
- Multiple and recurrent skin cancer.
Among the local photosensitizers, methylaminolevulinic acid (MALA) in the form of a cream is the most effective. When using this product, the cosmetic result is more acceptable than with surgical excision and cryodestruction.
Onko LEGO - tissue atypia
“If you are in a hurry to build a universe or a house, you will almost certainly notice later that you forgot to make a shallow place or a closet for brushes.” Mark Twain
Global changes in tumor tissue are noted during visual analysis. This is how the morphological atypism of the tumor manifests itself, consisting of cellular and tissue atypia.
Tissue is a collection of cells and non-cellular structures. Tissue atypia is manifested by the structural and functional restructuring of two interconnected tissue components - parenchyma (functional part) and stroma (connective tissue framework) [1].
Isolated tissue atypia is observed in mature, benign tumors. Its signs are determined by the histogenesis of the neoplasm. So, we have before us a benign non-melanocytic tumor of epithelial tissue - papilloma. Tumor elements “stand out” from the normal histological picture and draw the pathologist’s attention to themselves. In papilloma such “labels” are:
- papillary structure;
- excessive function of the villous epithelium (for example, during trauma, hyperkeratosis is observed in skin papillomas);
- submersible expansive growth of the epithelium at the base of the tumor (due to the proliferation of cells of the spinous layer - acanthosis) [2].
Also, most benign epithelial neoplasms are characterized by the presence of a clear boundary between the parenchyma and stroma. Papillomas under microscopy look like pictures with a clear, as if outlined outline: a darker colored epithelial component and a light fibrovascular stroma (when stained with hematoxylin and eosin) (Fig. 1) [3]. .
Figure 1 | Squamous cell papilloma of the skin
The tumor is covered with unevenly thickened mature stratified keratinizing epithelium, with hyperkeratosis (bright pink thickened stratum corneum), acanthosis (proliferation of cells of the spinous layer, with an increase in the number of rows, immersion of the epithelial papillae into the papillary layer of the dermis) [3].
Even benign neoplasms can lead to gross deformation of the organ. Indicative in this regard are leiomyomas - benign tumors of smooth muscle tissue. In the uterus, such tumor nodes sometimes reach gigantic sizes. Microscopically, simple (non-proliferating) leiomyomas (the term myomas are often used) are represented by a parenchymal component of well-defined bundles of hypertrophied smooth muscle cells, and a stromal (connective tissue) component - the extracellular matrix (Fig. 2) [4]. .
Figure 2 | Histological pattern of leiomyoma
Multidirectional bundles of spindle-shaped smooth muscle cells with elongated “cigar-shaped” nuclei [4]
The nodes do not have a true capsule of tumor tissue itself. Their clear boundaries are formed by compressed (compressed) myometrium, in which flattened smooth muscle elements are intertwined with a large number of collagen fibers due to activation of fibroblasts under ischemic conditions. Cellular atypia, including pathological mitoses, is not found in simple leiomyomas. If 5 or more mitotic figures are detected per 10 HPFs (High Power Fields), the neoplasm is assessed as a mitotically active (cellular, proliferating) leiomyoma (Fig. 3) [5]. .
Figure 3 | Microscopic picture of smooth muscle tumors
A, B: benign neoplasm - leiomyoma; C, D: malignant neoplasm - leiomyosarcoma [5].
But still the component of myomatous nodes is heterogeneous. The tumor node lives its life, changing its morphology as well. In “young” myomatous nodes, which are small in size, the nuclei of myocytes are large in size and ellipsoidal in shape; in “old” nodes with a large diameter, the nuclei are smaller and rod-shaped. Also, “with age,” the amount of connective tissue increases. Fibrous fibers seem to entwine smooth muscle cells, and in their tenacious embrace the myocytes undergo atrophy. Ischemic disorders in the nodes can lead to various forms of degeneration, hyaline, cystic, myxoid, hemorrhagic, as well as calcification, with natural changes in the morphological picture (Fig. 4) [6].
Figure 4 | Degenerative changes in leiomyoma
(a) hyaline type of degeneration; (b) calcification; (c) cystic degeneration; (d) “red” or hemorrhagic degeneration [6].
Hyalinosis is most often observed, with initial changes in the form of hyalinization of the stroma, with further replacement of smooth muscle cells of the tumor node by hyaline. With severe edema, the formation of cystic cavities of various sizes is possible. Rarely, the myxoid type is found, in which the cavities contain a mucopolysaccharide-rich substance that accumulates contrast agent on magnetic resonance imaging, in contrast to the contents of the cystic cavities. Red or hemorrhagic degeneration occurs as a result of hemorrhagic infarction of the tumor stroma (for example, caused by venous thrombosis or occlusion of intratumoral arteries).
A component of tissue atypism is vascular pathology. In proliferating leiomyomas, rapid new formation of sinusoidal vessels is observed. Around the vessels, areas of myocyte proliferation—growth zones—are formed, often along the periphery of existing nodes [7].
An evolutionarily thoughtful balance of tissue components ensures the functioning of the organ and its beautiful, harmonious macro- and microscopic appearance. The tumor disrupts this harmonious system, like a mad architect building bizarre, often ugly structures, demanding more and more “financing” and “workers”.
Sources:
1. Linder N. et al. Identification of tumor epithelium and stroma in tissue microarrays using texture analysis. Diagnosis Pathol. 2012;7:22. 2. Furue M. Epithelial tumor, invasion and stroma. Ann Dermatol. 2011;23(2):125–131. 3. Image courtesy of the Pathorama electronic database; 4. Shankar VS Leiomyoma: uterus. Female Genital System & Breast, Practical Pathology, Slides, Systemic Pathology. 2016. 5. Hoffman BL; et al. Williams Gynecology. 3rd edn. McGraw-Hill.2016. 6. Geethamala K, Murthy VS, Vani BR, Rao S. Uterine Leiomyomas: An ENIGMA. J Midlife Health. 2016;7(1):22–27. 7. Devereaux KA, Schoolmeester JK Smooth Muscle Tumors of the Female Genital Tract. Surg Pathol Clin. 2019;12(2):397-455.
Forecast
When squamous cell skin cancer measuring less than 2 cm is detected and adequate treatment is provided, the 5-year survival rate reaches 90%. If the tumor is larger and there is growth into the tissue, then this figure is reduced to 50%.
Tumors located on the skin of the periorbital region, external auditory canal, and nasolabial fold have a particularly unfavorable prognosis. With this localization, the tumor can grow into muscles and bones and can cause bleeding due to vascular damage, complicated by infections.
Prevention
The main measure for preventing squamous cell skin cancer is the timely detection and treatment of precancerous conditions. In this regard, young people are recommended to be examined by a dermatologist every 3 years, and people over 40 years old - every year. If you detect any changes in the skin, you should also contact a specialist.
Foci of chronic inflammation on the skin must undergo adequate sanitation. You should also avoid repeated damage to the same skin area (rubbing, compression by tight clothing and shoes, injury during monotonous manual work).
It is important to maintain a sun regime and use a cream with a sunscreen component, and avoid visiting a solarium. When working with chemical reagents that are sources of occupational hazard, it is necessary to use personal skin protection.
Book a consultation 24 hours a day
+7+7+78